Why does alcohol make my poo go weird?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As we enter the festive season it’s a good time to think about what all those celebratory alcoholic drinks can do to your gut.
Alcohol can interfere with the time it takes for food to go through your gut (also known as the “transit time”). In particular, it can affect the muscles of the stomach and the small bowel (also known as the small intestine).
So, how and why does alcohol make your poos goes weird? Here’s what you need to know.
Diarrhoea and the ‘transit time’
Alcohol’s effect on stomach transit time depends on the alcohol concentration.
In general, alcoholic beverages such as whisky and vodka with high alcohol concentrations (above 15%) slow down the movement of food in the stomach.
Beverages with comparatively low alcohol concentrations (such as wine and beer) speed up the movement of food in the stomach.
These changes in gut transit explain why some people can get a sensation of fullness and abdominal discomfort when they drink vodka or whisky.
How long someone has been drinking a lot of alcohol can affect small bowel transit.
We know from experiments with rats that chronic use of alcohol accelerates the transit of food through the stomach and small bowel.
This shortened transit time through the small bowel also happens when humans drink a lot of alcohol, and is linked to diarrhoea.
Alcohol can also reduce the absorption of carbohydrates, proteins and fats in the duodenum (the first part of the small bowel).
Alcohol can lead to reduced absorption of xylose (a type of sugar). This means diarrhoea is more likely to occur in drinkers who also consume a lot of sugary foods such as sweets and sweetened juices.
Chronic alcohol use is also linked to:
- lactose intolerance
- overgrowth of small bowel bacteria and
- reduced absorption of fats from the pancreas not producing enough digestive enzymes.
This means chronic alcohol use may lead to diarrhoea and loose stools.
How might a night of heavy drinking affect your poos?
When rats are exposed to high doses of alcohol over a short period of time, it results in small bowel transit delay.
This suggests acute alcohol intake (such as an episode of binge drinking) is more likely to lead to constipation than diarrhoea.
This is backed up by recent research studying the effects of alcohol in 507 university students.
These students had their stools collected and analysed, and were asked to fill out a stool form questionnaire known as the Bristol Stool Chart.
The research found a heavy drinking episode was associated with harder, firm bowel motions.
In particular, those who consumed more alcohol had more Type 1 stools, which are separate hard lumps that look or feel a bit like nuts.
The researchers believed this acute alcohol intake results in small bowel transit delay; the food stayed for longer in the intestines, meaning more water was absorbed from the stool back into the body. This led to drier, harder stools.
Interestingly, the researchers also found there was more of a type of bacteria known as “Actinobacteria” in heavy drinkers than in non-drinkers.
This suggests bacteria may have a role to play in stool consistency.
But binge drinking doesn’t always lead to constipation. Binge drinking in patients with irritable bowel syndrom (IBS), for example, clearly leads to diarrhoea, nausea and abdominal pain.
What can I do about all this?
If you’re suffering from unwanted bowel motion changes after drinking, the most effective way to address this is to limit your alcohol intake.
Some alcoholic beverages may affect your bowel motions more than others. If you notice a pattern of troubling poos after drinking certain drinks, it may be sensible to cut back on those beverages.
If you tend to get diarrhoea after drinking, avoid mixing alcohol with caffeinated drinks. Caffeine is known to stimulate contractions of the colon and so could worsen diarrhoea.
If constipation after drinking is the problem, then staying hydrated is important. Drinking plenty of water before drinking alcohol (and having water in between drinks and after the party is over) can help reduce dehydration and constipation.
You should also eat before drinking alcohol, particularly protein and fibre-rich foods.
Food in the stomach can slow the absorption of alcohol and may help protect against the negative effects of alcohol on the gut lining.
Is it anything to worry about?
Changes in bowel motions after drinking are usually short term and, for the most part, resolve themselves pretty efficiently.
But if symptoms such as diarrhoea persist beyond a couple of days after stopping alcohol, it may signify other concerning issues such as an underlying gut disorder like inflammatory bowel disease.
Researchers have also linked alcohol consumption to the development of irritable bowel syndrome.
If problems persist or if there are alarming symptoms such as blood in your stool, seek medical advice from a general practitioner.
Vincent Ho, Associate Professor and clinical academic gastroenterologist, Western Sydney University
This article is republished from The Conversation under a Creative Commons license. Read the original article.

Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
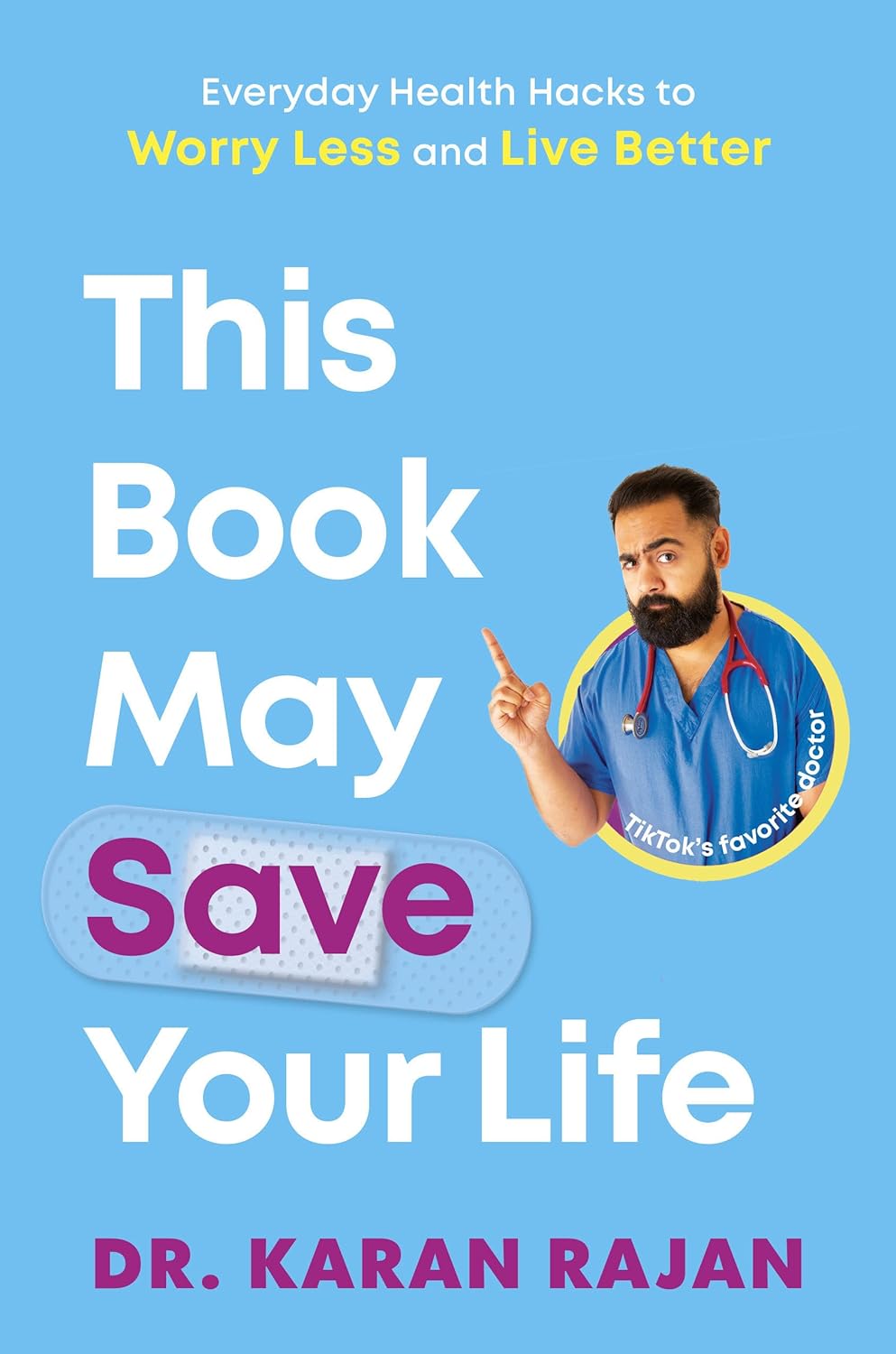
This Book May Save Your Life – by Dr. Karan Rajan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The title is a bold sell, but the book does include a lot of information about what can go wrong in your body, and how those things can be avoided.
What it’s not: a reiteration of Dr. Michael Greger’s “How Not To Die“. It’s not dense medical information, and it doesn’t cite papers at a rate of ten per page.
What it is: an easy-reading tour guide of the human body and its many quirks and foibles, and how we can leverage those to our benefit. On which note…
Hopefully, your insides will never see the light of day, but this author is a general surgeon and as such, is an experienced and well-qualified tour guide. Here, we learn about everything from the long and interesting journey through our gut, to the unique anatomical features and liabilities of the brain. From the bizarre oddities of the genitals, to things most people don’t know about the process of death.
The style of the book is very casual, with lots of short sections (almost mini chapters-within-chapters, really) making for very light reading—and certainly enjoyable reading too, unless you are inclined to squeamishness.
Bottom line: in honesty, the book is more informative than it is instructional, though it does contain the promised health tips too. With that in mind, it’s a very enjoyable and educational read, and we do recommend it.
Share This Post
-
Get Better Sleep: Beyond “Sleep Hygiene”
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Better Sleep, Better Life!
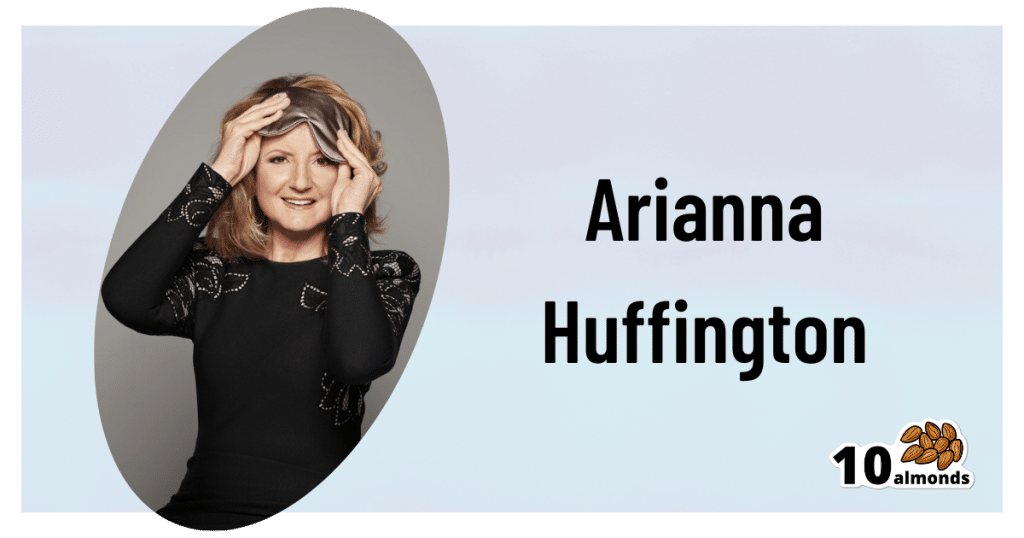
This is Arianna Huffington. Yes, that Huffington, of the Huffington Post. But! She’s also the CEO of Thrive Global, a behavior change tech company with the mission of changing the way we work and live—in particular, by challenging the idea that burnout is the required price of success.
The power of better sleep
Sleep is a very important, but most often neglected, part of good health. Here are some of Huffington’s top insights from her tech company Thrive, and as per her “Sleep Revolution” initiative.
Follow your circadian rhythm
Are you a night owl or a morning lark? Whichever it is, roll with it, and plan around that if your lifestyle allows for such. While it is possible to change from one to the other, we do have a predisposition towards one or the other, and will generally function best when not fighting it.
This came about, by the way, because we evolved to have half of us awake in the mornings and half in the evenings, to keep us all safe. Socially we’ve marched onwards from that point in evolutionary history, but our bodies are about a hundred generations behind the times, and that’s just what we have to work with!
Don’t be afraid (or ashamed!) to take naps
Naps, done right, can be very good for the health—especially if we had a bad night’s sleep the previous night.
Thrive found that workers are more productive when they have nap rooms, and (following on a little from the previous point) are allowed to sleep in or work from home.
See also: How To Nap Like A Pro (No More “Sleep Hangovers”!)
Make sure you have personal space available in bed
The correlation between relationship satisfaction and sleeping close to one’s partner has been found to be so high that it’s even proportional: the further away a couple sleeps from each other, the less happy they are. But…
Partners who got good sleep the previous night, will be more likely to want intimacy on any given night—at a rate of an extra 14% per extra hour of sleep the previous night. So, there’s a trade-off, as having more room in bed tends to result in better sleep. Time to get a bigger bed?
What gets measured, gets done
This goes for sleep, too! Not only does dream-journaling in the morning cue your subconscious to prepare to dream well the following night, but also, sleep trackers and sleep monitoring apps go a very long way to improving sleep quality, even if no extra steps are consciously taken to “score better”.
We’ve previously reviewed some of the most popular sleep apps; you can check out for yourself how they measured up:
Share This Post
-
Eat to Beat Depression and Anxiety – by Dr. Drew Ramsey
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most of us could use a little mood boost sometimes, and some of us could definitely stand to have our baseline neurochemistry elevated a bit. We’ve probably Googled “foods to increase dopamine”, and similar phrases. So, why is this a book, and not just an article saying to eat cashews and dark chocolate?
Dr. Drew Ramsey takes a holistic approach to health. By this we mean that to have good health, the whole body and mind must be kept healthy. Let a part slip, and the others will soon follow. Improve a part, and the others will soon follow, too.
Of course, there is only so much that diet can do. Jut as no diet will replace a Type 1 Diabetic’s pancreas with a working one, no diet will treat the causes of some kinds of depression and anxiety.
For this reason, Dr. Ramsey, himself a psychiatrist (and a farmer!) recommends a combination of talking therapy and diet, with medications as a “third leg” to be included when necessary. The goal, for him, is to reduce dependence on medications, while still recognizing when they can be useful or even necessary.
As for the practical, actionable advices in the book, he does (unsurprisingly) recommend a Mediterranean diet. Heavy on the greens and beans, plenty of colorful fruit and veg, small amounts of fish and seafood, even smaller amounts of grass-fed beef and fermented dairy. He also discusses a bunch of “superfoods” he particularly recommends.
Nor does he just hand-wave the process; he talks about the science of how and why each of these things helps.
And in practical terms, he even devotes some time to helping the reader get our kitchen set up, if we’re not already ready-to-go in that department. He also caters to any “can’t cook / won’t cook” readers and how to work around that too.
Bottom line: if you’d like to get rewiring your brain (leveraging neuroplasticity is a key component of the book), this will get you on track. A particular strength is how the author “thinks of everything” in terms of common problems that people (especially: depressed and anxious people!) might have in implementing his advices.
Share This Post
Related Posts
-
Walnuts vs Brazil Nuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing walnuts to Brazil nuts, we picked the walnuts.
Why?
Talking macros first, they are about equal in protein, carbs, fats, and fiber; their composition is almost identical in this regard. However, looking a little more closely at the fats, Brazil nuts have more than 2x the saturated fat, while walnuts have nearly 2x the polyunsaturated fat. So, we’ll declare the macros category a moderate win for walnuts.
The category of vitamins is not balanced; walnuts have more of vitamins A, B2, B3, B5, B6, B9, C, and choline, while Brazil nuts have more of vitamins B1 and E. A clear and easy win for walnuts.
The category of minerals is interesting, because of one mineral in particular. First let’s mention: walnuts have more iron and manganese, while Brazil nuts have more calcium, copper, magnesium, phosphorus, potassium, and selenium. Taken at face value, this is a clear win for Brazil nuts. However…
About that selenium… Specifically, it’s more than 391x higher, and a cup of Brazil nuts would give nearly 10,000x the recommended daily amount of selenium. Now, selenium is an essential mineral (needed for thyroid hormone production, for example), and at the RDA it’s good for good health. Your hair will be luscious and shiny. However, go much above that, and selenium toxicity becomes a thing, you may get sick, and it can cause your (luscious and shiny) hair to fall out. For this reason, it’s recommended to eat no more than 3–4 Brazil nuts per day.
There is one last consideration, and this is oxalates; walnuts are moderately high in oxalates (>50mg/100g) while Brazil nuts are very high in oxalates (>500mg/100g). This won’t affect most people at all, but if you have pre-existing kidney problems (including a history of kidney stones), you might want to go easy on oxalate-containing foods.
For most people, however, walnuts are a very healthy choice, and outshine Brazil nuts in most ways.
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Sunflower Seeds vs Sesame Seeds – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing sunflower seeds to sesame seeds, we picked the sunflower.
Why?
In moderation, both are very healthy. We say “in moderation” because they’re both about 50% fat and such fats, while vital for life, are generally best enjoyed in small portions. Of that fat, sunflower has the slightly better fat profile; they’re both mostly poly- and monounsaturated fats, but sunflower has 10% saturated fat while sesame has 15%. Aside from fats, sunflower has slightly more protein and sesame has slightly more carbs. While sesame has slightly more fiber, because of the carb profile sunflower still has the lower glycemic index. All in all, a moderate win for sunflower in the macros category.
You may be wondering, with all that discussion of fats, what they’re like for omega-3, and sesame seeds have more omega-3, though sunflower seeds contain it too. Still, a point in sesame’s favor here.
When it comes to vitamins, sunflower has more of vitamins A, B1, B2, B3, B5, B6, B9, C, E, and choline, while sesame is not higher in any vitamins.
In the category of minerals, sunflower has more phosphorus, potassium, and selenium, while sesame has more calcium, copper, iron, and zinc. This is nominally a marginal win for sesame, but it should be noted that sunflower is still very rich in copper, iron, and zinc too (but not calcium).
Adding up the categories makes for a moderate win for sunflower seeds, but as ever, enjoy both; diversity is best!
Want to learn more?
You might like to read:
Sunflower Seeds vs Pumpkin Seeds – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Yes, blue light from your phone can harm your skin. A dermatologist explains
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Social media is full of claims that everyday habits can harm your skin. It’s also full of recommendations or advertisements for products that can protect you.
Now social media has blue light from our devices in its sights.
So can scrolling on our phones really damage your skin? And will applying creams or lotions help?
Here’s what the evidence says and what we should really be focusing on.
Max kegfire/Shutterstock Remind me, what actually is blue light?
Blue light is part of the visible light spectrum. Sunlight is the strongest source. But our electronic devices – such as our phones, laptops and TVs – also emit it, albeit at levels 100-1,000 times lower.
Seeing as we spend so much time using these devices, there has been some concern about the impact of blue light on our health, including on our eyes and sleep.
Now, we’re learning more about the impact of blue light on our skin.
How does blue light affect the skin?
The evidence for blue light’s impact on skin is still emerging. But there are some interesting findings.
1. Blue light can increase pigmentation
Studies suggest exposure to blue light can stimulate production of melanin, the natural skin pigment that gives skin its colour.
So too much blue light can potentially worsen hyperpigmentation – overproduction of melanin leading to dark spots on the skin – especially in people with darker skin.
Blue light can worsen dark spots on the skin caused by overproduction of melanin. DUANGJAN J/Shutterstock 2. Blue light can give you wrinkles
Some research suggests blue light might damage collagen, a protein essential for skin structure, potentially accelerating the formation of wrinkles.
A laboratory study suggests this can happen if you hold your device one centimetre from your skin for as little as an hour.
However, for most people, if you hold your device more than 10cm away from your skin, that would reduce your exposure 100-fold. So this is much less likely to be significant.
3. Blue light can disrupt your sleep, affecting your skin
If the skin around your eyes looks dull or puffy, it’s easy to blame this directly on blue light. But as we know blue light affects sleep, what you’re probably seeing are some of the visible signs of sleep deprivation.
We know blue light is particularly good at suppressing production of melatonin. This natural hormone normally signals to our bodies when it’s time for sleep and helps regulate our sleep-wake cycle.
By suppressing melatonin, blue light exposure before bed disrupts this natural process, making it harder to fall asleep and potentially reducing the quality of your sleep.
The stimulating nature of screen content further disrupts sleep. Social media feeds, news articles, video games, or even work emails can keep our brains active and alert, hindering the transition into a sleep state.
Long-term sleep problems can also worsen existing skin conditions, such as acne, eczema and rosacea.
Sleep deprivation can elevate cortisol levels, a stress hormone that breaks down collagen, the protein responsible for skin’s firmness. Lack of sleep can also weaken the skin’s natural barrier, making it more susceptible to environmental damage and dryness.
Can skincare protect me?
The beauty industry has capitalised on concerns about blue light and offers a range of protective products such as mists, serums and lip glosses.
From a practical perspective, probably only those with the more troublesome hyperpigmentation known as melasma need to be concerned about blue light from devices.
This condition requires the skin to be well protected from all visible light at all times. The only products that are totally effective are those that block all light, namely mineral-based suncreens or some cosmetics. If you can’t see the skin through them they are going to be effective.
But there is a lack of rigorous testing for non-opaque products outside laboratories. This makes it difficult to assess if they work and if it’s worth adding them to your skincare routine.
What can I do to minimise blue light then?
Here are some simple steps you can take to minimise your exposure to blue light, especially at night when it can disrupt your sleep:
- use the “night mode” setting on your device or use a blue-light filter app to reduce your exposure to blue light in the evening
- minimise screen time before bed and create a relaxing bedtime routine to avoid the types of sleep disturbances that can affect the health of your skin
- hold your phone or device away from your skin to minimise exposure to blue light
- use sunscreen. Mineral and physical sunscreens containing titanium dioxide and iron oxides offer broad protection, including from blue light.
In a nutshell
Blue light exposure has been linked with some skin concerns, particularly pigmentation for people with darker skin. However, research is ongoing.
While skincare to protect against blue light shows promise, more testing is needed to determine if it works.
For now, prioritise good sun protection with a broad-spectrum sunscreen, which not only protects against UV, but also light.
Michael Freeman, Associate Professor of Dermatology, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: