Yes, you do need to clean your tongue. Here’s how and why
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Has your doctor asked you to stick out your tongue and say “aaah”? While the GP assesses your throat, they’re also checking out your tongue, which can reveal a lot about your health.
The doctor will look for any changes in the tongue’s surface or how it moves. This can indicate issues in the mouth itself, as well as the state of your overall health and immunity.
But there’s no need to wait for a trip to the doctor. Cleaning your tongue twice a day can help you check how your tongue looks and feels – and improve your breath.

What does a healthy tongue look like?
Our tongue plays a crucial role in eating, talking and other vital functions. It is not a single muscle but rather a muscular organ, made up of eight muscle pairs that help it move.
The surface of the tongue is covered by tiny bumps that can be seen and felt, called papillae, giving it a rough surface.
These are sometimes mistaken for taste buds – they’re not. Of your 200,000-300,000 papillae, only a small fraction contain taste buds. Adults have up to 10,000 taste buds and they are invisible to the naked eye, concentrated mainly on the tip, sides and back of the tongue. https://www.youtube.com/embed/uYvpUl7li9Y?wmode=transparent&start=0
A healthy tongue is pink although the shade may vary from person to person, ranging from dark to light pink.
A small amount of white coating can be normal. But significant changes or discolouration may indicate a disease or other issues.
How should I clean my tongue?
Cleaning your tongue only takes around 10-15 seconds, but it’s is a good way to check in with your health and can easily be incorporated into your teeth brushing routine.

You can clean your tongue by gently scrubbing it with a regular toothbrush. This dislodges any food debris and helps prevent microbes building up on its rough textured surface.
Or you can use a special tongue scraper. These curved instruments are made of metal or plastic, and can be used alone or accompanied by scrubbing with your toothbrush.
Your co-workers will thank you as well – cleaning your tongue can help combat stinky breath. Tongue scrapers are particularly effective at removing the bacteria that commonly causes bad breath, hidden in the tongue’s surface.
What’s that stuff on my tongue?
So, you’re checking your tongue during your twice-daily clean, and you notice something different. Noting these signs is the first step. If you observe any changes and they worry you, you should talk to your GP.
Here’s what your tongue might be telling you.
White coating
Developing a white coating on the tongue’s surface is one of the most common changes in healthy people. This can happen if you stop brushing or scraping the tongue, even for a few days.
In this case, food debris and microbes have accumulated and caused plaque. Gentle scrubbing or scraping will remove this coating. Removing microbes reduces the risk of chronic infections, which can be transferred to other organs and cause serious illnesses.

Yellow coating
This may indicate oral thrush, a fungal infection that leaves a raw surface when scrubbed.
Oral thrush is common in elderly people who take multiple medications or have diabetes. It can also affect children and young adults after an illness, due to the temporary suppression of the immune system or antibiotic use.
If you have oral thrush, a doctor will usually prescribe a course of anti-fungal medication for at least a month.
Black coating
Smoking or consuming a lot of strong-coloured food and drink – such as tea and coffee, or dishes with tumeric – can cause a furry appearance. This is known as a black hairy tongue. It’s not hair, but an overgrowth of bacteria which may indicate poor oral hygiene.

Pink patches
Pink patches surrounded by a white border can make your tongue look like a map – this is called “geographic tongue”. It’s not known what causes this condition, which usually doesn’t require treatment.
Pain and inflammation
A red, sore tongue can indicate a range of issues, including:
- nutritional deficiencies such as folic acid or vitamin B12
- diseases including pernicious anaemia, Kawasaki disease and scarlet fever
- inflammation known as glossitis
- injury from hot beverages or food
- ulcers, including cold sores and canker sores
- burning mouth syndrome.
Dryness
Many medications can cause dry mouth, also called xerostomia. These include antidepressants, anti-psychotics, muscle relaxants, pain killers, antihistamines and diuretics. If your mouth is very dry, it may hurt.
What about cancer?
White or red patches on the tongue that can’t be scraped off, are long-standing or growing need to checked out by a dental professional as soon as possible, as do painless ulcers. These are at a higher risk of turning into cancer, compared to other parts of the mouth.
Oral cancers have low survival rates due to delayed detection – and they are on the rise. So checking your tongue for changes in colour, texture, sore spots or ulcers is critical.
Dileep Sharma, Professor and Head of Discipline – Oral Health, University of Newcastle
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Laugh Often, To Laugh Longest!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Putting The Abs Into Absurdity
We’ve talked before about the health benefits of a broadly positive outlook on life:
Optimism Seriously Increases Longevity!
…and we’re very serious about it, but that’s about optimistic life views in general, and today we’re about not just keeping good humor in questionable circumstances, but actively finding good humor in the those moments—even when the moments in question might not be generally described as good!
After all, laughter really can be the best medicine, for example:
From the roots
First a quick recap on de-toothing the psychological aspect of threats, no matter how menacing they may be:
Hello, Emotions: Time For Radical Acceptance!
…which we can then take a step further:
What’s The Worst That Could Happen?
Choose your frame
Do you remember when that hacker hacked and publicized the US Federal no-fly list, after already hacking a nationwide cloud-based security camera company, getting access to more than 150,000 companies’ and private individuals’ security cameras, amongst various other cyber crimes, mostly various kinds of fraud and data theft?
Imagine how she (age 21) must have felt, when being indicted. What do you suppose this hacker had to say for itself under such circumstances?
❝congress is investigating now 🙂
but i stay silly :3 ❞
…the latter half of which, usually rendered “but I stay silly” or “but we stay silly” has since entered popular Gen-Z parlance, usually after expressing some negative thing, often in a state of powerlessness.
Which is an important life skill if powerlessness is something that is often likely.
It’s important for many Gen-Zs with negligible life prospects economically; it’s equally important for 60-somethings getting cancer diagnoses (statistically the most likely decade to find out one has cancer, by the way), and many other kinds of people younger, older, and in between.
Because at the end of the day, we all start powerless and we all end powerless.
Learned helplessness (two kinds)
In psychology, “learned helplessness” occurs when a person or creature gives up after learning that all and any attempts to resist a Bad Thing™ fail, perhaps even badly. A lab rat may just shut down and sit there getting electroshocked, for example. A person subjected to abuse may stop trying to improve their situation, and just go with the path of least resistance.
But, there’s another kind, wherein someone in a position of absolute powerlessness not only makes their peace with that, but also, decides that the one thing the outside world can’t control, is how they take it. Like the hacker we mentioned earlier.
Sometimes the gallows humor is even more literal, laughing at one’s own impending death. Not as a matter of bravado, but genuinely seeing the funny side.
But how?
Unfortunately, fortunately
The trick here is to “find a silver lining” that is nowhere near enough to compensate for the bad thing—and it may even be worse! But that’s fine:
“Unfortunately, I didn’t have time to do the dishes before leaving for my vacation. Fortunately, I also forgot to turn the oven off, so the house burning down covered up my messy kitchen”
Writer’s personal less drastic example: today I set my espresso machine to press me an espresso; it doesn’t have an auto-off and I got distracted and it overflowed everywhere; my immediate reaction was “Oh! I have been blessed with an abundance of coffee!”
This kind of silly little thing, on a daily basis, builds a very solid habit for life that allows one to see the funny side in even the most absurd situations, even matters of life and death (can confirm: been there enough times personally—so far so good, still alive to find the remembered absurdity silly).
The point is not to genuinely value the “silver lining”, because half the time it isn’t even one, really, and it is useless to pretend, in seriousness.
But to pretend in silliness? Now we’re onto something, and the real benefit is in the laughs we had along the way.
Because those worst moments? Are probably when we need it the most, so it’s good to get some practice in!
Want more ways to find the funny and make it a life habit?
We reviewed a good book recently:
The Humor Habit: Rewire Your Brain To Stress Less, Laugh More, And Achieve More’er – by Paul Osincup
Stay silly!
Share This Post
-
10 Ways To Naturally Boost Dopamine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dopamine is the “reward” hormone, and is responsible for motivation, as well as various oft-forgotten functions (such as spatial skills, motor functions, task processing, planning, and language). Sometimes, our relationship with dopamine isn’t what it could be, so here’s how to fix that:
Let’s get hormone-hacking…
Here are the 10 ways:
- The seesaw effect: reduce overstimulation by taking tolerance breaks from high-dopamine activities that aren’t particularly useful (like social media or phone games), allowing for natural enjoyment of daily activities that you’d normally find enjoyable. Think: if you died and negotiated to be sent back to life on the condition you’d appreciate it properly this time, what things would you then spend your time doing? It’s probably not Kingdom Crush Saga Farm 2, is it?
- Conscious state meditation: practise conscious state meditation, focusing inward to reduce anxiety and release dopamine. Even a few minutes a day can significantly enhance dopamine levels.
- Hack your REM cycles: optimize sleep, especially REM cycles, which produce the most dopamine. Aim to wake up after your final REM cycle to feel energized and happy.
- The runner’s high: engage in regular exercise, which boosts dopamine through physical exertion and can lead to feelings of relaxation and euphoria, often known as the “runner’s high.”
- Mood-enhancing music: listen to music that makes you feel good. Favorite songs can stimulate dopamine production, improving your mood and well-being.
- Bright light therapy: spend time in natural sunlight to stimulate dopamine production and elevate your mood, countering the negative effects of extended indoor time. If natural sunlight is not very available where you are (e.g. this writer who lives next to an ancient bog surrounded by fog and the days are getting short, at time of writing), then artificial daylight lamps are respectable supplement—but just that, a supplement, not a replacement. Despite how it looks/feels, natural sunlight (especially in the morning, to cue the circadian rhythm to do its thing) is beneficial even through cloud cover.
- Relieve stress for good: actively reduce stress, as it inhibits dopamine. Simplify daily routines and eliminate stressors to naturally boost dopamine and feel more relaxed. Of course, you cannot remove all stress from your life, so get good at managing the stress created by the stressors that do remain.
- Tap into your flow state: enter a “flow state” by focusing deeply on an engaging task, which can elevate dopamine levels and boost motivation and happiness.
- The hormesis effect: embrace mild physical challenges, like cold showers. The temporary discomfort will paradoxically increase dopamine (it’s the body’s way of saying “congratulations, you survived the hard thing, here’s a little treat, so that you’ll be motivated to survive the next hard thing, too”)
- Activate your inner artist: engage in creative activities that you find fun. The process of creating boosts dopamine and provides motivation, enhancing mood and enjoyment in life.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Rebalancing Dopamine (Without “Dopamine Fasting”)
Take care!
Share This Post
-
Mushrooms vs Eggplant – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing mushrooms to eggplant, we picked the mushrooms.
Why?
First, you may be wondering: which mushrooms? Button mushrooms? White mushrooms? Chestnut mushrooms? Portobello mushrooms? And the answer is yes. Those (and more; it represents most mushrooms that are commonly sold fresh in western supermarkets) are all the same species at different ages; namely, Agaricus bisporus—not to be mistaken for fly agaric, which despite the name, is not even a member of the Agaricus genus, and is in fact Amanita muscari. This is an important distinction, because fly agaric is poisonous, though fatality is rare, and it’s commonly enjoyed recreationally (after some preparation, which reduces its toxicity) for its psychoactive effects. It’s the famous red one with white spots. Anyway, today we will be talking instead about Agaricus bisporus, which is most popular western varieties of “edible mushroom”.
With that in mind, let’s get down to it:
In terms of macros, mushrooms contain more than 3x the protein, while eggplant contains nearly 2x the carbs and 3x the fiber. We’ll call this a tie for macros.
As for vitamins, mushrooms contain more of vitamins B1, B2, B3, B5, B6, B7, B9, B12, D, and choline, while eggplant contains more of vitamins A, E, and K. Most notably for vegans, mushrooms are a good non-animal source of vitamins B12 and D, which nutrients are not generally found in plants. Mushrooms, of course, are not technically plants. In any case, the vitamins category is an easy win for mushrooms.
When it comes to minerals, mushrooms have more copper, iron, phosphorus, potassium, selenium, and zinc, while eggplant has more calcium, magnesium, and manganese. Another easy win for mushrooms.
One final thing worth noting is that mushrooms are a rich source of the amino acid ergothioneine, which has been called a “longevity vitamin” for its healthspan-increasing effects (see our article below).
Meanwhile, in the category of mushrooms vs eggplant, mushrooms don’t leave much room for doubt and are the clear winner here.
Want to learn more?
You might like to read:
The Magic of Mushrooms: “The Longevity Vitamin” (That’s Not A Vitamin)
Take care!
Share This Post
Related Posts
-
Healing Cracked Fingers
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Question. Suffer from cracked (split) finger tips in the cold weather. Very painful, is there something I can take to ward off this off. Appreciate your daily email.❞
Ouch, painful indeed! Aside from good hydration (which is something we easily forget in cold weather), there’s no known internal guard against this*, but from the outside, oil-based moisturizers are the way to go.
Olive oil, coconut oil, jojoba oil, and shea butter are all fine options.
If the skin is broken such that infection is possible, then starting with an antiseptic ointment/cream is sensible. A good example product is Savlon, unless you are allergic to its active ingredient chlorhexidine.
*However, if perchance you are also suffering from peripheral neuropathy (a common comorbidity of cracked skin in the extremities), then lion’s main mushroom can help with that.
Writer’s anecdote: I myself started suffering from peripheral neuropathy in my hands earlier this year, doubtlessly due to some old injuries of mine.
However, upon researching for the above articles, I was inspired to try lion’s mane mushroom for myself. I take it daily, and have now been free of symptoms of peripheral neuropathy for several months.
Here’s an example product on Amazon, by the way
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Long-Covid Patients Are Frustrated That Federal Research Hasn’t Found New Treatments
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Erica Hayes, 40, has not felt healthy since November 2020 when she first fell ill with covid.
Hayes is too sick to work, so she has spent much of the last four years sitting on her beige couch, often curled up under an electric blanket.
“My blood flow now sucks, so my hands and my feet are freezing. Even if I’m sweating, my toes are cold,” said Hayes, who lives in Western Pennsylvania. She misses feeling well enough to play with her 9-year-old son or attend her 17-year-old son’s baseball games.
Along with claiming the lives of 1.2 million Americans, the covid-19 pandemic has been described as a mass disabling event. Hayes is one of millions of Americans who suffer from long covid. Depending on the patient, the condition can rob someone of energy, scramble the autonomic nervous system, or fog their memory, among many other http://symptoms.in/ addition to the brain fog and chronic fatigue, Hayes’ constellation of symptoms includes frequent hives and migraines. Also, her tongue is constantly swollen and dry.
“I’ve had multiple doctors look at it and tell me they don’t know what’s going on,” Hayes said about her tongue.
Estimates of prevalence range considerably, depending on how researchers define long covid in a given study, but the Centers for Disease Control and Prevention puts it at 17 million adults.
Despite long covid’s vast reach, the federal government’s investment in researching the disease — to the tune of $1.15 billion as of December — has so far failed to bring any new treatments to market.
This disappoints and angers the patient community, who say the National Institutes of Health should focus on ways to stop their suffering instead of simply trying to understand why they’re suffering.
“It’s unconscionable that more than four years since this began, we still don’t have one FDA-approved drug,” said Meighan Stone, executive director of the Long COVID Campaign, a patient-led advocacy organization. Stone was among several people with long covid who spoke at a workshop hosted by the NIH in September where patients, clinicians, and researchers discussed their priorities and frustrations around the agency’s approach to long-covid research.
Some doctors and researchers are also critical of the agency’s research initiative, called RECOVER, or Researching COVID to Enhance Recovery. Without clinical trials, physicians specializing in treating long covid must rely on hunches to guide their clinical decisions, said Ziyad Al-Aly, chief of research and development with the VA St Louis Healthcare System.
“What [RECOVER] lacks, really, is clarity of vision and clarity of purpose,” said Al-Aly, saying he agrees that the NIH has had enough time and money to produce more meaningful progress.
Now the NIH is starting to determine how to allocate an additional $662 million of funding for long-covid research, $300 million of which is earmarked for clinical trials. These funds will be allocated over the next four http://years.at/ the end of October, RECOVER issued a request for clinical trial ideas that look at potential therapies, including medications, saying its goal is “to work rapidly, collaboratively, and transparently to advance treatments for Long COVID.”
This turn suggests the NIH has begun to respond to patients. This has stirred cautious optimism among those who say that the agency’s approach to long covid has lacked urgency in the search for effective treatments.Stone calls this $300 million a down payment. She warns it’s going to take a lot more money to help people like Hayes regain some degree of health.“There really is a burden to make up this lost time now,” Stone said.
The NIH told KFF Health News and NPR via email that it recognizes the urgency in finding treatments. But to do that, there needs to be an understanding of the biological mechanisms that are making people sick, which is difficult to do with post-infectious conditions.
That’s why it has funded research into how long covid affects lung function, or trying to understand why only some people are afflicted with the condition.
Good Science Takes Time
In December 2020, Congress appropriated $1.15 billion for the NIH to launch RECOVER, raising hopes in the long-covid patient community.
Then-NIH Director Francis Collins explained that RECOVER’s goal was to better understand long covid as a disease and that clinical trials of potential treatments would come later.
According to RECOVER’s website, it has funded eight clinical trials to test the safety and effectiveness of an experimental treatment or intervention. Just one of those trials has published results.
On the other hand, RECOVER has supported more than 200 observational studies, such as research on how long covid affects pulmonary function and on which symptoms are most common. And the initiative has funded more than 40 pathobiology studies, which focus on the basic cellular and molecular mechanisms of long covid.
RECOVER’s website says this research has led to crucial insights on the risk factors for developing long covid and on understanding how the disease interacts with preexisting conditions.
It notes that observational studies are important in helping scientists to design and launch evidence-based clinical trials.
Good science takes time, said Leora Horwitz, the co-principal investigator for the RECOVER-Adult Observational Cohort at New York University. And long covid is an “exceedingly complicated” illness that appears to affect nearly every organ system, she said.
This makes it more difficult to study than many other diseases. Because long covid harms the body in so many ways, with widely variable symptoms, it’s harder to identify precise targets for treatment.
“I also will remind you that we’re only three, four years into this pandemic for most people,” Horwitz said. “We’ve been spending much more money than this, yearly, for 30, 40 years on other conditions.”
NYU received nearly $470 million of RECOVER funds in 2021, which the institution is using to spearhead the collection of data and biospecimens from up to 40,000 patients. Horwitz said nearly 30,000 are enrolled so far.
This vast repository, Horwitz said, supports ongoing observational research, allowing scientists to understand what is happening biologically to people who don’t recover after an initial infection — and that will help determine which clinical trials for treatments are worth undertaking.
“Simply trying treatments because they are available without any evidence about whether or why they may be effective reduces the likelihood of successful trials and may put patients at risk of harm,” she said.
Delayed Hopes or Incremental Progress?
The NIH told KFF Health News and NPR that patients and caregivers have been central to RECOVER from the beginning, “playing critical roles in designing studies and clinical trials, responding to surveys, serving on governance and publication groups, and guiding the initiative.”But the consensus from patient advocacy groups is that RECOVER should have done more to prioritize clinical trials from the outset. Patients also say RECOVER leadership ignored their priorities and experiences when determining which studies to fund.
RECOVER has scored some gains, said JD Davids, co-director of Long COVID Justice. This includes findings on differences in long covid between adults and kids.But Davids said the NIH shouldn’t have named the initiative “RECOVER,” since it wasn’t designed as a streamlined effort to develop treatments.
“The name’s a little cruel and misleading,” he said.
RECOVER’s initial allocation of $1.15 billion probably wasn’t enough to develop a new medication to treat long covid, said Ezekiel J. Emanuel, co-director of the University of Pennsylvania’s Healthcare Transformation Institute.
But, he said, the results of preliminary clinical trials could have spurred pharmaceutical companies to fund more studies on drug development and test how existing drugs influence a patient’s immune response.
Emanuel is one of the authors of a March 2022 covid roadmap report. He notes that RECOVER’s lack of focus on new treatments was a problem. “Only 15% of the budget is for clinical studies. That is a failure in itself — a failure of having the right priorities,” he told KFF Health News and NPR via email.
And though the NYU biobank has been impactful, Emanuel said there needs to be more focus on how existing drugs influence immune response.
He said some clinical trials that RECOVER has funded are “ridiculous,” because they’ve focused on symptom amelioration, for example to study the benefits of over-the-counter medication to improve sleep. Other studies looked at non-pharmacological interventions, such as exercise and “brain training” to help with cognitive fog.
People with long covid say this type of clinical research contributes to what many describe as the “gaslighting” they experience from doctors, who sometimes blame a patient’s symptoms on anxiety or depression, rather than acknowledging long covid as a real illness with a physiological basis.
“I’m just disgusted,” said long-covid patient Hayes. “You wouldn’t tell somebody with diabetes to breathe through it.”
Chimére L. Sweeney, director and founder of the Black Long Covid Experience, said she’s even taken breaks from seeking treatment after getting fed up with being told that her symptoms were due to her diet or mental health.
“You’re at the whim of somebody who may not even understand the spectrum of long covid,” Sweeney said.
Insurance Battles Over Experimental Treatments
Since there are still no long-covid treatments approved by the Food and Drug Administration, anything a physician prescribes is classified as either experimental — for unproven treatments — or an off-label use of a drug approved for other conditions. This means patients can struggle to get insurance to cover prescriptions.
Michael Brode, medical director for UT Health Austin’s Post-COVID-19 Program — said he writes many appeal letters. And some people pay for their own treatment.
For example, intravenous immunoglobulin therapy, low-dose naltrexone, and hyperbaric oxygen therapy are all promising treatments, he said.
For hyperbaric oxygen, two small, randomized controlled studies show improvements for the chronic fatigue and brain fog that often plague long-covid patients. The theory is that higher oxygen concentration and increased air pressure can help heal tissues that were damaged during a covid infection.
However, the out-of-pocket cost for a series of sessions in a hyperbaric chamber can run as much as $8,000, Brode said.
“Am I going to look a patient in the eye and say, ‘You need to spend that money for an unproven treatment’?” he said. “I don’t want to hype up a treatment that is still experimental. But I also don’t want to hide it.”
There’s a host of pharmaceuticals that have promising off-label uses for long covid, said microbiologist Amy Proal, president and chief scientific officer at the Massachusetts-based PolyBio Research Foundation. For instance, she’s collaborating on a clinical study that repurposes two HIV drugs to treat long covid.
Proal said research on treatments can move forward based on what’s already understood about the disease. For instance, she said that scientists have evidence — partly due to RECOVER research — that some patients continue to harbor small amounts of viral material after a covid infection. She has not received RECOVER funds but is researching antivirals.
But to vet a range of possible treatments for the millions suffering now — and to develop new drugs specifically targeting long covid — clinical trials are needed. And that requires money.
Hayes said she would definitely volunteer for an experimental drug trial. For now, though, “in order to not be absolutely miserable,” she said she focuses on what she can do, like having dinner with her http://family.at/ the same time, Hayes doesn’t want to spend the rest of her life on a beige couch.
RECOVER’s deadline to submit research proposals for potential long-covid treatments is Feb. 1.
This article is from a partnership that includes NPR and KFF Health News.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Antidepressants: Personalization Is Key!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Antidepressants: Personalization Is Key!
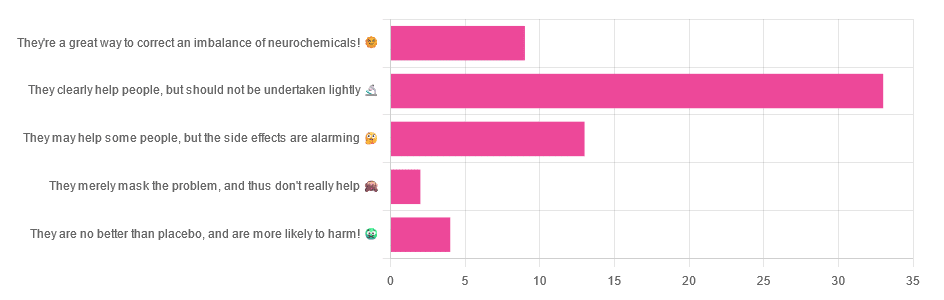
Yesterday, we asked you for your opinions on antidepressants, and got the above-depicted, below-described, set of responses:
- Just over half of respondents said “They clearly help people, but should not be undertaken lightly”
- Just over a fifth of respondents said “They may help some people, but the side effects are alarming”
- Just under a sixth of respondents said “They’re a great way to correct an imbalance of neurochemicals”
- Four respondents said “They are no better than placebo, and are more likely to harm”
- Two respondents said “They merely mask the problem, and thus don’t really help”
So what does the science say?
❝They are no better than placebo, and are more likely to harm? True or False?❞
True or False depending on who you are and what you’re taking. Different antidepressants can work on many different systems with different mechanisms of action. This means if and only if you’re not taking the “right” antidepressant for you, then yes, you will get only placebo benefits:
- Placebo Effect in the Treatment of Depression and Anxiety ← randomly assigned antidepressants are, shockingly, luck of the draw in usefulness
- Antidepressants versus placebo in major depression: an overview ← “wow this science is messy”
- Comparative efficacy and acceptability of 21 antidepressant drugs: a systematic review and network meta-analysis ← “oh look, it makes a difference which antidepressant we give to people”
Rather than dismissing antidepressants as worthless, therefore, it is a good idea to find out (by examination or trial and error) what kind of antidepressant you need, if you indeed do need such.
Otherwise it is like getting a flu shot and being surprised when you still catch a cold!
❝They merely mask the problem, and thus don’t really help: True or False?❞
False, categorically.
The problem in depressed people is the depressed mood. This may be influenced by other factors, and antidepressants indeed won’t help directly with those, but they can enable the person to better tackle them (more on this later).
❝They may help some people, but the side-effects are alarming: True or False?❞
True or False depending on more factors than we can cover here.
Side-effects vary from drug to drug and person to person, of course. As does tolerability and acceptability, since to some extent these things are subjective.
One person’s dealbreaker may be another person’s shrugworthy minor inconvenience at most.
❝They’re a great way to correct an imbalance of neurochemicals: True or False?❞
True! Contingently.
That is to say: they’re a great way to correct an imbalance of neurochemicals if and only if your problem is (at least partly) an imbalance of neurochemicals. If it’s not, then your brain can have all the neurotransmitters it needs, and you will still be depressed, because (for example) the other factors* influencing your depression have not changed.
*common examples include low self-esteem, poor physical health, socioeconomic adversity, and ostensibly bleak prospects for the future.
For those for whom the problem is/was partly a neurochemical imbalance and partly other factors, the greatest help the antidepressants give is getting the brain into sufficient working order to be able to tackle those other factors.
Want to know more about the different kinds?
Here’s a helpful side-by-side comparison of common antidepressants, what type they are, and other considerations:
Mind | Comparing Antidepressants
Want a drug-free approach?
You might like our previous main feature:
The Mental Health First-Aid That You’ll Hopefully Never Need
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: