What’s the difference between period pain and endometriosis pain?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Menstruation, or a period, is the bleeding that occurs about monthly in healthy people born with a uterus, from puberty to menopause. This happens when the endometrium, the tissue that lines the inside of the uterus, is shed.
Endometriosis is a condition that occurs when endometrium-like tissue is found outside the uterus, usually within the pelvic cavity. It is often considered a major cause of pelvic pain.
Pelvic pain significantly impacts quality of life. But how can you tell the difference between period pain and endometriosis?

Periods and period pain
Periods involve shedding the 4-6 millimetre-thick endometrial lining from the inside of the uterus.
As the lining detaches from the wall of the uterus, the blood vessels which previously supplied the lining bleed. The uterine muscles contract, expelling the blood and crumbled endometrium.
The crumbled endometrium and blood mostly pass through the cervix and vagina. But almost everyone back-bleeds via their fallopian tubes into their pelvic cavity. This is known as “retrograde menstruation”.

The process of menstrual shedding is caused by inflammatory substances, which also cause nausea, vomiting, diarrhoea, headaches, aches, pains, dizziness, feeling faint, as well as stimulating pain receptors.
These inflammatory substances are responsible for the pain and symptoms in the week before a period and the first few days.
For women with heavy periods, their worst days of pain are usually the heaviest days of their period, coinciding with more cramps to expel clots and more retrograde bleeding.
Many women also have pain when they are releasing an egg from their ovary at the time of ovulation. Ovulation or mid-cycle pain can be worse in those who bleed more, as those women are more likely to bleed into the ovulation follicle.
Around 90% of adolescents experience period pain. Among these adolescents, 20% will experience such severe period pain they need time off from school and miss activities. These symptoms are too often normalised, without validation or acknowledgement.
What about endometriosis?
Many symptoms have been attributed to endometriosis, including painful periods, pain with sex, bladder and bowel-related pain, low back pain and thigh pain.
Other pain-related conditions such migraines and chronic fatigue have also been linked to endometriosis. But these other pain-related symptoms occur equally often in people with pelvic pain who don’t have endometriosis.

Repeated, significant period and ovulation pain can eventually lead some people to develop persistent or chronic pelvic pain, which lasts longer than six months. This appears to occur through a process known as central sensitisation, where the brain becomes more sensitive to pain and other sensory stimuli.
Central sensitisation can occur in people with persistent pain, independent of the presence or absence of endometriosis.
Eventually, many people with period and/or persistent pelvic pain will have an operation called a laparoscopy, which allows surgeons to examine organs in the pelvis and abdomen, and diagnose and treat endometriosis.
Yet only 50% of those with identical pain symptoms who undergo a laparoscopy will end up having endometriosis.
Endometriosis is also found in pain-free women. So we cannot predict who does and doesn’t have endometriosis from symptoms alone.
How is this pain managed?
Endometriosis surgery usually involves removing lesions and adhesions. But at least 30% of people return to pre-surgery pain levels within six months or have more pain than before.
After surgery, emergency department presentations for pain are unchanged and 50% have repeat surgery within a few years.
Suppressing periods using hormonal therapies (such as continuous oral contraceptive pills or progesterone-only approaches) can suppress endometriosis and reduce or eliminate pain, independent of the presence or absence of endometriosis.
Not every type or dose of hormonal medications suits everyone, so medications need to be individualised.
The current gold-standard approach to manage persistent pelvic pain involves a multidisciplinary team approach, with the aim of achieving sustained remission and improving quality of life. This may include:
- physiotherapy for pelvic floor and other musculoskeletal problems
- management of bladder and bowel symptoms
- support for self-managing pain
- lifestyle changes including diet and exercise
- psychological or group therapy, as our moods, stress levels and childhood events can affect how we feel and experience pain.
Whether you have period pain, chronic pelvic pain or pain you think is associated with endometriosis, if you feel pain, it’s real. If it’s disrupting your life, you deserve to be taken seriously and treated as the whole person you are.
Sonia R. Grover, Senior Research Fellow, Murdoch Children’s Research Institute; Clinical Professor of Gynaecology, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Power Vegan Meals – by Maya Sozer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book has inspired some of the recipes we’ve shared recently—we’ve invariably tweaked and in our opinion improved them, but the recipes are great as written too.
The recipes, of which there are 75, are all vegan, gluten-free, high protein, and high fiber. Some reviewers on Amazon have complained that the recipes are high-calorie, and they often are, but those calories are mostly from healthy fats, so we don’t think it’s a bad thing. Still, if you’re doing a strict calorie-controlled diet, this is probably not the one for you.
Another thing the recipes are is tasty without being unduly complicated, as well as being mostly free from obscure ingredients. This latter is a good thing not because obscure ingredients are inherently bad, but rather that it can be frustrating to read a recipe and find its star ingredient is a cup of perambulatory periannath that must be harvested from the west-facing slopes of Ithilien during a full moon, no substitutions.
The style and format is simple and clear with minimal overture, one recipe per double-page; picture on one side, recipe on the other; perfect for a kitchen reading-stand.
Bottom line: these recipes are for the most part very consistent with what we share here, and we recommend them, unless you’re looking for low-calorie options.
Click here to check out Power Vegan Meals, and power-up your vegan meals!
Share This Post
-
Your Brain Is Always Listening – by Dr. Daniel Amen
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are a lot of books on Cognitive Behavioral Therapy (CBT), so what makes this one different?
While many CBT books have a focus (as this one also does) on controlling Automatic Negative Thoughts (ANTs), this one stands out in two ways:
Firstly: Dr. Amen, a medical doctor and psychiatrist, looks not just as the thoughts and feelings side of things… but also the neurological underpinnings. This makes a difference because it gives a much more tangible handle on some of the problems that we might face.
We wouldn’t tell someone with Type 1 Diabetes that they are “just blaming their pancreas” for blood sugar woes. So what’s with the notion of “this person is just blaming their brain”? Why would be harder on ourselves (or others) for having amygdalae that are a little out of whack, or a sluggish prefrontal cortex, or an overactive anterior cingulate gyrus?
So, Dr. Amen’s understanding and insights help us look at how we can give those bits of brain what they need to perk them up or calm them down.
Secondly, rather than picture-perfect easily-solved neat-and-tidy made-up scenarios as illustrations, he uses real (messy, human) case studies.
This means that we get to see how the methods advised work in the case of, for example, a business executive who has a trauma response to public speaking, because at the age of 12 he had to stand in court and argue for why his father should not receive the death penalty.
Bottom line: if these methods can ease situations like that, maybe we can apply them usefully in our own lives, too.
Click here to check out Your Brain Is Always Listening, and take control of yours!
Share This Post
-
Is ADHD Being Over-Diagnosed For Cash?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is ADHD Being Systematically Overdiagnosed?
The BBC’s investigative “Panorama” program all so recently did a documentary in which one of their journalists—who does not have ADHD—went to three private clinics and got an ADHD diagnosis from each of them:
- The BBC documentary: Private ADHD Clinics Exposed (28 mins)
- Their “5 Minutes” version: ADHD Undercover: How I Was Misdiagnosed (6 mins)
So… Is it really a case of show up, pay up, and get a shiny new diagnosis?
The BBC Panorama producers cherry-picked 3 private providers, and during those clinical assessments, their journalist provided answers that would certainly lead to a diagnosis.
This was contrasted against a three-hour assessment with an NHS psychiatrist—something that rarely happens in the NHS. Which prompts the question…
How did he walk into a 3-hour psychiatrist assessment, when most people have to wait in long waiting lists for a much more cursory appointment first with assorted gatekeepers, before going on another long waiting list, for an also-much-shorter appointment with a psychiatrist?
That would be because the NHS psychiatrist was given advance notification that this was part of an investigation and would be filmed (the private clinics were not gifted the same transparency)
So, maybe just a tad unequal treatment!
In case you’re wondering, here’s what that very NHS psychiatrist had to say on the topic:
Is it really too easy to be diagnosed with ADHD?
(we’ll give you a hint—remember Betteridge’s Law!)
❝Since the documentary aired, I have heard from people concerned that GPs could now be more likely to question legitimate diagnoses.
But as an NHS psychiatrist it is clear to me that the root of this issue is not overdiagnosis.
Instead, we are facing the combined challenges of remedying decades of underdiagnosis and NHS services that were set up when there was little awareness of ADHD.❞
~ Dr. Mike Smith, Psychiatrist
The ADHD foundation, meanwhile, has issued its own response, saying:
❝We are disappointed that BBC Panorama has opted to broadcast a poorly researched, sensationalist piece of television journalism.❞
Share This Post
Related Posts
-
Taking A Trip Through The Evidence On Psychedelics
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
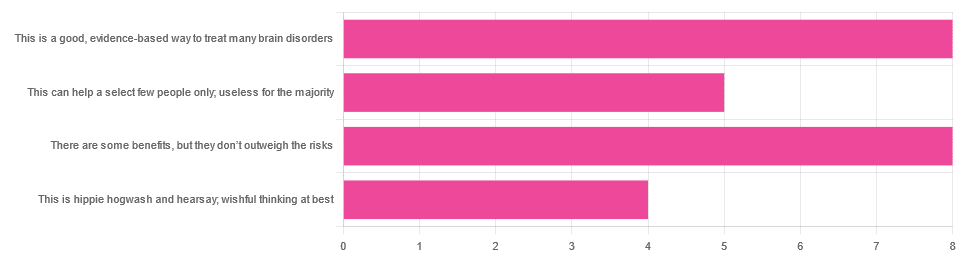
In Tuesday’s newsletter, we asked you for your opinions on the medicinal use of psychedelics, and got the above-depicted, below-described, set of responses:
- 32% said “This is a good, evidence-based way to treat many brain disorders”
- 32% said “There are some benefits, but they don’t outweigh the risks”
- 20% said “This can help a select few people only; useless for the majority”
- 16% said “This is hippie hogwash and hearsay; wishful thinking at best”
Quite a spread of answers, so what does the science say?
This is hippie hogwash and hearsay; wishful thinking at best! True or False?
False! We’re tackling this one first, because it’s easiest to answer:
There are some moderately-well established [usually moderate] clinical benefits from some psychedelics for some people.
If that sounds like a very guarded statement, it is. Part of this is because “psychedelics” is an umbrella term; perhaps we should have conducted separate polls for psilocybin, MDMA, ayahuasca, LSD, ibogaine, etc, etc.
In fact: maybe we will do separate main features for some of these, as there is a lot to say about each of them separately.
Nevertheless, looking at the spread of research as it stands for psychedelics as a category, the answers are often similar across the board, even when the benefits/risks may differ from drug to drug.
To speak in broad terms, if we were to make a research summary for each drug it would look approximately like this in each case:
- there has been research into this, but not nearly enough, as “the war on drugs” may well have manifestly been lost (the winner of the war being: drugs; still around and more plentiful than ever), but it did really cramp science for a few decades.
- the studies are often small, heterogenous (often using moderately wealthy white student-age population samples), and with a low standard of evidence (i.e. the methodology often has some holes that leave room for reasonable doubt).
- the benefits recorded are often small and transient.
- in their favor, though, the risks are also generally recorded as being quite low, assuming proper safe administration*.
*Illustrative example:
Person A takes MDMA in a club, dances their cares away, has had only alcohol to drink, sweats buckets but they don’t care because they love everyone and they see how we’re all one really and it all makes sense to them and then they pass out from heat exhaustion and dehydration and suffer kidney damage (not to mention a head injury when falling) and are hospitalized and could die;
Person B takes MDMA in a lab, is overwhelmed with a sense of joy and the clarity of how their participation in the study is helping humanity; they want to hug the researcher and express their gratitude; the researcher reminds them to drink some water.
Which is not to say that a lab is the only safe manner of administration; there are many possible setups for supervised usage sites. But it does mean that the risks are often as much environmental as they are risks inherent to the drug itself.
Others are more inherent to the drug itself, such as adverse cardiac events for some drugs (ibogaine is one that definitely needs medical supervision, for example).
For those who’d like to see numbers and clinical examples of the bullet points we gave above, here you go; this is a great (and very readable) overview:
NIH | Evidence Brief: Psychedelic Medications for Mental Health and Substance Use Disorders
Notwithstanding the word “brief” (intended in the sense of: briefing), this is not especially brief and is rather an entire book (available for free, right there!), but we do recommend reading it if you have time.
This can help a select few people only; useless for the majority: True or False?
True, technically, insofar as the evidence points to these drugs being useful for such things as depression, anxiety, PTSD, addiction, etc, and estimates of people who struggle with mental health issues in general is often cited as being 1 in 4, or 1 in 5. Of course, many people may just have moderate anxiety, or a transient period of depression, etc; many, meanwhile, have it worth.
In short: there is a very large minority of people who suffer from mental health issues that, for each issue, there may be one or more psychedelic that could help.
This is a good, evidence-based way to treat many brain disorders: True or False?
True if and only if we’re willing to accept the so far weak evidence that we discussed above. False otherwise, while the jury remains out.
One thing in its favor though is that while the evidence is weak, it’s not contradictory, insofar as the large preponderance of evidence says such therapies probably do work (there aren’t many studies that returned negative results); the evidence is just weak.
When a thousand scientists say “we’re not completely sure, but this looks like it helps; we need to do more research”, then it’s good to believe them on all counts—the positivity and the uncertainty.
This is a very different picture than we saw when looking at, say, ear candling or homeopathy (things that the evidence says simply do not work).
We haven’t been linking individual studies so far, because that book we linked above has many, and the number of studies we’d have to list would be:
n = number of kinds of psychedelic drugs x number of conditions to be treated
e.g. how does psilocybin fare for depression, eating disorders, anxiety, addiction, PTSD, this, that, the other; now how does ayahuasca fare for each of those, and so on for each drug and condition; at least 25 or 30 as a baseline number, and we don’t have that room.
But here are a few samples to finish up:
- Psilocybin as a New Approach to Treat Depression and Anxiety in the Context of Life-Threatening Diseases—A Systematic Review and Meta-Analysis of Clinical Trials
- Therapeutic Use of LSD in Psychiatry: A Systematic Review of Randomized-Controlled Clinical Trials
- Efficacy of Psychoactive Drugs for the Treatment of Posttraumatic Stress Disorder: A Systematic Review of MDMA, Ketamine, LSD and Psilocybin
- Changes in self-rumination and self-compassion mediate the effect of psychedelic experiences on decreases in depression, anxiety, and stress.
- Psychedelic Treatments for Psychiatric Disorders: A Systematic Review and Thematic Synthesis of Patient Experiences in Qualitative Studies
- Repeated lysergic acid diethylamide (LSD) reverses stress-induced anxiety-like behavior, cortical synaptogenesis deficits and serotonergic neurotransmission decline
In closing…
The general scientific consensus is presently “many of those drugs may ameliorate many of those conditions, but we need a lot more research before we can say for sure”.
On a practical level, an important take-away from this is twofold:
- drugs, even those popularly considered recreational, aren’t ontologically evil, generally do have putative merits, and have been subject to a lot of dramatization/sensationalization, especially by the US government in its famous war on drugs.
- drugs, even those popularly considered beneficial and potentially lifechangingly good, are still capable of doing great harm if mismanaged, so if putting aside “don’t do drugs” as a propaganda of the past, then please do still hold onto “don’t do drugs alone”; trained professional supervision is a must for safety.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Just Be Well – by Dr. Thomas Sult
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Firstly, what this is not: a “think yourself well” book. It’s not about just deciding to be well.
Rather, it’s about ensuring the foundations of wellness, from which the rest of good health can spring, and notably, an absence of chronic illness. In essence: enjoying chronic good health.
The prescription here is functional medicine, which stands on the shoulders of lifestyle medicine. This latter is thus briefly covered and the basics presented, but most of the book is about identifying the root causes of disease and eliminating them one by one, by taking into account the functions of the body’s processes, both in terms of pathogenesis (and thus, seeking to undermine that) and in terms of correct functioning (i.e., good health).
While the main focus of the book is on health rather than disease, he does cover a number of very common chronic illnesses, and how even in those cases where they cannot yet be outright cured, there’s a lot more that can be done for them than “take two of these and call your insurance company in the morning”, when the goal is less about management of symptoms (though that is also covered) and more about undercutting causes, and ensuring that even if one thing goes wrong, it doesn’t bring the entire rest of the system down with it (something that often happens without functional medicine).
The style is clear, simple, and written for the layperson without unduly dumbing things down.
Bottom line: if you would like glowingly good health regardless of any potential setbacks, this book can help your body do what it needs to for you.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Banana Bread vs Bagel – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing banana bread to bagel, we picked the bagel.
Why?
Unlike most of the items we compare in this section, which are often “single ingredient” or at least highly standardized, today’s choices are rather dependent on recipe. Certainly, your banana bread and your bagels may not be the same as your neighbor’s. Nevertheless, to compare averages, we’ve gone with the FDA’s Food Central Database for reference values, using the most default average recipes available. Likely you could make either or both of them a little healthier, but as it is, this is how we’ve gone about making it a fair comparison. With that in mind…
In terms of macros, bagels have more than 2x the protein and about 4x the fiber, while banana bread has slightly higher carbs and about 7x more fat. You may be wondering: are the fats healthy? And the answer is, it could be better, could be worse. The FDA recipe went with margarine rather than butter, which lowered the saturated fat to being only ¼ of the total fat (it would have been higher, had they used butter) whereas bagels have no saturated fat at all—which characteristic is quite integral to bagels, unless you make egg bagels, which is rather a different beast. All in all, the macros category is a clear win for bagels, especially when we consider the carb to fiber ratio.
In the category of vitamins, bagels have on average more vitamin B1, B3, B5, and B9, while banana bread has on average more of vitamins A and C. A modest win for bagels.
When it comes to minerals, bagels are the more nutrient dense with more copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while banana bread is not higher in any minerals. An obvious and easy win for bagels.
Closing thoughts: while the micronutrient profile quite possibly differs wildly from one baker to another, something that will probably stay more or less the same regardless is the carb to fiber ratio, and protein to fat. As a result, we’d weight the macros category as the more universally relevant. Bagels won in all categories today, as it happened, but it’s fairly safe to say that, on average, a baker who makes bagels and banana bread with the same levels of conscientiousness for health (or lack thereof) will tend to make bagels that are healthier than banana bread, based on the carb to fiber ratio, and the protein to fat ratio.
Enjoy!
Want to learn more?
You might like to read:
- Should You Go Light Or Heavy On Carbs?
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Wholewheat Bread vs Seeded White – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: