Cannellini Protein Gratin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A healthier twist on a classic, the protein here comes not only from the cannellini beans, but also from (at the risk of alienating French readers) a béchamel sauce that is not made using the traditional method involving flour and butter, but instead, has cashew protein as a major constituent.
You will need
- 3 medium potatoes, chopped (no need to peel them; you can if you want, but many of the nutrients are there and they’re not a problem for the recipe)
- 1 can cannellini beans (also called white kidney beans)
- 1 medium onion, chopped
- 2 stalks celery, sliced
- 1 carrot, chopped
- ½ bulb garlic, minced (or more, if you like)
- 1 jalapeño, chopped
- 2 tbsp tomato paste
- 1 tbsp chia seeds
- 2 tsp black pepper, coarse ground
- Extra virgin olive oil, for frying
For the béchamel sauce:
- ½ cup milk (we recommend a neutral-tasting plant milk, such as unsweetened soy, but go with your preference)
- ⅓ cup cashews, soaked in hot water for at least 5 minutes (longer is fine) and drained
- ¼ cup nutritional yeast
- 1 tsp garlic powder
- 1 tsp dried thyme
Method
(we suggest you read everything at least once before doing anything)
Note: it will be a bonus if you can use a pan that is good both for going on the hob and in the oven, such as a deep cast iron skillet, or a Dutch oven. If you don’t have something like that though, it’s fine, just use a sauté pan or similar, and then transfer to an oven dish for the oven part—we’ll mention this again when we get to it.
1) Preheat the oven to 250℉/175℃.
2) Heat the pan, adding some oil and then the oven; fry it for about 5 minutes, stirring often.
3) Add the potatoes, celery, carrot, garlic, and jalapeño, stirring for another 2 minutes.
4) Add the tomato paste, along with 1 cup water, the chia seeds, and the black pepper, and cook for a further 15 minutes, stirring occasionally as necessary.
5) Add the cannellini beans, and cook for another 15 minutes, stirring occasionally as necessary.
6) Blend all the ingredients for the béchamel sauce, processing it until it is smooth.
7) If you are using an oven-safe pan, pour the béchamel sauce over the bean mixture (don’t stir it; the sauce should remain on top) and transfer it to the oven. Don’t use a lid.
If you’re not using an oven safe pan, first transfer the bean mixture to an oven dish, then pour the béchamel sauce over the bean mixture (don’t stir it; the sauce should remain on top) and put it in the oven. Don’t use a lid.
8) Bake for about 15 minutes, or until turning golden-brown on top.
9) Serve! It can be enjoyed on its own, or with salad and/or rice. See also, our Tasty Versatile Rice Recipe.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- What Matters Most For Your Heart?
- The Many Health Benefits Of Garlic
- Easily Digestible Vegetarian Protein Sources
- Is Dairy Scary?
- Cashew Nuts vs Coconut – Which is Healthier?
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Great Cholesterol Myth, Revised and Expanded – by Dr. Jonny Bowden and Dr. Stephen Sinatra
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The topic of cholesterol, and saturated fat for that matter, is a complex and often controversial one. How does this book treat it?
With strong opinions, is how—but backed by good science. The authors, a nutritionist and a cardiologist, pull no punches about outdated and/or cherry-picked science, and instead make the case for looking at what, statistically speaking, appear to be the real strongest risk factors.
So, are they advocating for Dave Asprey-style butter-guzzling, or “the carnivore diet”? No, no they are not. Those things remain unhealthy, even if they give some short-term gains (of energy levels, weight loss, etc).
They do advocate, however, for enjoying saturated fats in moderation, and instead of certain polyunsaturated seed oils that do far worse. They also advocate strongly for avoiding sugar, stress, and (for different reasons) statins (in most people’s cases).
They also demystify in clear terms, and often with diagrams and infographics, the various kinds of fats and their components, broken down in far more detail than any other pop-science source this reviewer has seen.
Bottom line: if you want to take a scientific approach to heart health, this book can help you to focus on what will actually make the biggest difference.
Share This Post
-
Superfood Baked Apples
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Superfoods, and super-tasty. This is a healthy twist on a classic; your blood sugars will thank you for choosing this tasty sweet delight. It’s also packed with nutrients!
You will need
- 2 large firm baking apples, cored but not peeled
- 1/2 cup chopped walnuts
- 3 tbsp goji berries, rehydrated (soak them in warm water for 10–15minutes and drain)
- 1 tbsp honey, or maple syrup, per your preference (this writer is also a fan of aged balsamic vinegar for its strong flavor and much milder sweetness. If you don’t like things to be too sweet, this is the option for you)
- 2 tsp ground sweet cinnamon
- 1 tsp ground ginger
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 180℃ / 350℉ / gas mark 4
2) Mix the chopped walnuts with the goji berries and the honey (or whatever you used instead of the honey) as well as the sweet cinnamon and the ginger.
3) Place the apples in shallow baking dish, and use the mixture you just made to stuff their holes.
4) Add 1/2 cup water to the dish, around the apples. Cover gently with foil, and bake until soft.
Tip: check them every 20 minutes; they may be done in 40 or it may take 60; in honesty it depends on your oven. If unsure, cook them for longer at a lower temperature.
5) Serve warm.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- From Apples to Bees, and High-Fructose C’s
- Why You Should Diversify Your Nuts!
- Goji Berries: Which Benefits Do They Really Have?
- The Sugary Food That Lowers Blood Sugars
- Honey vs Maple Syrup – Which is Healthier?
- A Tale Of Two Cinnamons ← this is important, about why we chose the sweet cinnamon
- Ginger Does A Lot More Than You Think
Take care!
Share This Post
-
Longevity… Simplified – by Dr. Howard Luks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In the spirit of the book itself, we’ll keep this one simple:
The information in this book will not be new to regular readers of 10almonds, or at least, not if you’ve been with us for a while (because we can only cover so much per day, so long-time readers will have accumulated more knowledge).
On the other hand, the information is clear, correct, and very much stripped down to the most important basics. Not the very simplest basics, which would be an oversimplification to the point of inutility, but the most important basics.
To take an example, when it comes to exercise, he doesn’t say “exercise more” but rather that “a complete exercise program has four pillars: aerobic training, resistance training, balance training, and high-intensity interval training (HIIT)”, and then he goes about explaining, in clear and simple terms, how to do those.
The style is similar when it comes to diet, sleep, and body-part-specific chapters such as about heart health, brain health, and so forth.
Bottom line: if you’re a long-time 10almonds reader, you probably don’t need this one, but it’d be a great book for someone else who has expressed an interest in getting healthier, as it really is a top-tier “primer” in increasing health and healthspan.
Click here to check out Longevity… Simplified, and enjoy simplified longevity!
Share This Post
Related Posts
-
For Many Rural Women, Finding Maternity Care Outweighs Concerns About Abortion Access
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
BAKER CITY, Ore. — In what has become a routine event in rural America, a hospital maternity ward closed in 2023 in this small Oregon town about an hour from the Idaho border.
For Shyanne McCoy, 23, that meant the closest hospital with an obstetrician on staff when she was pregnant was a 45-mile drive away over a mountain pass.
When McCoy developed symptoms of preeclampsia last January, she felt she had the best chance of getting the care she needed at a larger hospital in Boise, Idaho, two hours away. She spent the final week of her pregnancy there, too far from home to risk leaving, before giving birth to her daughter.
Six months later, she said it seems clear to her that the health care needs of rural young women like her are largely ignored.
For McCoy and others, figuring out how to obtain adequate care to safely have a baby in Baker City has quickly eclipsed concerns about another medical service lacking in the area: abortion. But in Oregon and elsewhere in the country, progressive lawmakers’ attempts to expand abortion access sometimes clash with rural constituencies.
Oregon is considered one of the most protective states in the country when it comes to abortion. There are no legal limits on when someone can receive an abortion in the state, and the service is covered by its Medicaid system. Still, efforts to expand access in the rural, largely conservative areas that cover most of the state have encountered resistance and incredulity.
It’s a divide that has played out in elections in such states as Nevada, where voters passed a ballot measure in November that seeks to codify abortion protections in the state constitution. Residents in several rural counties opposed the measure.
In Oregon, during the months just before the Baker City closure was announced, Democratic state lawmakers were focused on a proposed pilot program that would launch two mobile reproductive health care clinics in rural areas. The bill specified that the van-based clinics would include abortion services.
State Rep. Christine Goodwin, a Republican from a southwestern Oregon district, called the proposal the “latest example” of urban legislators telling rural leaders what their communities need.
The mobile health clinic pilot was eventually removed from the bill that was under discussion. That means no new abortion options in Oregon’s Baker County — and no new state-funded maternity care either.
“I think if you expanded rural access in this community to abortions before you extended access to maternal health care, you would have an uprising on your hands,” said Paige Witham, 27, a member of the Baker County health care steering committee and the mother of two children, including an infant born in October.
A study published in JAMA in early December that examined nearly 5,000 acute care hospitals found that by 2022, 52% of rural hospitals lacked obstetrics care after more than a decade of unit closures. The health implications of those closures for young women, the population most likely to need pregnancy care, and their babies can be significant. Research has shown that added distance between a patient and obstetric care increases the likelihood the baby will be admitted to a neonatal intensive care unit, or NICU.
Witham said that while she does not support abortion, she believes the government should not “legislate it away completely.” She said that unless the government provides far more support for young families, like free child care and better mental health care, abortion should remain legal.
Conversations with a liberal school board member, a moderate owner of a timber company, members of Baker City’s Republican Party chapter, a local doula, several pregnant women, and the director of the Baker County Health Department — many of whom were not rigidly opposed to abortion — all turned up the same answer: No mobile clinics offering abortions here, please.
Kelle Osborn, a nurse supervisor for the Baker County Health Department, loved the idea of a mobile clinic that would provide education and birth control services to people in outlying areas. She was less thrilled about including abortion services in a clinic on wheels.
“It’s not something that should just be handed out from a mobile van,” she said of abortion services. She said people in her conservative rural county would probably avoid using the clinics for anything if they were understood to provide abortion services.
Both Osborn and Meghan Chancey, the health department’s director, said they would rank many health care priorities higher, including the need for a general surgeon, an ICU, and a dialysis clinic.
Nationally, reproductive health care services of all types tend to be limited for people in rural areas, even within states that protect abortion access. More than two-thirds of people in “maternity care deserts” — all of which are in rural counties — must drive more than a half-hour to get obstetric care, according to a 2024 March of Dimes report. For people in the Southern states where lawmakers installed abortion bans, abortion care can be up to 700 miles away, according to a data analysis by Axios.
Nathan Defrees grew up in Baker City and has practiced medicine here since 2017. He works for a family medicine clinic. If a patient asks about abortion, he provides information about where and how one can be obtained, but he doesn’t offer abortions himself.
“There’s not a lot of anonymity in small towns for physicians who provide that care,” he said. “Many of us aren’t willing to sacrifice the rest of our career for that.”
He also pointed to the small number of patients requesting the service locally. Just six people living in Baker County had an abortion in 2023, according to data from the Oregon Department of Public Health. Meanwhile, 125 residents had a baby that year.
A doctor with obstetric training living in another rural part of the state has chosen to quietly provide early-stage abortions when asked. The doctor, concerned for their family’s safety in the small, conservative town where they live, asked not to be identified.
The idea that better access to abortion is not needed in rural areas seems naive, the doctor said. People most in need of abortion often don’t have access to any medical service not already available in town, the doctor pointed out. The first patient the doctor provided an abortion for at the clinic was a meth user with no resources to travel or to manage an at-home medication abortion.
“It seemed entirely inappropriate for me to turn her away for care I had the training and the tools to do,” the doctor said.
Defrees said it has been easier for Baker County residents to get an abortion since the U.S. Supreme Court overturned Roe v. Wade.
A new Planned Parenthood clinic in Ontario, Oregon, 70 miles away in neighboring Malheur County, was built primarily to provide services to people from the Boise metro area, but it also created an option for many living in rural eastern Oregon.
Idaho is one of the 16 states with near-total bans on abortion. Like many states with bans, Idaho has struggled to maintain its already small fleet of fetal medicine doctors. The loss of regional expertise touches Baker City, too, Defrees said.
For example, he said, the treatment plan for women who have a desired pregnancy but need a termination for medical reasons is now far less clear. “It used to be those folks could go to Boise,” he said. “Now they can’t. That does put us in a bind.”
Portland is the next closest option for that type of care, and that means a 300-mile drive along a set of highways that can be treacherous in winter.
“It’s a lot scarier to be pregnant now in Baker City than it ever has been,” Defrees said.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
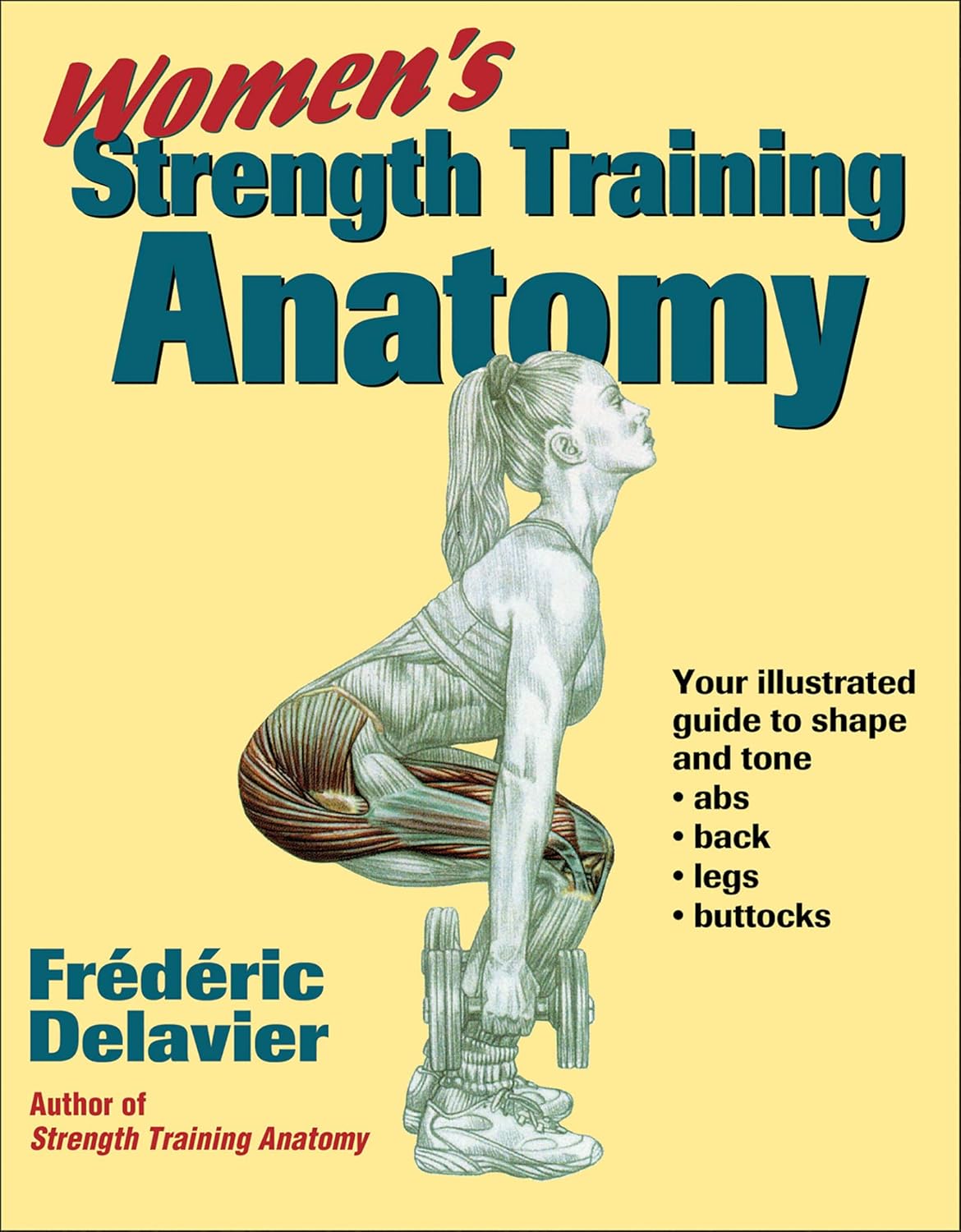
Women’s Strength Training Anatomy – by Frédéric Delavier
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fitness guides for women tend to differ from fitness guides for men, in the wrong ways:
“Do some squats and jumping jacks, and here’s a exercise for your abs; you too can look like our model here”
In those other books we are left wonder: where’s the underlying information? Where are the explanations that aren’t condescending? Where, dare we ask, is the understanding that a woman might ever lift something heavier than a baby?
Delavier, in contrast, delivers. With 130 pages of detailed anatomical diagrams for all kinds of exercises to genuinely craft your body the way you want it for you. Bigger here, smaller there, functional strength, you decide.
And rest assured: no, you won’t end up looking like Arnold Schwarzenegger unless you not only eat like him, but also have his genes (and possibly his, uh, “supplement” regime).
What you will get though, is a deep understanding of how to tailor your exercise routine to actually deliver the personalized and specific results that you want.
Pick Up Today’s Book on Amazon!
Not looking for a feminine figure? You may like the same author’s book for men:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ice Baths: To Dip Or Not To Dip?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
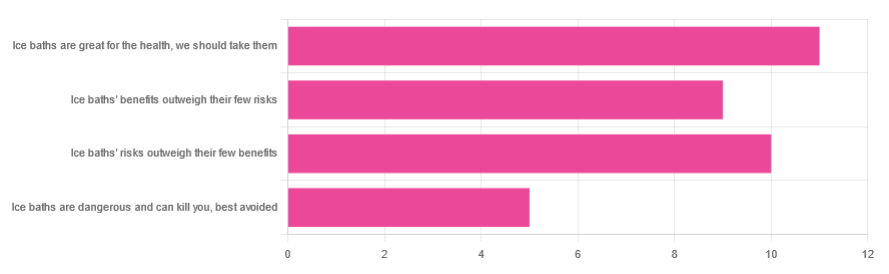
We asked you for your (health-related) view of ice baths, and got the above-depicted, below-described, set of responses:
- About 31% said “ice baths are great for the health; we should take them”
- About 29% said “ice baths’ risks outweigh their few benefits”
- About 26% said “ice baths’ benefits outweigh their few risks”
- About 14% said “ice baths are dangerous and can kill you; best avoided”
So what does the science say?
Freezing water is very dangerous: True or False?
True! Water close to freezing point is indeed very dangerous, and can most certainly kill you.
Fun fact, though: many such people are still saveable with timely medical intervention, in part because the same hypothermia that is killing them also slows down the process* of death
Source (and science) for both parts of that:
Cold water immersion: sudden death and prolonged survival
*and biologically speaking, death is a process, not an event, by the way. But we don’t have room for that today!
(unless you die in some sudden violent way, such as a powerful explosion that destroys your brain instantly; then it’s an event)
Ice baths are thus also very dangerous: True or False?
False! Assuming that they are undertaken responsibly and you have no chronic diseases that make it more dangerous for you.
What does “undertaken responsibly” mean?
Firstly, the temperature should not be near freezing. It should be 10–15℃, which for Americans is 50–59℉.
You can get a bath thermometer to check this, by the way. Here’s an example product on Amazon.
Secondly, your ice bath should last no more than 10–15 minutes. This is not a place to go to sleep.
What chronic diseases would make it dangerous?
Do check with your doctor if you have any doubts, as no list we make can be exhaustive and we don’t know your personal medical history, but the main culprits are:
- Cardiovascular disease
- Hypertension
- Diabetes (any type)
The first two are for heart attack risk; the latter is because diabetes can affect core temperature regulation.
Ice baths are good for the heart: True or False?
True or False depending on how they’re done, and your health before starting.
For most people, undertaking ice baths responsibly, repeated ice bath use causes the cardiovascular system to adapt to better maintain homeostasis when subjected to thermal shock (i.e. sudden rapid changes in temperature).
For example: Respiratory and cardiovascular responses to cold stress following repeated cold water immersion
And because that was a small study, here’s a big research review with a lot of data; just scroll to where it has the heading“Specific thermoregulative adaptations to regular exposure to cold air and/or cold water exposure“ for many examples and much discussion:
Health effects of voluntary exposure to cold water: a continuing subject of debate
Ice baths are good against inflammation: True or False?
True! Here’s one example:
Uric acid and glutathione levels (important markers of chronic inflammation) are also significantly affected:
Uric acid and glutathione levels during short-term whole body cold exposure
Want to know more?
That’s all we have room for today, but check out our previous “Expert Insights” main feature looking at Wim Hof’s work in cryotherapy:
A Cold Shower A Day Keeps The Doctor Away?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: