What families should know about whooping cough
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What you need to know
- Whooping cough is a bacterial respiratory illness that can cause long-term symptoms and even death.
- Two types of vaccines protect against it: The DTap vaccine is given to babies and children up to 6 years old, while the Tdap vaccine is given to children 7 years and older and adults.
- If you or your child has symptoms of whooping cough, isolate them from vulnerable family members and seek treatment early to reduce the risk of serious illness.
Whooping cough, also called pertussis, is a highly contagious respiratory illness that’s particularly dangerous for babies. Cases are now at least four times as high as they were at this time last year. Fortunately, vaccines are extremely effective at preventing the disease across age groups.
Read on to learn about the symptoms and risks of whooping cough, who should get vaccinated, and what to do when symptoms appear.
What are the symptoms of whooping cough?
Early symptoms of whooping cough typically appear five to 10 days after exposure and may include a runny or stuffy nose, a low fever, and a mild cough. One to two weeks later, some people may experience extreme coughing fits that can cause shortness of breath, trouble sleeping, vomiting, fatigue, and rib fractures. These fits usually last one to six weeks, but they can last up to 10 weeks after infection.
About one in three babies under 1 year old who contract whooping cough require hospitalization, as they may experience life-threatening pauses in breathing (called apnea), pneumonia, and other complications. Children and adults who have asthma or are immunocompromised are also more likely to develop severe symptoms.
Which vaccines protect against whooping cough, and who is eligible?
Two types of vaccines protect against whooping cough: The DTap vaccine is given to babies and children up to 6 years old, while the Tdap vaccine is given to children 7 years and older and adults. Both vaccines protect against infections from diptheria, tetanus, and pertussis.
The Centers for Disease Control and Prevention recommends that pregnant people receive a single dose of the Tdap vaccine between 27 and 36 weeks of pregnancy, as this lowers the risk of whooping cough in babies younger than 2 months old by 78 percent.
Multiple doses are required for the best protection. Learn more about DTaP and Tdap vaccine schedules from the CDC, and talk to your health care provider about how many doses you and your children need.
What should families do when whooping cough symptoms appear?
If you or your child has symptoms of whooping cough, isolate the infected person from vulnerable family members. It’s also important to seek treatment early to reduce the risk of serious illness. Health care providers typically prescribe antibiotics to those recovering at home.
Over-the-counter cough and cold medicine is not recommended for children under 4 years old. However, limiting smoke, dust, and chemical fumes at home and using a humidifier can reduce coughing. If you are caring for someone with whooping cough who exhibits pauses in breathing or develops gray or blue skin, call 911 immediately.
For more information, talk to your health care provider.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why 7 Hours Sleep Is Not Enough
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How Sleep-Deprived Are You, Really?
This is Dr. Matthew Walker. He’s a neuroscientist and sleep specialist, and is the Director of the Center for Human Sleep Science at UC Berkeley’s Department of Psychology. He’s also the author of the international bestseller “Why We Sleep”.
What does he want us to know?
Sleep deprivation is more serious than many people think it is. After about 16 hours without sleep, the brain begins to fail, and needs more than 7 hours of sleep to “reset” cognitive performance.
Note: note “seven or more”, but “more than seven”.
After ten days with only 7 hours sleep (per day), Dr. Walker points out, the brain is as dysfunctional as it would be after going without sleep for 24 hours.
Here’s the study that sparked a lot of Dr. Walker’s work:
Importantly, in Dr. Walker’s own words:
❝Three full nights of recovery sleep (i.e., more nights than a weekend) are insufficient to restore performance back to normal levels after a week of short sleeping❞
~ Dr. Matthew Walker
See also: Why You Probably Need More Sleep
Furthermore: the sleep-deprived mind is unaware of how sleep-deprived it is.
You know how a drunk person thinks they can drive safely? It’s like that.
You do not know how sleep-deprived you are, when you are sleep-deprived!
For example:
❝(60.7%) did not signal sleepiness before a sleep fragment occurred in at least one of the four MWT trials❞
Source: Sleepiness is not always perceived before falling asleep in healthy, sleep-deprived subjects
Sleep efficiency matters
With regard to the 7–9 hours band for optimal health, Dr. Walker points out that the sleep we’re getting is not always the sleep we think we’re getting:
❝Assuming you have a healthy sleep efficiency (85%), to sleep 9 hours in terms of duration (i.e. to be a long-sleeper), you would need to be consistently in bed for 10 hours and 36 minutes a night. ❞
~ Dr. Matthew Walker
At the bottom end of that, by the way, doing the same math: to get only the insufficient 7 hours sleep discussed earlier, a with a healthy 85% sleep efficiency, you’d need to be in bed for 8 hours and 14 minutes per night.
The unfortunate implication of this: if you are consistently in bed for 8 hours and 14 minutes (or under) per night, you are not getting enough sleep.
“But what if my sleep efficiency is higher than 85%?”
It shouldn’t be.If your sleep efficiency is higher than 85%, you are sleep-deprived and your body is having to enforce things.
Want to know what your sleep efficiency is?
We recommend knowing this, by the way, so you might want to check out:
Head-To-Head Comparison of Google and Apple’s Top Sleep-Monitoring Apps
(they will monitor your sleep and tell you your sleep efficiency, amongst other things)
Want to know more?
You might like his book:
Why We Sleep: Unlocking the Power of Sleep and Dreams
…and/or his podcast:
…and for those who like videos, here’s his (very informative) TED talk:
Prefer text? Click here to read the transcript
Want to watch it, but not right now? Bookmark it for later
Enjoy!
Share This Post
-
Trout vs Haddock – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing trout to haddock, we picked the trout.
Why?
It wasn’t close.
In terms of macros, trout has more protein and more fat, although the fat is mostly healthy (some saturated though, and trout does have more cholesterol). This category could be a win for either, depending on your priorities. But…
When it comes to vitamins, trout has a lot more of vitamins A, B1, B2, B3, B5, B6, B12, C, D, and E, while haddock is not higher in any vitamins.
In the category of minerals, trout has more calcium, copper, iron, magnesium, potassium, and zinc, while haddock has slightly more selenium. Given that a 10oz portion of trout already contains 153% of the RDA of selenium, however, the same size portion of haddock having 173% of the RDA isn’t really a plus for haddock (especially as selenium can cause problems if we get too much). Oh, and haddock is also higher in sodium, but in industrialized countries, most people most of the time need less of that, not more.
On balance, the overwhelming nutritional density of trout wins the day.
Want to learn more?
You might like to read:
Farmed Fish vs Wild Caught: It Makes Quite A Difference!
Take care!
Share This Post
-
Cashew & Chickpea Balti
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to curries, the humble balti is perhaps the best when you don’t have all day to let something simmer. Filled with healthful spices, this one also comes complete with lots of fiber as well as healthy proteins and fats, with most of its calories coming from the nuts themselves, and the haricot paste base makes for a deliciously creamy curry without having to add anything unhealthy.
You will need
- 1 cup cashews, soaked in warm water for at least 5 minutes, and drained (if allergic, omit)
- 1 can chickpeas (keep the water)
- 1 can haricot beans (keep the water)
- 1 can crushed tomatoes
- 2 medium (or 3 small) red onions, sliced
- red or green chilis, quantity per your preference re heat, chopped
- ½ bulb garlic, crushed
- ½ oz fresh ginger, peeled and finely chopped
- 1 tbsp tomato paste
- 1 tbsp garam masala
- 1 tbsp ground coriander
- 1 tbsp black pepper, coarse ground
- 2 tsp turmeric
- 1 tsp mustard seeds (if allergic, omit)
- 1 tsp sweet cinnamon
- 1 tsp coriander seeds
- ½ tsp MSG or 1 tsp low-sodium salt
- Avocado oil, for frying (extra virgin olive-oil, or cold-pressed coconut oil, are fine alternatives)
- Garnish: handful fresh cilantro, chopped (or parsley, if you have the “cilantro tastes like soap” gene)
Method
(we suggest you read everything at least once before doing anything)
1) Heat a little oil in a large sauté pan (we’re going to need space to work; a large wok is traditional but a sauté pan is convenient), and add the garlic, ginger, mustard seeds, and coriander seeds, stirring for about 2 minutes, then add the onions and chilis, stirring for another 3 minutes. The onions and chilis won’t be fully cooked yet, but that’s fine, we just needed to get them started.
2) Add the crushed tomatoes, stirring them in, and when they get to temperature, turn the heat down to a simmer.
3) Add the chickpeas to the pan, but separately put the chickpea water into a high-speed blender.
4) Add the haricot beans, including the water they came in, to the high-speed blender, as well as the tomato paste and the remaining spices (including the MSG or salt), and blend on high until smooth. Add the curry paste (that’s what you’ve just made in the blender) to the pan, and stir in well.
5) Add the cashews, stirring in well. Taste, and adjust any spices if necessary for your liking. If the onions still aren’t fully cooked, let them simmer until they are, but it shouldn’t take long.
10almonds tip: if perchance you made it too spicy, you can add a little lime juice and the acidity will counteract the heat. Adding lemon juice, lime juice, or some kind of vinegar (depending on what works with the flavor profile of your recipe) is a good last resort to have up your sleeve for fixing a dish that got too spicy.
6) Add the garnish, and serve—we recommend serving it with our Tasty Versatile Rice, but any carb is fine.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Why You Should Diversify Your Nuts!
- Three Daily Servings of Beans?
- Cashew Nuts vs Coconut – Which is Healthier?
- What Matters Most For Your Heart?
- Our Top 5 Spices: How Much Is Enough For Benefits? ← we hit 5/5 again today!
Take care!
Share This Post
Related Posts
-
How do I handle it if my parent is refusing aged care? 4 things to consider
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s a shock when we realise our parents aren’t managing well at home.
Perhaps the house and garden are looking more chaotic, and Mum or Dad are relying more on snacks than nutritious meals. Maybe their grooming or hygiene has declined markedly, they are socially isolated or not doing the things they used to enjoy. They may be losing weight, have had a fall, aren’t managing their medications correctly, and are at risk of getting scammed.
You’re worried and you want them to be safe and healthy. You’ve tried to talk to them about aged care but been met with swift refusal and an indignant declaration “I don’t need help – everything is fine!” Now what?
Here are four things to consider.
1. Start with more help at home
Getting help and support at home can help keep Mum or Dad well and comfortable without them needing to move.
Consider drawing up a roster of family and friends visiting to help with shopping, cleaning and outings. You can also use home aged care services – or a combination of both.
Government subsidised home care services provide from one to 13 hours of care a week. You can get more help if you are a veteran or are able to pay privately. You can take advantage of things like rehabilitation, fall risk-reduction programs, personal alarms, stove automatic switch-offs and other technology aimed at increasing safety.
Call My Aged Care to discuss your options.
Is Mum or Dad OK at home?
Nadino/Shutterstock2. Be prepared for multiple conversations
Getting Mum or Dad to accept paid help can be tricky. Many families often have multiple conversations around aged care before a decision is made.
Ideally, the older person feels supported rather than attacked during these conversations.
Some families have a meeting, so everyone is coming together to help. In other families, certain family members or friends might be better placed to have these conversations – perhaps the daughter with the health background, or the auntie or GP who Mum trusts more to provide good advice.
Mum or Dad’s main emotional support person should try to maintain their relationship. It’s OK to get someone else (like the GP, the hospital or an adult child) to play “bad cop”, while a different person (such as the older person’s spouse, or a different adult child) plays “good cop”.
3. Understand the options when help at home isn’t enough
If you have maximised home support and it’s not enough, or if the hospital won’t discharge Mum or Dad without extensive supports, then you may be considering a nursing home (also known as residential aged care in Australia).
Every person has a legal right to choose where we live (unless they have lost capacity to make that decision).
This means families can’t put Mum or Dad into residential aged care against their will. Every person also has the right to choose to take risks. People can choose to continue to live at home, even if it means they might not get help immediately if they fall, or eat poorly. We should respect Mum or Dad’s decisions, even if we disagree with them. Researchers call this “dignity of risk”.
It’s important to understand Mum or Dad’s point of view. Listen to them. Try to figure out what they are feeling, and what they are worried might happen (which might not be rational).
Try to understand what’s really important to their quality of life. Is it the dog, having privacy in their safe space, seeing grandchildren and friends, or something else?
Older people are often understandably concerned about losing independence, losing control, and having strangers in their personal space.
Sometimes families prioritise physical health over psychological wellbeing. But we need to consider both when considering nursing home admission.
Research suggests going into a nursing home temporarily increases loneliness, risk of depression and anxiety, and sense of losing control.
Mum and Dad should be involved in the decision-making process about where they live, and when they might move.
Some families start looking “just in case” as it often takes some time to find the right nursing home and there can be a wait.
After you have your top two or three choices, take Mum or Dad to visit them. If this is not possible, take pictures of the rooms, the public areas in the nursing home, the menu and the activities schedule.
We should give Mum or Dad information about their options and risks so they can make informed (and hopefully better) decisions.
For instance, if they visit a nursing home and the manager says they can go on outings whenever they want, this might dispel a belief they are “locked up”.
Having one or two weeks “respite” in a home may let them try it out before making the big decision about staying permanently. And if they find the place unacceptable, they can try another nursing home instead.
You might need to have multiple conversations about aged care.
CGN089/Shutterstock4. Understand the options if a parent has lost capacity to make decisions
If Mum or Dad have lost capacity to choose where they live, family may be able to make that decision in their best interests.
If it’s not clear whether a person has capacity to make a particular decision, a medical practitioner can assess for that capacity.
Mum or Dad may have appointed an enduring guardian to make decisions about their health and lifestyle decisions when they are not able to.
An enduring guardian can make the decision that the person should live in residential aged care, if the person no longer has the capacity to make that decision themselves.
If Mum or Dad didn’t appoint an enduring guardian, and have lost capacity, then a court or tribunal can appoint that person a private guardian (usually a family member, close friend or unpaid carer).
If no such person is available to act as private guardian, a public official may be appointed as public guardian.
Deal with your own feelings
Families often feel guilt and grief during the decision-making and transition process.
Families need to act in the best interest of Mum or Dad, but also balance other caring responsibilities, financial priorities and their own wellbeing.
Lee-Fay Low, Professor in Ageing and Health, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Aspirin vs Cancer Metastasis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Aspirin is a bit of a mixed bag.
In the category of things in its favor, it’s a modest analgesic with few side effects from occasional use, so it’s a good option if you have a headache, for example.
Unless you’re already on blood thinners or having a bleeding disorder, in which case, aspirin is not the thing to reach for.
About aspirin and heart disease
This is actually a complicated one, and we covered it at length in a dedicated main feature. If you want a one-line summary, it’s “chronic low-dose aspirin use can lower overall CVD risk, but does not reduce CVD mortality or all-cause mortality, and you may pay for it with gastrointestinal bleeding, and increased risk of ulcers“.
For a more nuanced explanation, see: Aspirin, CVD Risk, & Potential Counter-Risks
On the other hand, if you are having a heart attack and are waiting for the ambulance that you already called, and have aspirin to hand that you don’t have to go looking for, then it can be good to take a dose then.
For more on that, see: How To Survive A Heart Attack When You’re Alone
There are more problems
In the case of chronic use of low-dose aspirin, not only does it increase the risks of bleeding, especially gastrointestinal bleeding, and ulcers, but also it increases the risk of anemia. Given that anemia also gives the symptom “dizziness”, this is also a significant threat for increasing the incidence of falls in the older population, too, which can of course lead to serious complications and ultimately death.
For the science about this, see: Low-Dose Aspirin & Anemia
Now, about aspirin and cancer metastasis
This one’s a point in aspirin’s favor.
Cancer is, in and of itself, obviously a big problem. In terms of when it’s most likely to kill someone, that is usually when the cancer becomes metastatic, that is to say, it has spread.
So, while preventing cancer and, failing that, killing cancer are very important goals, there is a third axis to cancer care, which is preventing metastasis in someone who has cancer.
And that’s what aspirin does. How, you ask?
Scientists found this one out by accident!
They were doing genetic research in mice, to find genes that had an effect on metastasis. In the process, they found a certain gene that instructs the creation of a certain protein, and mice that lacked that gene (and thus its associated protein) had less metastasis.
The protein in question suppresses T-cells, which are programmed to recognize and kill metastatic cancer cells (amongst having other great jobs; they are an important part of the immune system in general, and one that declines with aging; most people in their 60s or older are producing very few T-cells).
About that, see: Focusing On Health In Our Sixties
Tracing the cell signaling, the researchers found that the protein is activated when T-cells are exposed to thromboxane A2 (or TXA2 to its friends).
And TXA2? That’s produced by platelets, and aspirin works by inhibiting TXA2 production, effectively making platelets (and thus the blood as a whole) less sticky.
So, that’s quite a few steps in the process, but ultimately:
- Aspirin inhibits TXA2 production
- Lower TXA2 levels mean ARHGEF1 (that’s the protein) isn’t activated
- ARHGEF1 not being activated means T-cells are free to do their thing
- T-cells are now free to kill metastatic cancer cells
You can read the paper here:
Aspirin prevents metastasis by limiting platelet TXA2 suppression of T cell immunity
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
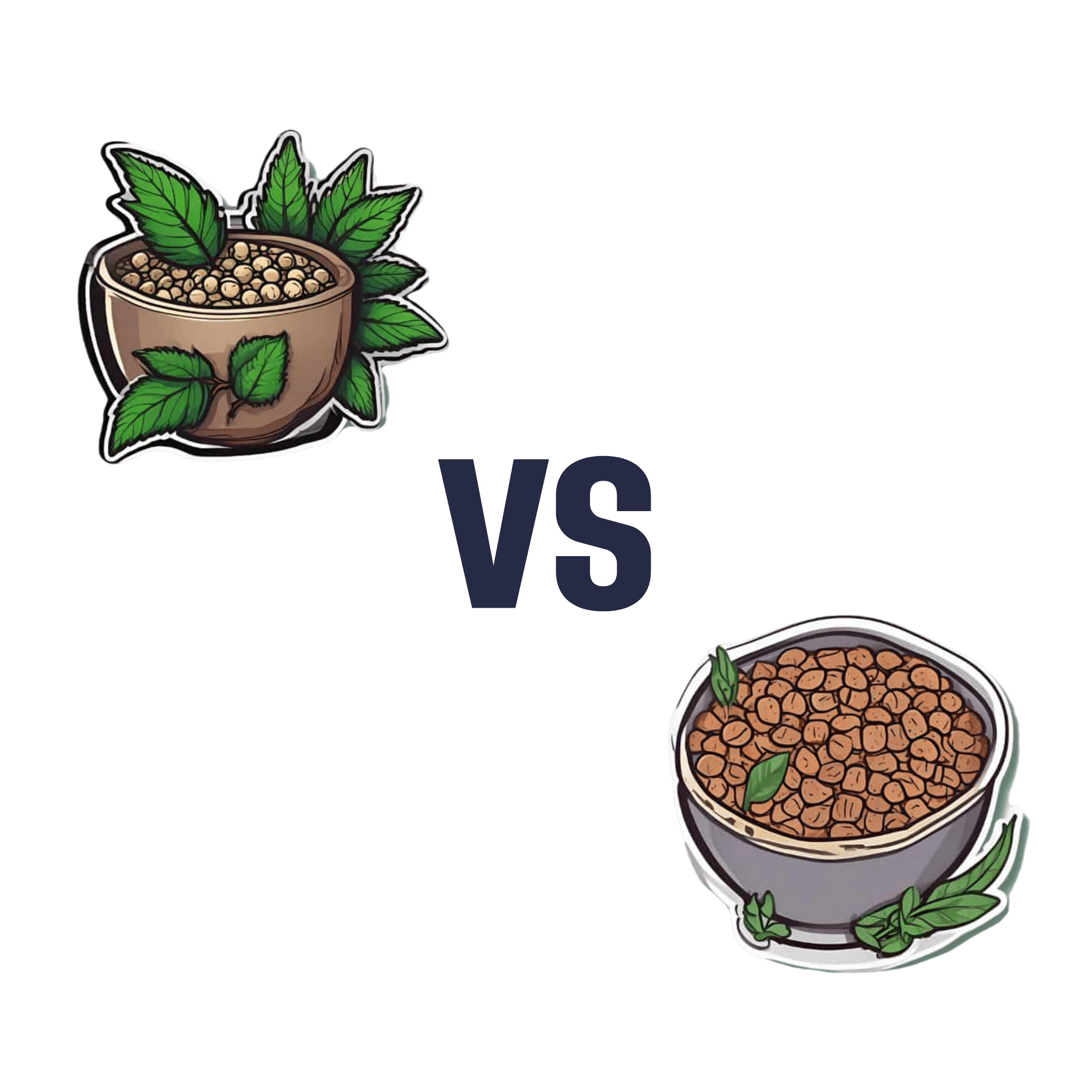
Hemp Seeds vs Flax Seeds – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing hemp seeds to flax seeds, we picked the flax.
Why?
Both are great, but quite differently so! In other words, they both have their advantages, but on balance, we prefer the flax’s advantages.
Part of this come from the way in which they are sold/consumed—hemp seeds must be hulled first, which means two things as a result:
- Flax seeds have much more fiber (about 8x more)
- Hemp seeds have more protein (about 2x more), proportionally, at least ← this is partly because they lost a bunch of weight by losing their fiber to the hulling, so the “per 100g” values of everything else go up, even though the amount per seed didn’t change
Since people’s diets are more commonly deficient in fiber than protein, and also since 8x is better than 2x, we consider this a win for flax.
Of course, many people enjoy hemp or flax specifically for the healthy fatty acids, so how do they stack up in that regard?
- Flax seeds have more omega-3s
- Hemp seeds have more omega-6s
This, for us, is a win for flax too, as the omega-3s are generally what we need more likely to be deficient in. Hemp enthusiasts, however, may argue that the internal balance of omega-3s to omega-6s is closer to an ideal ratio in hemp—but nutrition doesn’t exist in a vacuum, so we have to consider things “as part of a balanced diet” (because if one were trying to just live on hemp seeds, one would die), and most people’s diets are skewed far too far in favor or omega-6 compared to omega-3. So for most people, the higher levels of omega-3s are the more useful.
Want to learn more?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: