What’s the difference between miscarriage and stillbirth?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the difference? is a new editorial product that explains the similarities and differences between commonly confused health and medical terms, and why they matter.
Former US First Lady Michelle Obama revealed in her memoir she had a miscarriage. UK singer-songwriter and actor Lily Allen has gone on the record about her stillbirth.
Both miscarriage and stillbirth are sadly familiar terms for pregnancy loss. They can be traumatic life events for the prospective parents and family, and their impacts can be long-lasting. But the terms can be confused.
Here are some similarities and differences between miscarriage and stillbirth, and why they matter.

Let’s start with some definitions
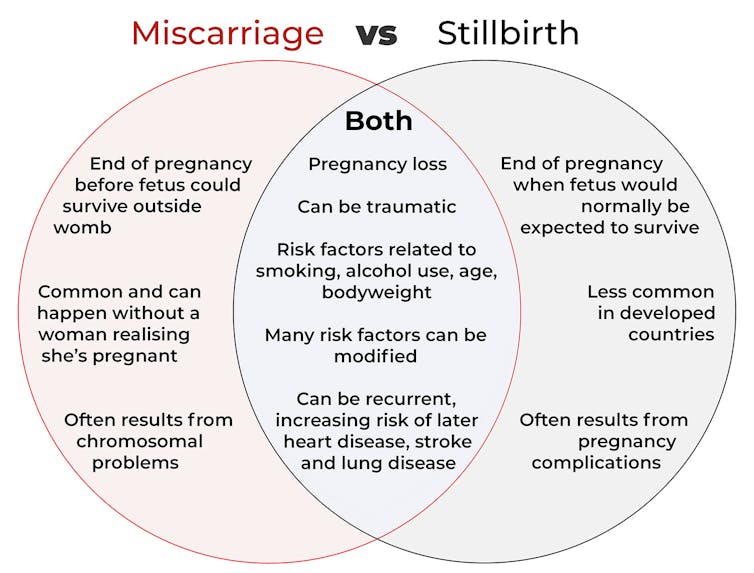
In broad terms, a miscarriage is when a pregnancy ends while the fetus is not yet viable (before it could survive outside the womb).
This is the loss of an “intra-uterine” pregnancy, when an embryo is implanted in the womb to then develop into a fetus. The term miscarriage excludes ectopic pregnancies, where the embryo is implanted outside the womb.
However, stillbirth refers to the end of a pregnancy when the fetus is normally viable. There may have been sufficient time into the pregnancy. Alternatively, the fetus may have grown large enough to be normally expected to survive, but it dies in the womb or during delivery.
The Australian Institute of Health and Welfare defines stillbirth as a fetal death of at least 20 completed weeks of gestation or with a birthweight of at least 400 grams.
Internationally, definitions of stillbirth vary depending on the jurisdiction.
How common are they?
It is difficult to know how common miscarriages are as they can happen when a woman doesn’t know she is pregnant. There may be no obvious symptoms or something that looks like a heavier-than-normal period. So miscarriages are likely to be more common than reported.
Studies from Europe and North America suggest a miscarriage occurs in about one in seven pregnancies (15%). More than one in eight women (13%) will have a miscarriage at some time in her life.
Around 1–2% of women have recurrent miscarriages. In Australia this is when someone has three or more miscarriages with no pregnancy in between.
Australia has one of the lowest rates of stillbirth in the world. The rate has been relatively steady over the past 20 years at 0.7% or around seven per 1,000 pregnancies.
Who’s at risk?
Someone who has already had a miscarriage or stillbirth has an increased risk of that outcome again in a subsequent pregnancy.
Compared with women who have had a live birth, those who have had a stillbirth have double the risk of another. For those who have had recurrent miscarriages, the risk of another miscarriage is four-fold higher.
Some factors have a u-shaped relationship, with the risk of miscarriage and stillbirth lowest in the middle.
For instance, maternal age is a risk factor for both miscarriage and stillbirth, especially if under 20 years old or older than 35. Increasing age of the male is only a risk factor for stillbirth, especially for fathers over 40.

Similarly for maternal bodyweight, women with a body mass index or BMI in the normal range have the lowest risk of miscarriage and stillbirth compared with those in the obese or underweight categories.
Lifestyle factors such as smoking and heavy alcohol drinking while pregnant are also risk factors for both miscarriage and stillbirth.
So it’s important to not only avoid smoking and alcohol while pregnant, but before getting pregnant. This is because early in the pregnancy, women may not know they have conceived and could unwittingly expose the developing fetus.
Why do they happen?
Miscarriage often results from chromosomal problems in the developing fetus. However, genetic conditions or birth defects account for only 7-14% of stillbirths.
Instead, stillbirths often relate directly to pregnancy complications, such as a prolonged pregnancy or problems with the umbilical cord.
Maternal health at the time of pregnancy is another contributing factor in the risk of both miscarriage and stillbirths.
Chronic diseases, such as high blood pressure, diabetes, hypothyroidism (underactive thyroid), polycystic ovary syndrome, problems with the immune system (such as an autoimmune disorder), and some bacterial and viral infections are among factors that can increase the risk of miscarriage.
Similarly mothers with diabetes, high blood pressure, and untreated infections, such as malaria or syphilis, face an increased risk of stillbirth.
In many cases, however, the specific cause of pregnancy loss is not known.
How about the long-term health risks?
Miscarriage and stillbirth can be early indicators of health issues later in life.
For instance, women who have had recurrent miscarriages or recurrent stillbirths are at higher risk of cardiovascular disease (such as heart disease or stroke).
Our research has also looked at the increased risk of stroke. Compared with women who had never miscarried, we found women with a history of three or more miscarriages had a 35% higher risk of non-fatal stroke and 82% higher risk of fatal stroke.
Women who had a stillbirth had a 31% higher risk of a non-fatal stroke, and those who had had two or more stillbirths were at a 26% higher risk of a fatal stroke.
We saw similar patterns in chronic obstructive pulmonary disease or COPD, a progressive lung disease with respiratory symptoms such as breathlessness and coughing.
Our data showed women with a history of recurrent miscarriages or stillbirths were at a 36% or 67% higher risk of COPD, respectively, even after accounting for a history of asthma.

Why is all this important?
Being well-informed about the similarities and differences between these two traumatic life events may help explain what has happened to you or a loved one.
Where risk factors can be modified, such as smoking and obesity, this information can be empowering for individuals who wish to reduce their risk of miscarriage and stillbirth and make lifestyle changes before they become pregnant.
More information and support about miscarriage and stillbirth is available from SANDS and Pink Elephants.
Gita Mishra, Professor of Life Course Epidemiology, Faculty of Medicine, The University of Queensland; Chen Liang, PhD student, reproductive history and non-communicable diseases in women, The University of Queensland, and Jenny Doust, Clinical Professorial Research Fellow, School of Public Health, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
An Unexpected Extra Threat Of Alcohol
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If You Could Use Some Exotic Booze…
…then for health reasons, we’re going to have to say “nay”.
We’ve written about alcohol before, and needless to say, it’s not good:
(the answer is “no, we cannot”)
In fact, the WHO (which unlike government regulatory bodies setting “safe” limits on drinking, makes no profit from taxes on alcohol sales) has declared that “the only safe amount of alcohol is zero”:
WHO: No level of alcohol consumption is safe for our health
Up there, where the air is rarefied…
If you’re flying somewhere this summer (Sinatra-style flying honeymoon or otherwise), you might want to skip the alcohol even if you normally do imbibe, because:
❝…even in young and healthy individuals, the combination of alcohol intake with sleeping under hypobaric conditions poses a considerable strain on the cardiac system and might lead to exacerbation of symptoms in patients with cardiac or pulmonary diseases.
These effects might be even greater in older people; cardiovascular symptoms have a prevalence of 7% of inflight medical emergencies, with cardiac arrest causing 58% of aircraft diversions.❞
Source: Alcohol plus cabin pressure at higher altitude may threaten sleeping plane passengers’ heart health
The experiment divided subjects into a control group and a study group; the study group were placed in simulated cabin pressure as though at altitude, which found, when giving some of them two small(we’re talking the kind given on flights) alcoholic drinks:
❝The combination of alcohol and simulated cabin pressure at cruising altitude prompted a fall in SpO2 to an average of just over 85% and a compensatory increase in heart rate to an average of nearly 88 beats/minute during sleep.❞
In contrast, that was 77 beats/minute for those who had alcohol but weren’t at altitude pressure, or 64 beats/minute for those who neither drank nor were at altitude pressure.
Lots more metrics were recorded and the study is interesting to read; if you’ve ever slept on a plane and thought “that sleep was not restful at all”, then know: it wasn’t just the seat’s fault, nor the engine, nor the recycled nature of the air—it was the reduced pressure causing hypoxia (defined as having oxygen levels lower than the healthy clinical norm of 90%) and almost halving your sleep’s effectiveness for a less than 10% drop in available oxygen in the blood (the sleepers not at altitude pressure averaged 96% SpO2, compared to the 85% at altitude).
We say “almost halving” because the deep sleep phase of sleep was reduced from 84 minutes (control) to 67.5 minutes at altitude without alcohol, or 46.5 minutes at altitude with alcohol.
Again, this was a pressure cabin in a lab—so this wasn’t about the other conditions of an airplane (seats, engine hundreds of other people, etc).
Which means: in an actual airplane it’s probably even worse.
Oh, and the study participants? All healthy individuals aged 18–40, so again probably worse for those older (or younger) than that range, or with existing health conditions!
Want to know more?
You can read the study in full here:
Want to drop the drink at any altitude? Check out:
Want to get that vacation feel without alcohol? You’re going to love:
Mocktails – by Moira Clark (book)
Enjoy!
Share This Post
-
Make Overnight Oats Shorter Or Longer For Different Benefits!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝How long do I have to soak oats for to get the benefits of “overnight oats”?❞
The primary benefit of overnight oats (over cooked oats) is that they are soft enough to eat without having been cooked (as cooking increases their glycemic index).
So, if it’s soft, it’s good to eat. A few hours should be sufficient.
Bonus information
If, by the way, you happen to leave oats and milk (be it animal or plant milk) sealed in a jar at room temperature for a 2–3 days (less if your “room temperature” is warmer than average), it will start to ferment.
- Good news: fermentation can bring extra health benefits!
- Bad news: you’re on your own if something pathogenic is present
For more on this, you might like to read:
Enjoy!
Share This Post
-
ADHD For Smart Ass Women – by Tracy Otsuka
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed books about ADHD in adults before, what makes this one different? It’s the wholly female focus. Which is not to say some things won’t apply to men too, they will.
But while most books assume a male default unless it’s “bikini zone” health issues, this one is written by a woman for women focusing on the (biological and social) differences in ADHD for us.
A strength of the book is that it neither seeks to:
- over-medicalize things in a way that any deviation from the norm is inherently bad and must be fixed, nor
- pretend that everything’s a bonus, that we are superpowered and beautiful and perfect and capable and have no faults that might ever need addressing actually
…instead, it gives a good explanation of the ins and outs of ADHD in women, the strengths and weaknesses that this brings, and good solid advice on how to play to the strengths and reduce (or at least work around) the weaknesses.
Bottom line: this book has been described as “ADHD 2.0 (a very popular book that we’ve reviewed previously), but for women”, and it deserves that.
Click here to check out ADHD for Smart Ass Women, and fall in love with your neurodivergent brain!
Share This Post
Related Posts
-
When Carbs, Proteins, & Fats Switch Metabolic Roles
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Strange Things Happening In The Islets Of Langerhans
It is generally known and widely accepted that carbs have the biggest effect on blood sugar levels (and thus insulin response), fats less so, and protein least of all.
And yet, there was a groundbreaking study published yesterday which found:
❝Glucose is the well-known driver of insulin, but we were surprised to see such high variability, with some individuals showing a strong response to proteins, and others to fats, which had never been characterized before.
Insulin plays a major role in human health, in everything from diabetes, where it is too low*, to obesity, weight gain and even some forms of cancer, where it is too high.
These findings lay the groundwork for personalized nutrition that could transform how we treat and manage a range of conditions.❞
*saying ”too low” here is potentially misleading without clarification; yes, Type 1 Diabetics will have too little [endogenous] insulin (because the pancreas is at war with itself and thus isn’t producing useful quantities of insulin, if any). Type 2, however, is more a case of acquired insulin insensitivity, because of having too much at once too often, thus the body stops listening to it, “boy who cried wolf”-style, and the pancreas also starts to get fatigued from producing so much insulin that’s often getting ignored, and does eventually produce less and less while needing more and more insulin to get the same response, so it can be legitimately said “there’s not enough”, but that’s more of a subjective outcome than an objective cause.
Back to the study itself, though…
What they found, and how they found it
Researchers took pancreatic islets from 140 heterogenous donors (varied in age and sex; ostensibly mostly non-diabetic donors, but they acknowledge type 2 diabetes could potentially have gone undiagnosed in some donors*) and tested cell cultures from each with various carbs, proteins, and fats.
They found the expected results in most of the cases, but around 9% responded more strongly to the fats than the carbs (even more strongly than to glucose specifically), and even more surprisingly 8% responded more strongly to the proteins.
*there were also some known type 2 diabetics amongst the donors; as expected, those had a poor insulin response to glucose, but their insulin response to proteins and fats were largely unaffected.
What this means
While this is, in essence, a pilot study (the researchers called for larger and more varied studies, as well as in vivo human studies), the implications so far are important:
It appears that, for a minority of people, a lot of (generally considered very good) antidiabetic advice may not be working in the way previously understood. They’re going to (for example) put fat on their carbs to reduce the blood sugar spike, which will technically still work, but the insulin response is going to be briefly spiked anyway, because of the fats, which very insulin response is what will lower the blood sugars.
In practical terms, there’s not a lot we can do about this at home just yet—even continuous glucose monitors won’t tell us precisely, because they’re monitoring glucose, not the insulin response. We could probably measure everything and do some math and work out what our insulin response has been like based on the pace of change in blood sugar levels (which won’t decrease without insulin to allow such), but even that is at best grounds for a hypothesis for now.
Hopefully, more publicly-available tests will be developed soon, enabling us all to know our “insulin response type” per the proteome predictors discovered in this study, rather than having to just blindly bet on it being “normal”.
Ironically, this very response may have hidden itself for a while—if taking fats raised insulin response without raising blood sugar levels, then if blood sugar levels are the only thing being measured, all we’ll see is “took fats at dinner; blood sugars returned to normal more quickly than when taking carbs without fats”.
You can read the study in full here:
Proteomic predictors of individualized nutrient-specific insulin secretion in health and disease
Want to know more about blood sugar management?
You might like to catch up on:
- 10 Ways To Balance Your Blood Sugars
- Track Your Blood Sugars For Better Personalized Health
- How To Turn Back The Clock On Insulin Resistance
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Calm Your Inflammation – by Dr. Brenda Tidwell
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The book starts with an overview of inflammation, both acute and chronic, before diving into how to reduce the latter kind (acute inflammation being usually necessary and helpful, usually fighting disease rather than creating it).
The advice in the book is not just dietary, and covers lifestyle interventions too, including exercise etc—and how to strike the right balance, since the wrong kind of exercise or too much of it can sabotage our efforts. Similarly, Dr. Tidwell doesn’t just say such things as “manage stress” but also provides 10 ways of doing so, and so forth for other vectors of inflammation-control. She does cover dietary things as well though, including supplements where applicable, and the role of gut health, sleep, and other factors.
The style of the book is quite entry-level pop-science, designed to be readable and comprehensible to all, without unduly dumbing-down. In terms of hard science or jargon, there are 6 pages of bibliography and 3 pages of glossary, so it’s neither devoid of such nor overwhelmed by it.
Bottom line: if fighting inflammation is a priority for you, then this book is an excellent primer.
Click here to check out Calm Your Inflammation, and indeed calm your inflammation!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Vagus Nerve (And How You Can Make Use Of It)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Vagus Nerve: The Brain-Gut Highway
The longest cranial nerve is the vagus nerve; it runs all the way from your brain to your colon. It’s very important, and (amongst other tasks) it largely regulates your parasympathetic nervous system, and autonomous functions like:
- Breathing
- Heart rate
- Vasodilation & vasoconstriction
- Blood pressure
- Reflex actions (e.g. coughing, sneezing, swallowing, vomiting, hiccuping)
That’s great, but how does knowing about it help us?
Because of vagal maneuvers! This means taking an action to stimulate the vagus nerve, and prompt it to calm down various bodily functions that need calming down. This can take the form of:
- Massage
- Electrostimulation
- Diaphragmatic breathing
Massage is perhaps the simplest; “vagus” means “wandering”, and the nerve is accessible in various places, including behind the ears. That’s the kind of thing that’ easier to show than tell, though, so we’ll include a video at the end.
Electrostimulation is the fanciest, and has been used to treat migraines and cluster headaches. Check out, for example:
Update on noninvasive neuromodulation for migraine treatment-Vagus nerve stimulation
Diaphragmatic breathing means breathing from the diaphragm—the big muscular tissue that sits under your lungs. You might know it as “abdominal breathing”, and refers to breathing “to the abdomen” rather than merely to the chest.
Even though your lungs are obviously in your chest not your abdomen, breathing with a focus on expanding the abdomen (rather than the chest) when breathing in, will result in much deeper breathing as the diaphragm allows the lungs to fill downwards as well as outwards.
Why this helps when it comes to the vagus nerve is simply that the vagus nerve passes by the diaphragm, such that diaphragmatic breathing will massage the vagus nerve deep inside your body.
More than just treating migraines
Vagus nerve stimulation has also been researched and found potentially helpful for managing:
- Depression, inflammation, and heart disease
- Diabetes and glycemic issues in general
- Multiple sclerosis and autoimmune disease in general
- Alzheimer’s disease and dementia in general
- Rheumatoid arthritis (we already mentioned inflammation and autoimmune diseases, but this is an interesting paper so we included it)
All this is particularly important as we get older, because vagal response reduces with age, and vagus nerve stimulation, which improves vagal tone, makes it easier not just to manage the aforementioned maladies, but also simply to relax more easily and more deeply.
See: Influence of age and gender on autonomic regulation of heart
We promised a video for the massage, so here it is:
! Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: