You can now order all kinds of medical tests online. Our research shows this is (mostly) a bad idea
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.

Many of us have done countless rapid antigen tests (RATs) over the course of the pandemic. Testing ourselves at home has become second nature.
But there’s also a growing worldwide market in medical tests sold online directly to the public. These are “direct-to-consumer” tests, and you can access them without seeing a doctor.
While this might sound convenient, the benefits to most consumers are questionable, as we discovered in a recent study.
What are direct-to-consumer tests?
Let’s start with what they’re not. We’re not talking about patients who are diagnosed with a condition, and use tests to monitor themselves (for example, finger-prick testing to monitor blood sugar levels for people with diabetes).
We’re also not talking about home testing kits used for population screening, such as RATs for COVID, or the “poo tests” sent to people aged 50 and over for bowel cancer screening.
Direct-to-consumer tests are products marketed to anyone who is willing to pay, without going through their GP. They can include hormone profiling tests, tests for thyroid disease and food sensitivity tests, among many others.
Some direct-to-consumer tests allow you to complete the test at home, while self-collected lab tests give you the equipment to collect a sample, which you then send to a lab. You can now also buy pathology requests for a lab directly from a company without seeing a doctor.

Ground Picture/Shutterstock
What we did in our study
We searched (via Google) for direct-to-consumer products advertised for sale online in Australia between June and December 2021. We then assessed whether each test was likely to provide benefits to those who use them based on scientific literature published about the tests, and any recommendations either for or against their use from professional medical organisations.
We identified 103 types of tests and 484 individual products ranging in price from A$12.99 to A$1,947.
We concluded only 11% of these tests were likely to benefit most consumers. These included tests for STIs, where social stigma can sometimes discourage people from testing at a clinic.
A further 31% could possibly benefit a person, if they were at higher risk. For example, if a person had symptoms of thyroid disease, a test may benefit them. But the Royal Australian College of General Practitioners does not recommend testing for thyroid disease in people without symptoms because evidence showing benefits of identifying and treating people with early thyroid disease is lacking.
Some 42% were commercial “health checks” such as hormone and nutritional status tests. Although these are legitimate tests – they may be ordered by a doctor in certain circumstances, or be used in research – they have limited usefulness for consumers.
A test of your hormone or vitamin levels at a particular time can’t do much to help you improve your health, especially because test results change depending on the time of day, month or season you test.
Most worryingly, 17% of the tests were outright “quackery” that wouldn’t be recommended by any mainstream health practitioner. For example, hair analysis for assessing food allergies is unproven and can lead to misdiagnosis and ineffective treatments.
More than half of the tests we looked at didn’t state they offered a pre- or post-test consultation.

fizkes/Shutterstock
Products available may change outside the time frame of our study, and direct-to-consumer tests not promoted or directly purchasable online, such as those offered in pharmacies or by commercial health clinics, were not included.
But in Australia, ours is the first and only study we know of mapping the scale and variety of direct-to-consumer tests sold online.
Research from other countries has similarly found a lack of evidence to support the majority of direct-to-consumer tests.
4 questions to ask before you buy a test online
Many direct-to-consumer tests offer limited benefits, and could even lead to harms. Here are four questions you should ask yourself if you’re considering buying a medical test online.
1. If I do this test, could I end up with extra medical appointments or treatments I don’t need?
Doing a test yourself might seem harmless (it’s just information, after all), but unnecessary tests often find issues that would never have caused you problems.
For example, someone taking a diabetes test may find moderately high blood sugar levels see them labelled as “pre-diabetic”. However, this diagnosis has been controversial, regarded by many as making patients out of healthy people, a large number of whom won’t go on to develop diabetes.
2. Would my GP recommend this test?
If you have worrying symptoms or risk factors, your GP can recommend the best tests for you. Tests your GP orders are more likely to be covered by Medicare, so will cost you a lot less than a direct-to-consumer test.
3. Is this a good quality test?
A good quality home self-testing kit should indicate high sensitivity (the proportion of true cases that will be accurately detected) and high specificity (the proportion of people who don’t have the disease who will be accurately ruled out). These figures should ideally be in the high 90s, and clearly printed on the product packaging.
For tests analysed in a lab, check if the lab is accredited by the National Association of Testing Authorities. Avoid tests sent to overseas labs, where Australian regulators can’t control the quality, or the protection of your sample or personal health information.
4. Do I really need this test?
There are lots of reasons to want information from a test, like peace of mind, or just curiosity. But unless you have clear symptoms and risk factors, you’re probably testing yourself unnecessarily and wasting your money.
Direct-to-consumer tests might seem like a good idea, but in most cases, you’d be better off letting sleeping dogs lie if you feel well, or going to your GP if you have concerns.
Patti Shih, Senior Lecturer, Australian Centre for Health Engagement, Evidence and Values, University of Wollongong; Fiona Stanaway, Associate Professor in Clinical Epidemiology, University of Sydney; Katy Bell, Associate Professor in Clinical Epidemiology, Sydney School of Public Health, University of Sydney, and Stacy Carter, Professor and Director, Australian Centre for Health Engagement, Evidence and Values, University of Wollongong
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
8 Signs On Your Breast You Shouldn’t Ignore
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Can you name the 8 signs that may indicate breast cancer? This video discusses them, and also shows what they look like on various different skintones:
Stay abreast:
Dr Simi Adedeji bids us watch out for:
- Inverted nipple: a newly inverted nipple (pointing inward or folded) should be checked by a doctor, especially if it’s a recent change.
- Flaky rash: a flaky, itchy, or red rash around the nipple or areola could indicate an underlying issue and should not be dismissed as just a skin condition.
- Tethering: skin pulling or denting, noticeable when raising your arms, may signal a deeper problem.
- Dimpling: skin resembling an orange peel (po orang sign) with dips and accentuated pores could indicate swelling or thickening and requires medical evaluation.
- Redness or heat: unusual warmth, redness, or tenderness in the breast, particularly if not breastfeeding, should be investigated.
- Nipple discharge: any unusual fluid from the nipple (be it yellow, green, milky, clear, or blood-stained) warrants attention, especially if spontaneous or only from one side.
- Change in size: sudden changes in the size or shape of one breast should not be ignored.
- Breast lump: a firm, irregular, or persistent lump in the breast, armpit, or collarbone area should be checked promptly, even if it’s not always harmful.
The above signs may indicate cancer or something else, but none of them are things that should be ignored (even if you get just one sign).
For more on each of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
The Hormone Therapy That Reduces Breast Cancer Risk & More
Take care!
Share This Post
-
Deskbound – by Kelly Starrett and Glen Cordoza
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve all heard that “sitting is the new smoking”, and whether or not that’s an exaggeration (the jury’s out), one thing that is clear is that sitting is very bad.
Popular advice is “here’s how to sit with good posture and stretch your neck sometimes”… but that advice tends to come from companies that pay people to sit for a long time. They might not be the a very unbiased source.
Starrett and Cordoza offer better. After one opening chapter covering the multifarious ways sitting ruins our health, the rest of the book is all advice, covering:
- The principles of how the body is supposed to be
- The most important movements that we should be doing
- A dynamic workstation setup
- This is great, because “get a standing desk” tends to present more questions than answers, and can cause as much harm as good if done wrong
- The authors also cover how to progressively cut down on sitting, rather than try to go cold-turkey.
- They also recognize that not everyone can stand at all, and…
- Optimizing the sitting position, for when we must sit
- Exercises to maintain our general mobility and compensate about as well as we can for the body-unfriendly nature of modern life.
The book is mostly explanations, so at 682 pages, you can imagine it’s not just “get up, lazybones!”. Rather, things are explained in such detail (and with many high-quality medical diagrams) so that we can truly understand them.
Most of us have gone through life knowing we should have “better posture” and “move more”… but without the details, that can be hard to execute correctly, and worse, we can even sabotage our bodies unknowingly with incorrect form.
This book straightens all that out very comprehensively, and we highly recommend it.
Share This Post
-
The Vagus Nerve’s Power for Weight Loss
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Arun Dhir is a university lecturer, a gastrointestinal surgeon, an author, and a yoga and meditation instructor, and he has this to say:
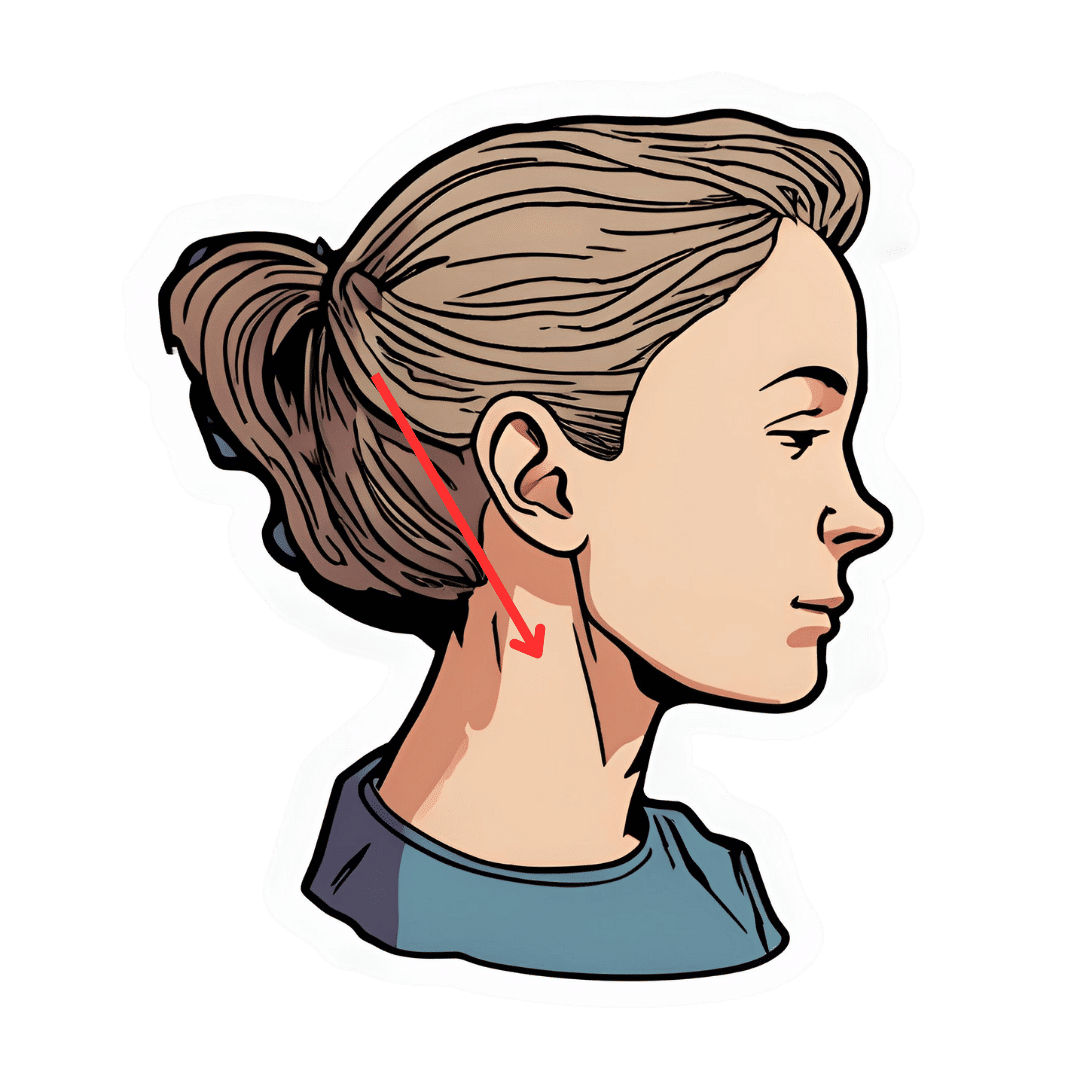
Gut feelings
The vagus nerve is the 10th cranial nerve, also known as “vagus” (“the wanderer”), because it travels from the brain to many other body parts, including the ears, throat, heart, respiratory system, gut, pancreas, liver, and reproductive system. It’s no surprise then, that it plays a key role in brain-gut communication and metabolism regulation.
The vagus nerve is part of the parasympathetic nervous system, responsible for rest, digestion, and counteracting the stress response. Most signals through the vagus nerve travel from the gut to the brain, though there is communication in both directions.
You may be beginning to see how this works and its implications for weight management: the vagus nerve senses metabolites from the liver, pancreas, and small intestine, and regulates insulin production by stimulating beta cells in the pancreas, which is important for avoiding/managing insulin resistance and metabolic syndrome in general.
Dr. Dhir cites a study in which vagus nerve stimulation (originally used for treating epilepsy and depression) was shown to cause unintentional weight loss (6-11%) in patients, revealing a link to weight management. Of course, that is quite a specific sample, so more research is needed to say for sure, but because the principle is very sound and the mechanism of action is clear, it’s not being viewed as a controversial conclusion.
As for how get these benefits, here are seven ways:
- Cold water on the face: submerge your face in cold water in the morning while holding water in your mouth, or cover your face with a cold wet washcloth (while holding your breath please; no need to waterboard yourself!), which activates the “mammalian dive response” in which your body activates the parasympathetic nervous system in order to remain calm and thus survive for longer underwater
- Alternate hot and cold showers: switch between hot and cold water during showers for 10-second intervals; this creates eustress and activates the process of hormesis, improving your overall stress management and reducing any chronic stress response you may otherwise have going on
- Humming and gargling: the vibrations in the throat stimulate the nearby vagus nerve
- Deep breathing (pranayama): yoga breathing exercises, especially combined with somatic exercises such as the sun salutation, can stimulate the vagus nerve
- Intermittent fasting: helps recalibrate the metabolism and indirectly improves vagus nerve function
- Massage and acupressure: stimulates lymphatic channels and the vagus nerve
- Long walks in nature (“forest bathing”): helps trigger relaxation in general
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
The Vagus Nerve (And How You Can Make Use Of It)
Take care!
Share This Post
Related Posts
-
Cordyceps: Friend Or Foe?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cordyceps: friend or foe?
Cordyceps is a famously frightening fungus. It’s the one responsible for “zombie ants” and other zombie creatures, and it’s the basis for the existential threat to humanity in the TV show The Last of Us.
It’s a parasitic fungus that controls the central and peripheral nervous systems of its host, slowly replacing the host’s body, as well as growing distinctive spines that erupt out of the host’s body. Taking over motor functions, it compels the host to do two main things, which are to eat more food, and climb to a position that will be good to release spores from.
Fortunately, none of that matters to humans. Cordyceps does not (unlike in the TV show) affect humans that way.
What does Cordyceps do in humans?
Cordyceps (in various strains) is enjoyed as a health supplement, based on a long history of use in Traditional Chinese Medicine, and nowadays it’s coming under a scientific spotlight too.
The main health claims for it are:
- Against inflammation
- Against aging
- Against cancer
- For blood sugar management
- For heart health
- For exercise performance
Sounds great! What does the science say?
There’s a lot more science for the first three (which are all closely related to each other, and often overlapping in mechanism and effect).
So let’s take a look:
Against inflammation
The science looks promising for this, but studies so far have either been in vitro (cell cultures in petri dishes), or else murine in vivo (mouse studies), for example:
- Anti-inflammatory effects of Cordyceps mycelium in murine macrophages
- Cordyceps sinensis as an immunomodulatory agent
- Immunomodulatory functions of extracts from Cordyceps cicadae
- Cordyceps pruinosa inhibits in vitro and in vivo inflammatory mediators
In summary: we can see that it has anti-inflammatory properties for mice and in the lab; we’d love to see the results of studies done on humans, though. Also, while it has anti-inflammatory properties, it performed less well than commonly-prescribed anti-inflammatory drugs, for example:
❝C. militaris can modulate airway inflammation in asthma, but it is less effective than prednisolone or montelukast.❞
Against aging
Because examining the anti-aging effects of a substance requires measuring lifespans and repeating the experiment, anti-aging studies do not tend to be done on humans, because they would take lifetimes to perform. To this end, it’s inconvenient, but not a criticism of Cordyceps, that studies have been either mouse studies (short lifespan, mammals like us) or fruit fly studies (very short lifespan, genetically surprisingly similar to us).
The studies have had positive results, with typical lifespan extensions of 15–20%:
- The lifespan-extending effect of Cordyceps sinensis in normal mice
- Cordyceps sinensis oral liquid prolongs the lifespan of the fruit fly, Drosophila melanogaster
- Anti-aging activity of polysaccharides from Cordyceps militaris
- Anti-aging effect of Cordyceps sinensis extract
Against cancer
Once again, the studies here have been in vitro, or murine in vivo. They do look good though:
In vitro (human cell cultures in a lab):
In vivo (mouse studies):
Summary of these is: Cordyceps quite reliably inhibits tumor growth in vitro (human cell cultures) and in vivo (mouse studies). However, trials in human cancer patients are so far conspicuous by their absence.
For blood sugar management
Cordyceps appears to mimic the action of insulin, without triggering insulin sensitivity. For example:
The anti-hyperglycemic activity of the fruiting body of Cordyceps in diabetic rats
There were some other rat/mouse studies with similar results. No studies in humans yet.
For heart health
Cordyceps contains adenosine. You may remember that caffeine owes part of its stimulant effect to blocking adenosine, the hormone that makes us feel sleepy. So in this way, Cordyceps partially does the opposite of what caffeine does, and may be useful against arrhythmia:
Cardiovascular protection of Cordyceps sinensis act partially via adenosine receptors
For exercise performance
A small (30 elderly participants) study found that Cordyceps supplementation improved VO2 max by 7% over the course of six weeks:
However, another small study (22 young athletes) failed to reproduce those results:
Cordyceps Sinensis supplementation does not improve endurance exercise performance
In summary…
Cordyceps almost certainly has anti-inflammation, anti-aging, and anti-cancer benefits.
Cordyceps may have other benefits too, but the evidence is thinner on the ground for those, so far.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Mango vs Papaya – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing mango to papaya, we picked the mango.
Why?
Both are great! But there are some things to set them apart:
In terms of macros, this one’s not so big of a difference. They are equal in fiber, while mango has more protein and slightly more carbs. They are both low glycemic index, so we’ll call this one a tie, or the slenderest nominal win for papaya.
When it comes to vitamins, mango has more of vitamins A, B1, B3, B5, B7, B9, E, K, and choline, while papaya has more vitamin C. However, a cup of mango already gives the RDA of vitamin C, so at this point, it’s not even really much of a bonus that papaya has more. In any case, a clear and overwhelming win in the vitamins category for mango.
As for minerals, this one’s closer; mango has more copper, manganese, phosphorus, and zinc, while papaya has more calcium, iron, and magnesium. Still, a 4:3 win for mango.
Adding these up makes for a clear win for mango. However, one extra thing to bear in mind about both:
Both of these fruits interact with warfarin and many other anticoagulants. So if you’re taking those, you might want to skip these, or at least consult with your doctor/pharmacist for input on your personal situation.
Aside from that; enjoy both; diversity is good! But mango is the more nutritionally dense, and thus the winner here.
Want to learn more?
You might like to read:
5 Ways To Make Your Smoothie Blood Sugar Friendly (Avoid the Spike!)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Apples vs Bananas – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing apples to bananas, we picked the bananas.
Why?
Both apples and bananas contain lots of vitamins, but bananas contain far more of Vitamins A, B, and C.
Apples beat bananas only for vitamins E and K.
This may seem like “well that’s 2 vs 3; that’s pretty close” until one remembers that vitamin B is actually eight vitamins in a trenchcoat. Bananas have more of vitamins B1, B2, B3, B5, B6, and B9.
If you’re wondering about the other numbers: neither fruit contains vitamins B7 (biotin) or B12 (cobalamins of various kinds). Vitamins B4, B8, B10, and B11 do not exist as such (due to changes in how vitamins are classified).
Both apples and bananas contain lots of minerals, but bananas contain far more of iron, magnesium, phosphorus, potassium, zinc, copper, manganese, and selenium.
Apples beat bananas only for calcium (and then, only very marginally)
Both apples and bananas have plenty of fiber.
Apples have marginally less sugar, but given the fiber content, this is pretty much moot when it comes to health considerations, and apples are higher in fructose in any case.
In short, both are wonderful fruits (and we encourage you to enjoy both!), and/but bananas beat apples healthwise in almost all measures.
PS: top tip if you find it challenging to get bananas at the right level of ripeness for eating… Try sun-dried! Not those hard chip kinds (those are mechanically and/or chemically dried, and usually have added sugar and preservatives), but sun-dried.
Here’s an example product on Amazon
Warning: since there aren’t many sun-dried bananas available on Amazon, double-check you haven’t been redirected to mechanically/chemically dried ones, as Amazon will try that sometimes!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: