What’s the difference between a heart attack and cardiac arrest? One’s about plumbing, the other wiring
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In July 2023, rising US basketball star Bronny James collapsed on the court during practice and was sent to hospital. The 18-year-old athlete, son of famous LA Lakers’ veteran LeBron James, had experienced a cardiac arrest.
Many media outlets incorrectly referred to the event as a “heart attack” or used the terms interchangeably.
A cardiac arrest and a heart attack are distinct yet overlapping concepts associated with the heart.
With some background in how the heart works, we can see how they differ and how they’re related.

Understanding the heart
The heart is a muscle that contracts to work as a pump. When it contracts it pushes blood – containing oxygen and nutrients – to all the tissues of our body.
For the heart muscle to work effectively as a pump, it needs to be fed its own blood supply, delivered by the coronary arteries. If these arteries are blocked, the heart muscle doesn’t get the blood it needs.
This can cause the heart muscle to become injured or die, and results in the heart not pumping properly.
Heart attack or cardiac arrest?
Simply put, a heart attack, technically known as a myocardial infarction, describes injury to, or death of, the heart muscle.
A cardiac arrest, sometimes called a sudden cardiac arrest, is when the heart stops beating, or put another way, stops working as an effective pump.
In other words, both relate to the heart not working as it should, but for different reasons. As we’ll see later, one can lead to the other.
Why do they happen? Who’s at risk?
Heart attacks typically result from blockages in the coronary arteries. Sometimes this is called coronary artery disease, but in Australia, we tend to refer to it as ischaemic heart disease.
The underlying cause in about 75% of people is a process called atherosclerosis. This is where fatty and fibrous tissue build up in the walls of the coronary arteries, forming a plaque. The plaque can block the blood vessel or, in some instances, lead to the formation of a blood clot.
Atherosclerosis is a long-term, stealthy process, with a number of risk factors that can sneak up on anyone. High blood pressure, high cholesterol, diet, diabetes, stress, and your genes have all been implicated in this plaque-building process.
Other causes of heart attacks include spasms of the coronary arteries (causing them to constrict), chest trauma, or anything else that reduces blood flow to the heart muscle.
Regardless of the cause, blocking or reducing the flow of blood through these pipes can result in the heart muscle not receiving enough oxygen and nutrients. So cells in the heart muscle can be injured or die.

But a cardiac arrest is the result of heartbeat irregularities, making it harder for the heart to pump blood effectively around the body. These heartbeat irregularities are generally due to electrical malfunctions in the heart. There are four distinct types:
- ventricular tachycardia: a rapid and abnormal heart rhythm in which the heartbeat is more than 100 beats per minute (normal adult, resting heart rate is generally 60-90 beats per minute). This fast heart rate prevents the heart from filling with blood and thus pumping adequately
- ventricular fibrillation: instead of regular beats, the heart quivers or “fibrillates”, resembling a bag of worms, resulting in an irregular heartbeat greater than 300 beats per minute
- pulseless electrical activity: arises when the heart muscle fails to generate sufficient pumping force after electrical stimulation, resulting in no pulse
- asystole: the classic flat-line heart rhythm you see in movies, indicating no electrical activity in the heart.

Cardiac arrest can arise from numerous underlying conditions, both heart-related and not, such as drowning, trauma, asphyxia, electrical shock and drug overdose. James’ cardiac arrest was attributed to a congenital heart defect, a heart condition he was born with.
But among the many causes of a cardiac arrest, ischaemic heart disease, such as a heart attack, stands out as the most common cause, accounting for 70% of all cases.
So how can a heart attack cause a cardiac arrest? You’ll remember that during a heart attack, heart muscle can be damaged or parts of it may die. This damaged or dead tissue can disrupt the heart’s ability to conduct electrical signals, increasing the risk of developing arrhythmias, possibly causing a cardiac arrest.
So while a heart attack is a common cause of cardiac arrest, a cardiac arrest generally does not cause a heart attack.
What do they look like?
Because a cardiac arrest results in the sudden loss of effective heart pumping, the most common signs and symptoms are a sudden loss of consciousness, absence of pulse or heartbeat, stopping of breathing, and pale or blue-tinged skin.
But the common signs and symptoms of a heart attack include chest pain or discomfort, which can show up in other regions of the body such as the arms, back, neck, jaw, or stomach. Also frequent are shortness of breath, nausea, light-headedness, looking pale, and sweating.
What’s the take-home message?
While both heart attack and cardiac arrest are disorders related to the heart, they differ in their mechanisms and outcomes.
A heart attack is like a blockage in the plumbing supplying water to a house. But a cardiac arrest is like an electrical malfunction in the house’s wiring.
Despite their different nature both conditions can have severe consequences and require immediate medical attention.
Michael Todorovic, Associate Professor of Medicine, Bond University and Matthew Barton, Senior lecturer, School of Nursing and Midwifery, Griffith University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
High-Protein Paneer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
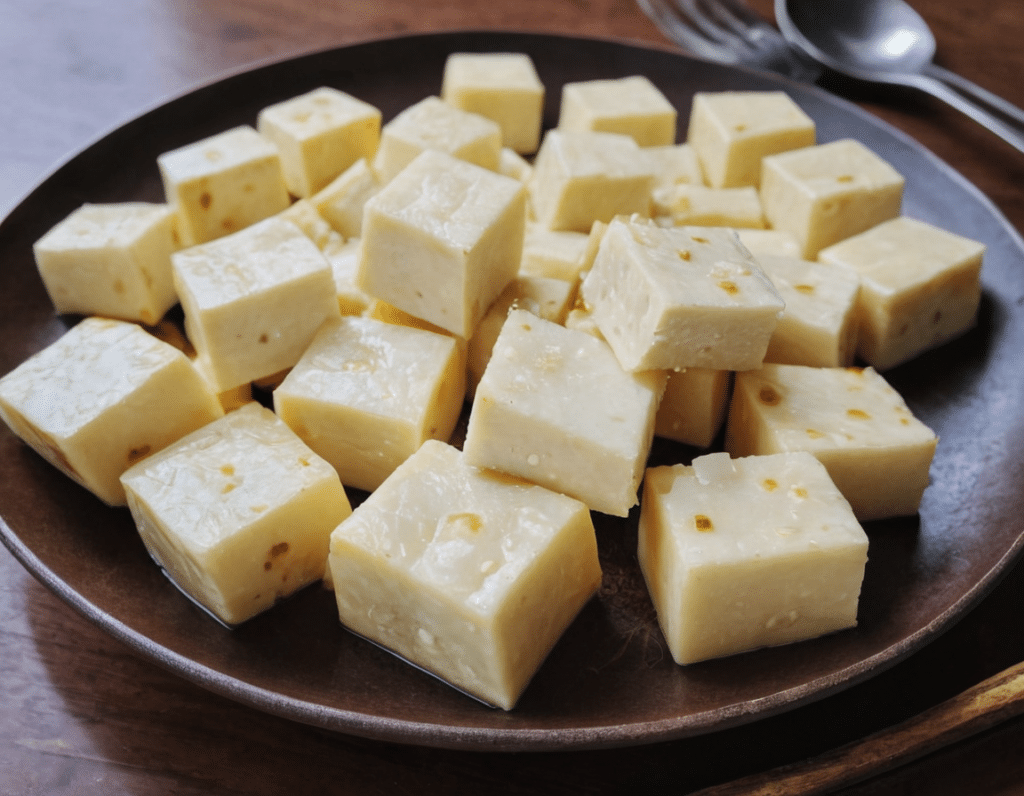
Paneer (a kind of Desi cheese used in many recipes from that region) is traditionally very high in fat, mostly saturated. Which is delicious, but not exactly the most healthy.
Today we’ll be making a plant-based paneer that does exactly the same jobs (has a similar texture and gentle flavor, takes on the flavors of dishes in the same way, etc) but with a fraction of the fat (of which only a trace amount is saturated, in this plant-based version), and even more protein. We’ll use this paneer in some recipes in the future, but it can be enjoyed by itself already, so let’s get going…
You will need
- ½ cup gram flour (unwhitened chickpea flour)
- Optional: 1 tsp low-sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Whisk the flour (and salt, if using) with 2 cups water in a big bowl, whisking until the texture is smooth.
2) Transfer to a large saucepan on a low-to-medium heat; you want it hot, but not quite a simmer. Keep whisking until the mixture becomes thick like polenta. This should take 10–15 minutes, so consider having someone else to take shifts if the idea of whisking continually for that long isn’t reasonable to you.
3) Transfer to a non-stick baking tin that will allow you to pour it about ½” deep. If the tin’s too large, you can always use a spatula to push it up against two or three sides, so that it’s the right depth
3) Refrigerate for at least 10 minutes, but longer is better if you have the time.
4) When ready to serve/use, cut it into ½” cubes. These can be served/used now, or kept for about a week in the fridge.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
Take care!
Share This Post
-
Daily, Weekly, Monthly: Habits Against Aging
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Anil Rajani has advice on restoring/retaining youthfulness. Two out of three of the sections are on skincare specifically, which may seem a vanity, but it’s also worth remembering that our skin is a very large and significant organ, and makes a big difference for the rest of our physical health, as well as our mental health. So, it’s worthwhile to look after it:
The recommendations
Daily: meditation practice
Meditation reduces stress, which reduction in turn protects telomere length, slowing the overall aging process in every living cell of the body.
Weekly: skincare basics
Dr. Rajani recommends a combination of retinol and glycolic acid. The former to accelerate cell turnover, stimulate collagen production, and reduce wrinkles; the latter, to exfoliate dead cells, allowing the retinol to do its job more effectively.
We at 10almonds would like to add: wearing sunscreen with SPF50 is a very good thing to do on any day that your phone’s weather app says the UV index is “moderate” or higher.
Monthly: skincare extras
Here are the real luxuries; spa visits, microneedling (stimulates collagen production), and non-ablative laser therapy. He recommends creating a home spa if possible for monthly skincare treatments, investing in high-quality devices for long-term benefits.
For more on all of these things, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Age & Aging: What Can (And Can’t) We Do About It?
- No-Frills, Evidence-Based Mindfulness
- The Evidence-Based Skincare That Beats Product-Specific Hype
Take care!
Share This Post
-
Natto, Taurine + Black Pepper, And Other Game-Changers
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Loved the info on nuts; of course I always eat pecans, which didn’t make the list of healthy nuts!❞
Dear subscriber, pardon the paraphrase of your comment—somehow it got deleted and now exists only in this writer’s memory. However, to address it:
Pecans are great too! We can’t include everything in every article (indeed, we got another feedback the same day saying the article was too long), but we love when you come to us with stuff for us to look at and write about (seriously, writer here: the more you ask, the easier it makes my job), so let’s talk pecans for a moment:
Pecans would have been number six on our list if we’d have written more!
Like many nuts, they’ve an abundance of healthy fats, fiber, vitamins, and minerals.
They’re particularly good for zinc, which is vital for immune function, healing (including normal recovery after normal exercise), and DNA synthesis (so: anti-aging).
Pecans are also great for reducing LDL (“bad” cholesterol) and triglycerides (which are also bad for heart health); check it out:
Share This Post
Related Posts
-
How Primary Care Is Being Disrupted: A Video Primer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How patients are seeing their doctor is changing, and that could shape access to and quality of care for decades to come.
More than 100 million Americans don’t have regular access to primary care, a number that has nearly doubled since 2014. Yet demand for primary care is up, spurred partly by record enrollment in Affordable Care Act plans. Under pressure from increased demand, consolidation, and changing patient expectations, the model of care no longer means visiting the same doctor for decades.
KFF Health News senior correspondent Julie Appleby breaks down what is happening — and what it means for patients.
More From This Investigation
Primary Care Disrupted
Known as the “front door” to the health system, primary care is changing. Under pressure from increased demand, consolidation, and changing patient expectations, the model of care no longer means visiting the same doctor for decades. KFF Health News looks at what this means for patients.
Credits
Hannah Norman Video producer and animator Oona Tempest Illustrator and creative director KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Forever Strong – by Dr. Gabrielle Lyon
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Obesity kills a lot of people (as does medical neglect and malpractice when it comes to obese patients, but that is another matter), but often the biggest problem is not “too much fat” but rather “too little muscle”. This gets disguised a bit, because these factors often appear in the same people, but it’s a distinction that’s worthy of note.
Dr. Lyon lays out a lot of good hard science in this work, generally in the field of protein metabolism, but also with a keen eye on all manner of blood metrics (triglycerides, LDL/HDL, fasting blood sugars, assorted other biomarkers of metabolic health).
The style of this book is two books in one. It’s a very accessible pop-science book in its primary tone, with an extra layer of precise science and lots of references, for those who wish to dive into that.
In the category of criticism, the diet plan section of the book is rather meat-centric, but the goal of this is protein content, not meat per se, so substitutions can easily be made. That’s just one small section of the book, though, and it’s little enough a downside that even Dr. Mark Hyman (a popular proponent of plant-based nutrition) highly recommends the book.
Bottom line: if you’d like to be less merely fighting decline and more actually becoming healthier as you age, then this book will help you do just that.
Click here to check out Forever Strong, and level up your wellness as you age!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Love Changes Your Brain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When we fall in love, have a romantic attachment, or have a sad breakup, there’s a lot going on neurochemically, and also with different parts of the brain taking the wheel. Dr. Shannon Odell explains:
The neurochemistry of love
Of course, not every love will follow this exact pattern, but here’s perhaps the most common one:
Infatuation stage: This early phase is characterized by obsessive thoughts and a strong desire to be with the person. The ventral tegmental area (VTA), the brain’s reward center, becomes highly active, releasing dopamine, one of the feel-good neurotransmitters, which makes love feel intoxicating, similar to addictive substances. Additionally, activity in the prefrontal cortex, responsible for critical thinking and judgment, decreases, causing people to see their partners through “rose-tinted glasses”. However, this intense stage usually lasts only a few months.
Attachment stage: As the relationship progresses, it shifts into a more stable and long-lasting phase. This stage is driven by oxytocin and vasopressin, hormones that promote trust/bonding and arousal, respectively. These same hormones also play a role in family and friendship connections. Oxytocin, in particular, reduces stress hormones, which is why spending time with a loved one can feel so calming.
Heartbreak stage: When a relationship ends, the insular cortex processes emotional and physical pain, making heartbreak feel as painful as a physical injury. Meanwhile, the VTA remains active, leading to intense longing and cravings for the lost partner, similar to withdrawal symptoms. The stress axis also activates, causing distress and restlessness. Over time, higher brain regions help regulate these emotions. Healing strategies such as exercise, socializing, and listening to music can help by triggering dopamine release and easing the pain of heartbreak.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: