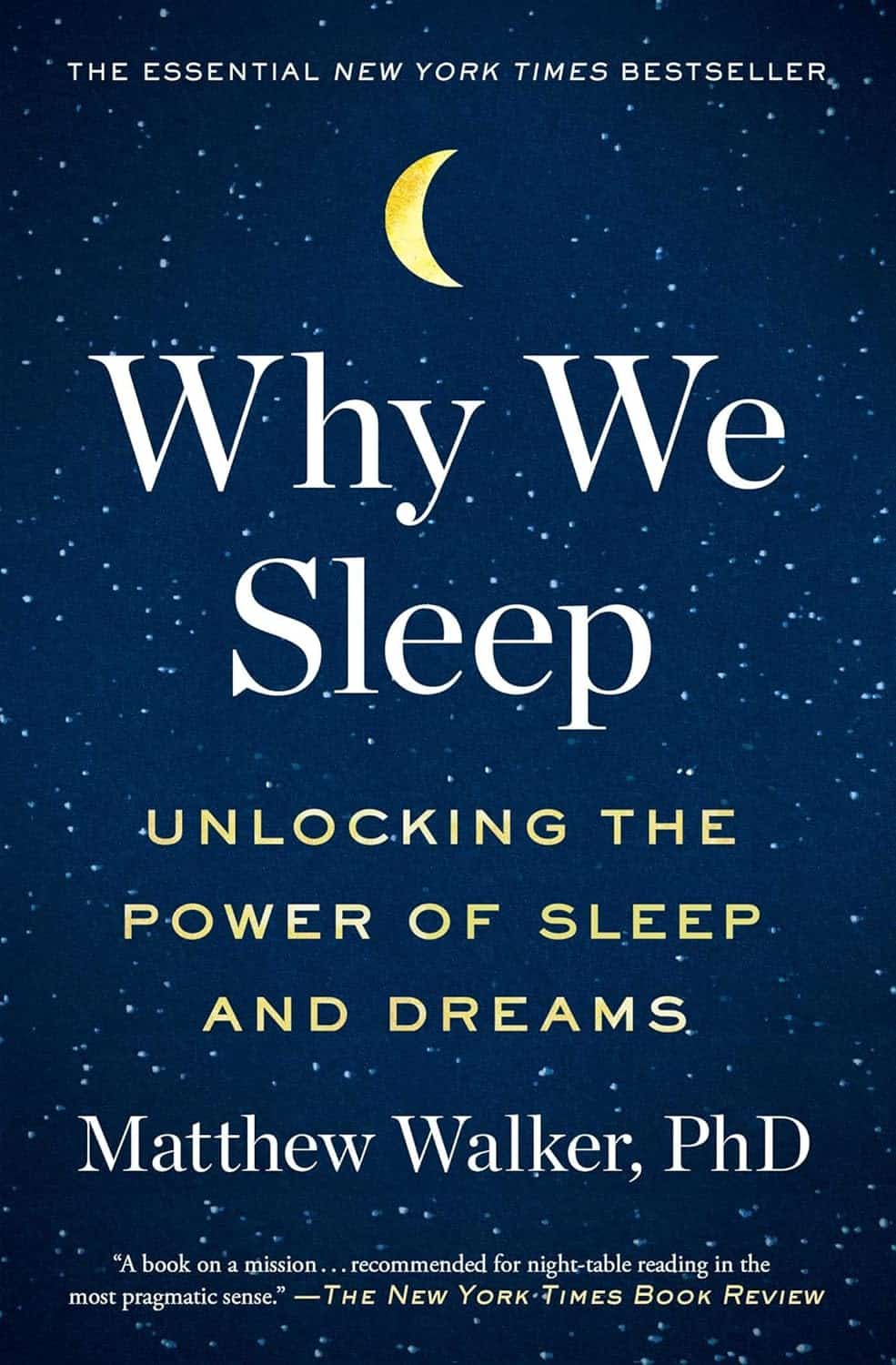
Why We Sleep – by Dr Matthew Walker
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
- We all know sleep is important.
- We all know that without it, we’ll suffer rapid cognitive decline.
- We all know approximately what we’re supposed to do to get good sleep.
So what does this book bring to the table? Mostly, deep understanding (written from the perspective of a career in sleep science) presented in such a way as to be applicable, by you, in your life. Stop sabotaging yourself before you even get out of your bed in the morning!
Hustle culture champions early mornings and late nights, and either or both of those might be difficult to avoid. But to make what you’re doing sustainable, you’re going to have to make some informed decisions about looking after your #1 asset—you!
Dr. Walker writes in a clear and accessible fashion, without skimping on the hard science, and always with practical application in mind. All in all, we can’t recommend this one enough.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Aging with Grace – by Dr. David Snowdon
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this book is not: a book about Christianity. Don’t worry, we didn’t suddenly change the theme of 10almonds.
Rather, what this book is: a book about a famous large (n=678) study into the biology of aging, that took a population sample of women who had many factors already controlled-for, e.g. they ate the same food, had the same schedule, did the same activities, etc—for many years on end. In other words, a convent of nuns.
This allowed for a lot more to be learned about other factors that influence aging, such as:
- Heredity / genetics in general
- Speaking more than one language
- Supplementing with vitamins or not
- Key adverse events (e.g. stroke)
- Key chronic conditions (e.g. depression)
The book does also cover (as one might expect) the role that community and faith can play in healthy longevity, but since the subjects were 678 communally-dwelling people of faith (thus: no control group of faithless loners), this aspect is discussed only in anecdote, or in reference to other studies.
The author of this book, by the way, was the lead researcher of the study, and he is a well-recognised expert in the field of Alzheimer’s in particular (and Alzheimer’s does feature quite a bit throughout).
The writing style is largely narrative, and/but with a lot of clinical detail and specific data; this is by no means a wishy-washy book.
Bottom line: if you’d like to know what nuns were doing in the 1980s to disproportionally live into three-figure ages, then this book will answer those questions.
Click here to check out Aging with Grace, and indeed age with grace!
Share This Post
-
Pistachios vs Walnuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pistachios to walnuts, we picked the pistachios.
Why?
Pistachios have more protein and fiber, while walnuts have more fat (though the fats are famously healthy, the same is true of the fats in pistachios).
In the category of vitamins, pistachios have several times more* of vitamins A, B1, B6, C, and E, while walnuts boast only a little more of vitamin B9. They are approximately equal on other vitamins they both contain.
*actually 25x more vitamin A, but the others are 2x, 3x, 4x more.
When it comes to minerals, things are more even; pistachios have more iron, phosphorus, potassium, and selenium, while walnuts have more copper, magnesium, manganese, and zinc. So this category’s a tie.
So given two clear wins for pistachios, and one tie, it’s evident that pistachios win the day.
However! Do enjoy both of these nuts; we often mention that diversity is good in general, and in this case, it’s especially true because of the different mineral profiles, and also because in terms of the healthy fats that they offer, pistachios offer more monounsaturated fats and walnuts offer more polyunsaturated fats; both are healthy, just different.
They’re about equal on saturated fat, in case you were wondering, as it makes up about 6% of the total fats in both cases.
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Share This Post
-
War in Ukraine affected wellbeing worldwide, but people’s speed of recovery depended on their personality
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The war in Ukraine has had impacts around the world. Supply chains have been disrupted, the cost of living has soared and we’ve seen the fastest-growing refugee crisis since World War II. All of these are in addition to the devastating humanitarian and economic impacts within Ukraine.
Our international team was conducting a global study on wellbeing in the lead up to and after the Russian invasion. This provided a unique opportunity to examine the psychological impact of the outbreak of war.
As we explain in a new study published in Nature Communications, we learned the toll on people’s wellbeing was evident across nations, not just in Ukraine. These effects appear to have been temporary – at least for the average person.
But people with certain psychological vulnerabilities struggled to recover from the shock of the war.
Tracking wellbeing during the outbreak of war
People who took part in our study completed a rigorous “experience-sampling” protocol. Specifically, we asked them to report their momentary wellbeing four times per day for a whole month.
Data collection began in October 2021 and continued throughout 2022. So we had been tracking wellbeing around the world during the weeks surrounding the outbreak of war in February 2022.
We also collected measures of personality, along with various sociodemographic variables (including age, gender, political views). This enabled us to assess whether different people responded differently to the crisis. We could also compare these effects across countries.
Our analyses focused primarily on 1,341 participants living in 17 European countries, excluding Ukraine itself (44,894 experience-sampling reports in total). We also expanded these analyses to capture the experiences of 1,735 people living in 43 countries around the world (54,851 experience-sampling reports) – including in Australia.
A global dip in wellbeing
On February 24 2022, the day Russia invaded Ukraine, there was a sharp decline in wellbeing around the world. There was no decline in the month leading up to the outbreak of war, suggesting the change in wellbeing was not already occurring for some other reason.
However, there was a gradual increase in wellbeing during the month after the Russian invasion, suggestive of a “return to baseline” effect. Such effects are commonly reported in psychological research: situations and events that impact our wellbeing often (though not always) do so temporarily.
Unsurprisingly, people in Europe experienced a sharper dip in wellbeing compared to people living elsewhere around the world. Presumably the war was much more salient for those closest to the conflict, compared to those living on an entirely different continent.
Interestingly, day-to-day fluctuations in wellbeing mirrored the salience of the war on social media as events unfolded. Specifically, wellbeing was lower on days when there were more tweets mentioning Ukraine on Twitter/X.
Our results indicate that, on average, it took around two months for people to return to their baseline levels of wellbeing after the invasion.
Different people, different recoveries
There are strong links between our wellbeing and our individual personalities.
However, the dip in wellbeing following the Russian invasion was fairly uniform across individuals. None of the individual factors assessed in our study, including personality and sociodemographic factors, predicted people’s response to the outbreak of war.
On the other hand, personality did play a role in how quickly people recovered. Individual differences in people’s recovery were linked to a personality trait called “stability”. Stability is a broad dimension of personality that combines low neuroticism with high agreeableness and conscientiousness (three traits from the Big Five personality framework).
Stability is so named because it reflects the stability of one’s overall psychological functioning. This can be illustrated by breaking stability down into its three components:
- low neuroticism describes emotional stability. People low in this trait experience less intense negative emotions such as anxiety, fear or anger, in response to negative events
- high agreeableness describes social stability. People high in this trait are generally more cooperative, kind, and motivated to maintain social harmony
- high conscientiousness describes motivational stability. People high in this trait show more effective patterns of goal-directed self-regulation.
So, our data show that people with less stable personalities fared worse in terms of recovering from the impact the war in Ukraine had on wellbeing.
In a supplementary analysis, we found the effect of stability was driven specifically by neuroticism and agreeableness. The fact that people higher in neuroticism recovered more slowly accords with a wealth of research linking this trait with coping difficulties and poor mental health.
These effects of personality on recovery were stronger than those of sociodemographic factors, such as age, gender or political views, which were not statistically significant.
Overall, our findings suggest that people with certain psychological vulnerabilities will often struggle to recover from the shock of global events such as the outbreak of war in Ukraine.
Luke Smillie, Professor in Personality Psychology, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Build Strong Feet: Exercises To Strengthen Your Foot & Ankle
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot depends on the health of our feet, especially when it comes to their strength and stability. But they often get quite neglected, when it comes to maintenance. Here’s how to help your feet keep the rest of your body in good condition:
On a good footing
The foot-specific exercises recommended here include:
- Active toe flexion/extension: curl and extend your toes
- Active toe adduction/abduction: use a towel for feedback this time as you spread your toes
- “Short foot” exercise: create an arch by bringing the base of your big toe towards your heel
- Resisted big toe flexion: use resistance bands; flex your big toe while controlling the others.
- Standing big toe flexion (isometric): press your big toe against an inclined surface as forcefully as you can
- Foot bridge exercise: hold your position with the front part of your feet on an elevated surface, to strengthen the arch.
- Heel raises: which can be progressed from basic to more advanced variations, increasing difficulty
- Ankle movements: dorsiflexion, inversion, etc, to increase mobility
It’s important to also look after your general lower body strength and stability, including (for example) single-leg deadlifts, step-downs, and lunges
Balance and proprioceptive exercises are good too, such as a static or dynamic one-leg balances, progressing to doing them with your eyes closed and/or on unstable surfaces (be careful, of course, and progress to this only when confident).
For more on all of these, an explanation of the anatomy, some other exercises too, and visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Steps For Keeping Your Feet A Healthy Foundation
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Lifespan vs Healthspan, And The Spice Of Life
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Great newsletter. Am taking turmeric for inflammation of hips and feet. Works like magic. Would like to know how it works, and what tumeric is best combined with – also whether there any risks in longterm use.❞
Glad you’re enjoying! As for turmeric, it sure is great, isn’t it? To answer your questions in a brief fashion:
- How it works: it does a lot of things, but perhaps its most key feature is its autoxidative metabolites that mediate its anti-inflammatory effect. This, it slows or inhibits oxidative stress that would otherwise cause inflammation, increase cancer risk, and advance aging.
- Best combined with: black pepper
- Any risks in long-term use: there are no known risks in long-term use ← that’s just one study, but there are lots. Some studies were prompted by reported hepatotoxicity of curcumin supplements, but a) the reports themselves seem to be without evidence b) the reported hepatoxicity was in relation to contaminants in the supplements, not the curcumin itself c) clinical trials were unable to find any hepatotoxicity (or other) risks anyway. Here’s an example of such a study.
You might also like our previous main feature: Why Curcumin (Turmeric) Is Worth Its Weight In Gold
❝This push for longevity is appealing but watching my mother in her nineties is a life I’m not looking forward to. Healthy longevity, yes, but longevity for the sake of a longer life? No thank you.❞
Yes, you’re quite right, that’s exactly the point! Assuming we live to die of age-related conditions (i.e., we do not suffer a fatal accident or incident in our younger years), those unfun last years are coming whether they come at 75 or 95. Or earlier or later, because that can absolutely happen too!
For example: nearly 10% of Americans over 65 have difficulty with self-care
As a rule, and we’ve covered some of the science of this previously, having at least 4 out of 5 of the “big 5” lifestyle factors (diet, exercise, sleep, low-or-zero alcohol, not smoking) not only extends life, but specifically extends the healthspan, i.e. the count of healthy life-years that precedes final age-related decline.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Collard Greens vs Watercress – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing collard greens to watercress, we picked the collard greens.
Why?
It was close! But…
In terms of macros, collard greens have 8x the fiber, 4x the carbs, and slightly more protein. The fiber-to-carbs ratio also gives collard greens the lower glycemic index, although honestly, nobody is getting metabolic disease from eating watercress. Still, by the numbers it’s a clear win for collard greens, and especially 8x the fiber is not to be undervalued!
When it comes to vitamins, things were much more even; collard greens have more of vitamins A, B3, B9, K, and choline, while watercress has more of vitamins B1, B2, B5, C, and E. They’re tied on vitamin B6, so that makes a 5.5:5.5 tie overall. Looking for a tiebreaker, collard greens’ margins of difference are greater, so we could call this a tie or the narrowest of wins for collard greens ion this category.
In the category of minerals, collard greens have more calcium, copper, iron, manganese, and zinc, while watercress has more copper, phosphorus, potassium, and selenium. They’re tied on magnesium. This time the margins of difference are also comparable, so there’s really no tiebreaker available for this one. Thus, an absolute tie on minerals.
Looking at polyphenols, watercress has slightly more, with the main contender being 4mg/100g quercetin.
Adding up the sections results in either a tie or a slight for collard greens based on the tiebreaker in the vitamins category.
We can also put the two clear wins (one for collard greens and one for watercress), and say that in our opinion, collard greens’ 4g/100g fiber beats watercress’s 4mg/100g quercetin.
Quercetin is great and all, but:
- if you buy a quercetin supplement like this one on Amazon it’s 1000mg capsules, so how critical is watercress’s 4mg, really? Yes, getting it from food is better, but it’s not 25,000% better.
- no doctor that we know of is saying “you need more quercetin or you’re going to die”, but they do say “you need more fiber or you’re going to die”
- indeed, the WHO passionately proclaims that 95% of people in the US especially desperately need to eat more fiber, whereas there is no similar giant public health campaign begging people to have 4mg more of quercetin
…so we’ll say that’s another tiebreaker in favor of collard greens.
In short: collard greens scrape a win based on several tiebreakers, but watercress was a very close contender indeed!
Of course, by all means enjoy either or (ideally!) both; diversity is good.
Want to learn more?
You might like:
What’s Your Plant Diversity Score?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: