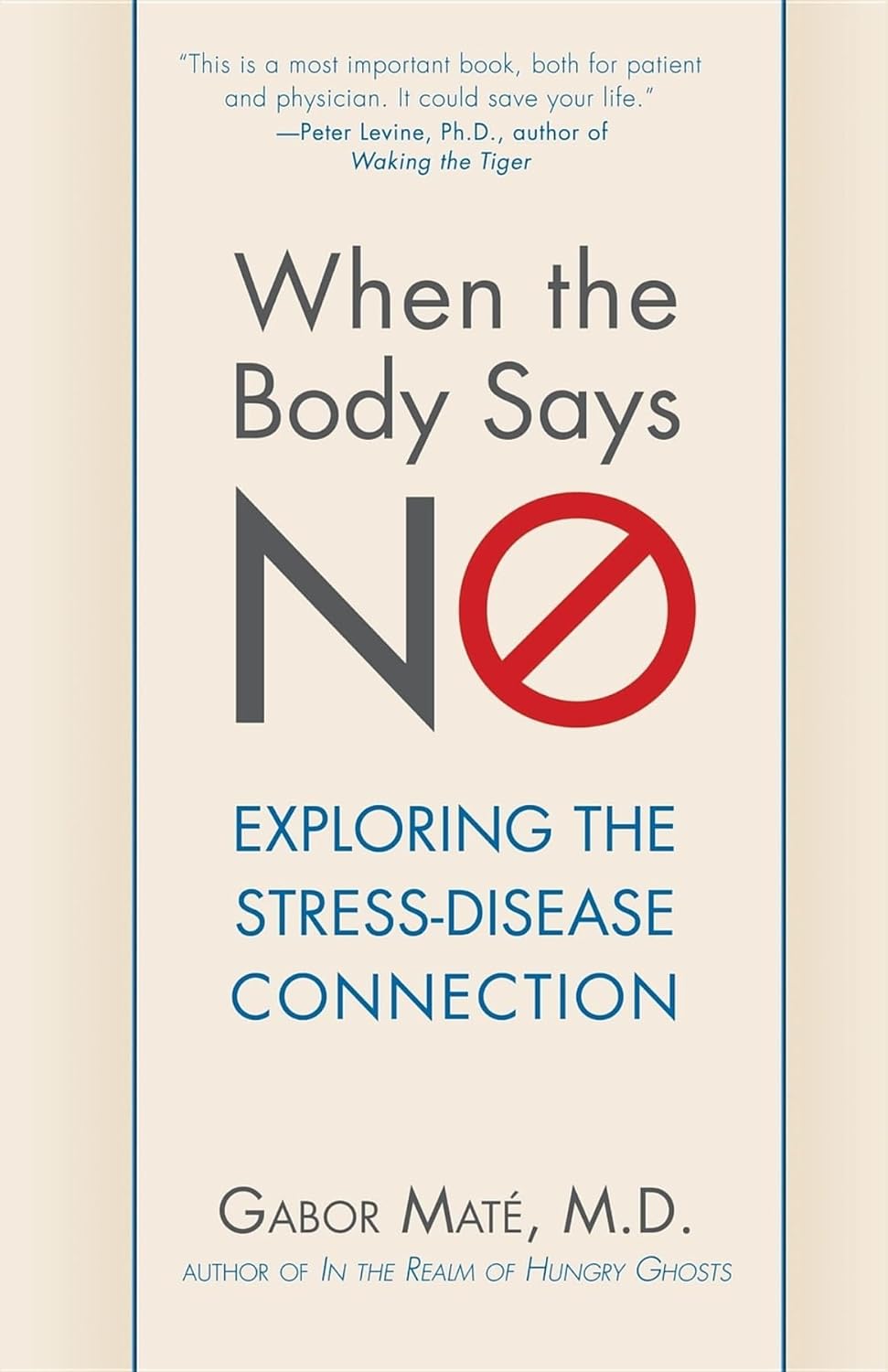
When the Body Says No – by Dr. Gabor Maté
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We know that chronic stress is bad for us because of what it does to our cortisol levels, so what is the rest of this book about?
Dr. Gabor Maté is a medical doctor, heavily specialized in the impact of psychological trauma on long term physical health.
Here, he examies—as the subtitle promises—the connection between stress and disease. As it turns out, it’s not that simple.
We learn not just about the impact that stress has on our immune system (including increasing the risk of autoimmune disorders like rheumatoid arthritis), the cardiovascular system, and various other critical systems fo the body… But also:
- how environmental factors and destructive coping styles contribute to the onset of disease, and
- how traumatic events can warp people’s physical perception of pain
- how certain illnesses are associated with particular personality types.
This latter is not “astrology for doctors”, by the way. It has more to do with what coping strategies people are likely to employ, and thus what diseases become more likely to take hold.
The book has practical advice too, and it’s not just “reduce your stress”. Ideally, of course, indeed reduce your stress. But that’s a) obvious b) not always possible. Rather, Dr. Maté explains which coping strategies result in the least prevalence of disease.
In terms of writing style, the book is very much easy-reading, but be warned that (ironically) this isn’t exactly a feel-good book. There are lot of tragic stories in it. But, even those are very much well-worth reading.
Bottom line: if you (and/or a loved one) are suffering from stress, this book will give you the knowledge and understanding to minimize the harm that it will otherwise do.
Click here to check out When The Body Says No, and take good care of yourself; you’re important!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Longevity… Simplified – by Dr. Howard Luks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In the spirit of the book itself, we’ll keep this one simple:
The information in this book will not be new to regular readers of 10almonds, or at least, not if you’ve been with us for a while (because we can only cover so much per day, so long-time readers will have accumulated more knowledge).
On the other hand, the information is clear, correct, and very much stripped down to the most important basics. Not the very simplest basics, which would be an oversimplification to the point of inutility, but the most important basics.
To take an example, when it comes to exercise, he doesn’t say “exercise more” but rather that “a complete exercise program has four pillars: aerobic training, resistance training, balance training, and high-intensity interval training (HIIT)”, and then he goes about explaining, in clear and simple terms, how to do those.
The style is similar when it comes to diet, sleep, and body-part-specific chapters such as about heart health, brain health, and so forth.
Bottom line: if you’re a long-time 10almonds reader, you probably don’t need this one, but it’d be a great book for someone else who has expressed an interest in getting healthier, as it really is a top-tier “primer” in increasing health and healthspan.
Click here to check out Longevity… Simplified, and enjoy simplified longevity!
Share This Post
-
Native Americans Have Shorter Life Spans. Better Health Care Isn’t the Only Answer.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
HISLE, S.D. — Katherine Goodlow is only 20, but she has experienced enough to know that people around her are dying too young.
Goodlow, a member of the Lower Brule Sioux Tribe, said she’s lost six friends and acquaintances to suicide, two to car crashes, and one to appendicitis. Four of her relatives died in their 30s or 40s, from causes such as liver failure and covid-19, she said. And she recently lost a 1-year-old nephew.
“Most Native American kids and young people lose their friends at a young age,” said Goodlow, who is considering becoming a mental health therapist to help her community. “So, I’d say we’re basically used to it, but it hurts worse every time we lose someone.”
Native Americans tend to die much earlier than white Americans. Their median age at death was 14 years younger, according to an analysis of 2018-21 data from the Centers for Disease Control and Prevention
The disparity is even greater in Goodlow’s home state. Indigenous South Dakotans who died between 2017 and 2021 had a median age of 58 — 22 years younger than white South Dakotans, according to state data.
Donald Warne, a physician who is co-director of the Johns Hopkins Center for Indigenous Health and a member of the Oglala Sioux Tribe, can rattle off the most common medical conditions and accidents killing Native Americans.
But what’s ultimately behind this low life expectancy, agree Warne and many other experts on Indigenous health, are social and economic forces. They argue that in addition to bolstering medical care and fully funding the Indian Health Service — which provides health care to Native Americans — there needs to be a greater investment in case management, parenting classes, and home visits.
“It’s almost blasphemy for a physician to say,” but “the answer to addressing these things is not hiring more doctors and nurses,” Warne said. “The answer is having more community-based preventions.”
The Indian Health Service funds several kinds of these programs, including community health worker initiatives, and efforts to increase access to fresh produce and traditional foods.
Private insurers and state Medicaid programs, including South Dakota’s, are increasingly covering such services. But insurers don’t pay for all the services and aren’t reaching everyone who qualifies, according to Warne and the National Academy for State Health Policy.
Warne pointed to Family Spirit, a program developed by the Johns Hopkins center to improve health outcomes for Indigenous mothers and children.
Chelsea Randall, the director of maternal and child health at the Great Plains Tribal Leaders’ Health Board, said community health workers educate Native pregnant women and connect them with resources during home visits.
“We can be with them throughout their pregnancy and be supportive and be the advocate for them,” said Randall, whose organization runs Family Spirit programs across seven reservations in the Dakotas, and in Rapid City, South Dakota.
The community health workers help families until children turn 3, teaching parenting skills, family planning, drug abuse prevention, and stress management. They can also integrate the tribe’s culture by, for example, using their language or birthing traditions.
The health board funds Family Spirit through a grant from the federal Health Resources and Services Administration, Randall said. Community health workers, she said, use some of that money to provide child car seats and to teach parents how to properly install them to counter high rates of fatal crashes.
Other causes of early Native American deaths include homicide, drug overdoses, and chronic diseases, such as diabetes, Warne said. Native Americans also suffer a disproportionate number of infant and maternal deaths.
The crisis is evident in the obituaries from the Sioux Funeral Home, which mostly serves Lakota people from the Pine Ridge Reservation and surrounding area. The funeral home’s Facebook page posts obituaries for older adults, but also for many infants, toddlers, teenagers, young adults, and middle-aged residents.
Misty Merrival, who works at the funeral home, blames poor living conditions. Some community members struggle to find healthy food or afford heat in the winter, she said. They may live in homes with broken windows or that are crowded with extended family members. Some neighborhoods are strewn with trash, including intravenous needles and broken bottles.
Seeing all these premature deaths has inspired Merrival to keep herself and her teenage daughter healthy by abstaining from drugs and driving safely. They also talk every day about how they’re feeling, as a suicide-prevention strategy.
“We’ve made a promise to each other that we wouldn’t leave each other like that,” Merrival said.
Many Native Americans live in small towns or on poor, rural reservations. But rurality alone doesn’t explain the gap in life expectancy. For example, white people in rural Montana live 17 years longer, on average, than Native Americans in the state, according to state data reported by Lee Enterprises newspapers.
Many Indigenous people also face racism or personal trauma from child or sexual abuse and exposure to drugs or violence, Warne said. Some also deal with generational trauma from government programs and policies that broke up families and tried to suppress Native American culture.
Even when programs are available, they’re not always accessible.
Families without strong internet connections can’t easily make video appointments. Some lack cars or gas money to travel to clinics, and public transportation options are limited.
Randall, the health board official, is pregnant and facing her own transportation struggles.
It’s a three-hour round trip between her home in the town of Pine Ridge and her prenatal appointments in Rapid City. Randall has had to cancel several appointments when family members couldn’t lend their cars.
Goodlow, the 20-year-old who has lost several loved ones, lives with seven other people in her mother’s two-bedroom house along a gravel road. Their tiny community on the Pine Ridge Reservation has homes and ranches but no stores.
Goodlow attended several suicide-prevention presentations in high school. But the programs haven’t stopped the deaths. One friend recently killed herself after enduring the losses of her son, mother, best friend, and a niece and nephew.
A month later, another friend died from a burst appendix at age 17, Goodlow said. The next day, Goodlow woke up to find one of her grandmother’s parakeets had died. That afternoon, she watched one of her dogs die after having seizures.
“I thought it was like some sign,” Goodlow said. “I started crying and then I started thinking, ‘Why is this happening to me?’”
Warne said the overall conditions on some reservations can create despair. But those same reservations, including Pine Ridge, also contain flourishing art scenes and language and cultural revitalization programs. And not all Native American communities are poor.
Warne said federal, state, and tribal governments need to work together to improve life expectancy. He encourages tribes to negotiate contracts allowing them to manage their own health care facilities with federal dollars because that can open funding streams not available to the Indian Health Service.
Katrina Fuller is the health director at Siċaŋġu Co, a nonprofit group on the Rosebud Reservation in South Dakota. Fuller, a member of the Rosebud Sioux Tribe, said the organization works toward “wicozani,” or the good way of life, which encompasses the physical, emotional, cultural, and financial health of the community.
Siċaŋġu Co programs include bison restoration, youth development, a Lakota language immersion school, financial education, and food sovereignty initiatives.
“Some people out here that are struggling, they have dreams, too. They just need the resources, the training, even the moral support,” Fuller said. “I had one person in our health coaching class tell me they just really needed someone to believe in them, that they could do it.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
Olive Oil vs Coconut Oil – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing extra virgin olive oil to cold-pressed coconut oil, we picked the olive oil.
Why?
While the cold-pressed coconut oil may offer some health benefits due to its lauric acid content, its 80–90% saturated fat content isn’t great for most people. It’s a great oil when applied topically for healthy skin and hair, though!
The extra virgin olive oil has a much more uncontroversially healthy blend of triglycerides, and (in moderation) is universally recognized as very heart-healthy.
Your local supermarket, most likely, has a good extra virgin olive oil, but if you’d like to get some online, here’s an example product on Amazon for your convenience.
Share This Post
Related Posts
-
Green Paneer Flatbreads
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
These are versatile little snacks that can be eaten alone or served as part of a buffet; great for warm summer nights!
You will need
- 1 lb block of paneer (you can also use our plant-based high-protein paneer recipe)
- 7 oz unsweetened yogurt (your choice what kind; plant-based is fine; live cultured is best)
- 1 tomato, thinly sliced
- ½ red onion, thinly sliced
- 2 oz spinach leaves
- 1 tbsp lime juice
- 1 tsp red chili powder
- 4 wholewheat flatbreads
And then the marinade:
- 3 oz spinach
- ½ bulb garlic
- 1 tsp cumin seeds
- 1 tsp coriander seeds
- 1 tsp chili flakes
- ½ tsp MSG or 1 tsp low-sodium salt (MSG being the preferable and healthier option)
- 2 tbsp extra virgin olive oil
- Juice of ½ lime
Method
(we suggest you read everything at least once before doing anything)
1) Blend the marinade ingredients in a blender.
2) Cut the paneer into long cuboid chapes (similar to fish fingers) and put them in a bowl. Pour ⅔ of the marinade over them, and gently mix to coat evenly.
3) Heat a ridged griddle pan, and when hot, add the paneer and cook for 1–2 minutes each side without stirring, jiggling, or doing anything other than turning once per uncooked side.
4) Combine the onion, tomato, spinach leaves, lime choice, and chili powder to make the salad.
5) Add the remaining marinade to the yogurt to make a green dip.
6) Toast your flatbreads under the grill.
5) Assemble, putting the paneer and salad with a spoonful of the dip on the flatbread, and serve:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- High-Protein Plant-Based Paneer
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Our Top 5 Spices: How Much Is Enough For Benefits?
- Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Apricots vs Plums – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing apricots to plums, we picked the apricots.
Why?
Both are great, but it wasn’t close!
In terms of macros, apricots have more fiber, protein, and carbs, with their fiber:carb ratio also giving them the lower glycemic index (although, as usual for any whole fruit, neither are going to give anyone metabolic disease). In any case, by the numbers, and especially for having more fiber, apricots win this category.
In the category of vitamins, apricots have more of vitamins A, B1, B2, B3, B5, B6, B7, B9, C, E, and choline, while plums have more vitamin K. A clear win for apricots.
When it comes to minerals, apricots have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while plums are not higher in any mineral. Another hands-down win for apricots.
Looking at polyphenols, both have an abundance of many, especially assorted flavanols, including quercetin. However, plums additionally have some anthocyanins (whence the color), so they get a marginal victory in this round.
Still, adding up the sections, it’s a 3:1 win for apricots. Of course, do enjoy either or both, though; diversity is good!
Want to learn more?
You might like:
Top 8 Fruits That Prevent & Kill Cancer
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
10 Ways To Delay Aging
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Dr. Colin Rose; he is a Senior Associate of the Royal Society of Medicine. He’s also a main contributor to EduScience, a program funded by the E.U. which is designed to enhance the teaching and learning of science in schools in Europe.
His most recent work has been about aging—and how to delay it. We also reviewed his latest book, here:
Delay Ageing – by Dr. Colin Rose
So, what does he want us to know? The key lies in his compilation of ten ways in which we age on a cellular level, and what we can to do slow each one of those:
Damage to DNA accumulates
While DNA can get damaged without any external stimulus to cause that, there are a lot of modifiable factors that we can do to reduce DNA damage. The list is easy: if it causes cancer, it causes aging.
Thus, check out: Stop Cancer 20 Years Ago
Cells become senescent
Our cells are replaced all the time; some sooner than others, but all of them at some point. The problem occurs when cells are outliving their usefulness. If a cell becomes completely immortal, that is cancer, but happily most don’t. Nevertheless, having senescent (aging) cells in the body means that those senescent cells are what get copied forwards by mitosis, and our DNA becomes like a photocopy of a tattered old photocopy of a tattered old photocopy. Which, needless to say, is not good for our health. So, the best thing to do is to kill them earlier:
Yes, really: Fisetin: The Anti-Aging Assassin
Mitochondria become dysfunctional
Without properly functional mitochondria, no living human cell can do its job properly.
Options: 7 Ways To Boost Mitochondrial Health To Fight Disease
Beneficial genes are switched off, harmful genes are on
It’s easy to think of our genes as being immutable, but epigenetics means that our environment (amongst other factors) can mean that our gene expression changes.
Imagine it this way: your genes are a set of instructions for your body. However, your body will act or not on those instructions, depending on other factors. Hormones often play a big part in this; for example sex hormones tell the body which set of genetic instructions to read (and thus what kind of body to build/rebuild), and cortisol or oxytocin can tell the body which set of contingency plans to activate or suppress (respectively). A milder example is gray hair; genes have the program for it, but many other factors inform the body when, if, and how to do it.
Of more concern when it comes to aging is what goes on with more critical systems, such as the brain, in which the aforementioned DNA damage can cause unhelpful instructions to get interpreted, resulting in epigenetic changes that in turn facilitate age-related degeneration.
As to what can be done, see : Klotho: Unzipping The Genes Of Aging?
Stem cells become exhausted
Stem cells can become different kinds of cells, and thus they’re very useful for maintaining a healthy body. However, they get depleted with age. We can slow down the rate of loss, though; for example, intermittent fasting can help:
Per Dr. Li’s 5 Ways To Beat Cancer (And Other Diseases)
And for more detail, see:
Doctor’s Tip: Regeneration (stem cells) — one of your body’s five defense systems
(complete with lists of foods to eat or avoid for stem cell health)
Cells fail to communicate properly
Cells need to talk to each other constantly, to continue doing their jobs. We are one big organism, after all, and not a haphazard colony of the countless cells that constitute such. However, cell signalling gets worse with age, which in turn precipitates others age-related problems. Fortunately, there are nutrients that can improve cellular communication.
For example: PS, We Love You ← this is about phosphatidylserine, also called “PS”
Telomeres become shorter
These protective caps on our DNA suffer the wear-and-tear so that our DNA doesn’t have to. However, as they get shorter, the DNA can start suffering damage. For this reason, telomere length is considered one of the most “Gold Standard” markers of cellular aging.
Here’s what can be done for that: The Stress Prescription (Against Aging!)
The body fails to sense nutritional intake properly
This is mostly about insulin signalling (though problems can occur in other systems too, but we only have so much room here), so it’s important to take care of that.
See: Turn Back The Clock On Insulin Resistance
Proteins accumulate errors
This is due to DNA damage, of course, but there are specific things that can reduce protein error accumulation; see for example:
A quick fix – preventing protein errors extends lifespan
See also: Rapamycin Can Slow Aging By 20% (But Watch Out)
The microbiome becomes unbalanced
We at 10almonds often mention that gut health affects pretty much every other kind of health, and it’s true for aging as well. So, take care of that microbiome!
Here’s a primer: Gut Health 101
Want to know more about delaying aging beyond the cellular level?
Check out: Age & Aging: What Can (And Can’t) We Do About It?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: