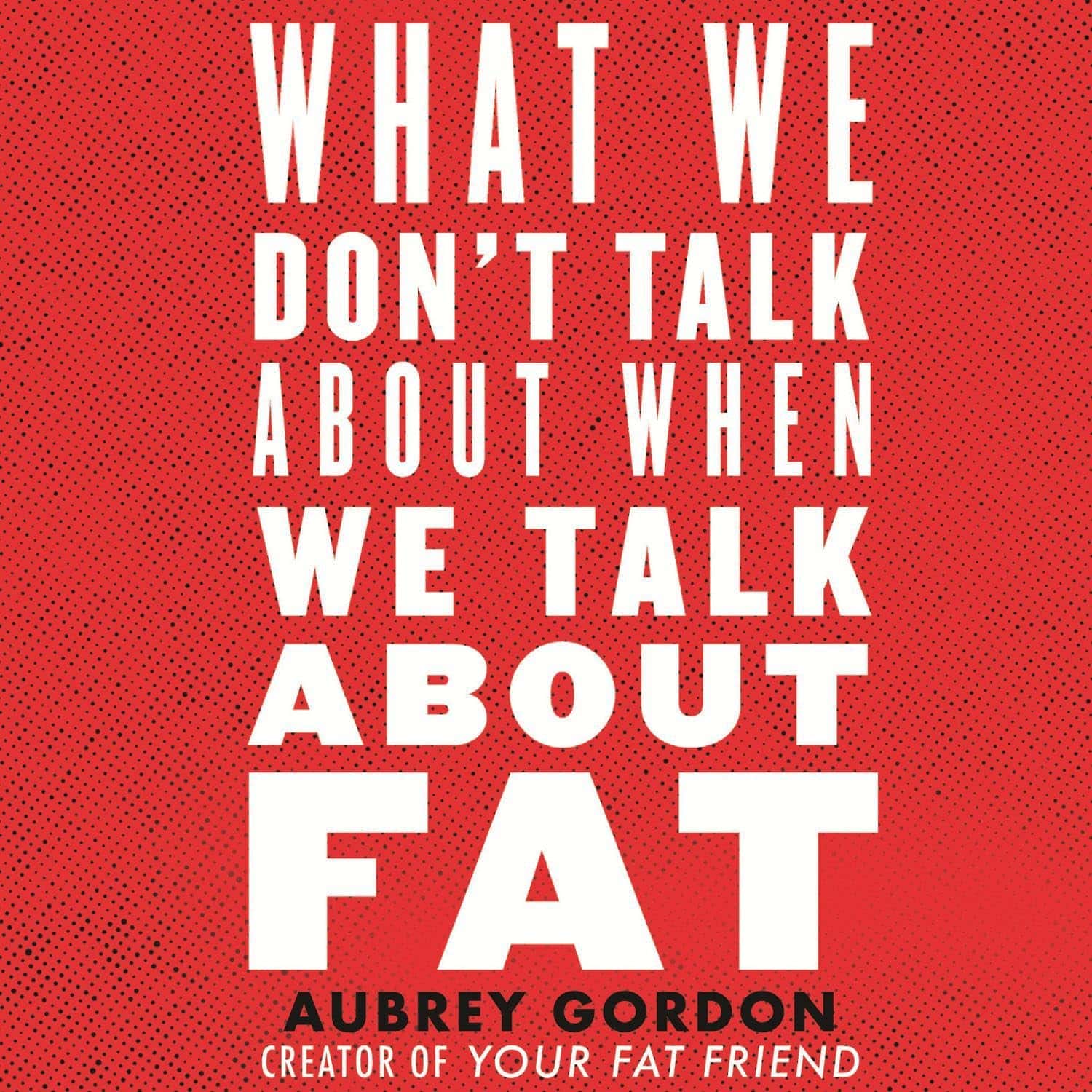
What We Don’t Talk About When We Talk About Fat – by Aubrey Gordon
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are books aplenty to encourage and help you to lose weight. This isn’t one of those.
There are also books aplenty to encourage and help you to accept yourself and your body at the weight you are, and forge self-esteem. This isn’t one of those, either—in fact, it starts by assuming you already have that.
There are fair arguments for body neutrality, and fat acceptance. Very worthy also is the constant fight for bodily sovereignty.
These are worthy causes, but they’re for the most-part not what our author concerns herself with here. Instead, she cares for a different and very practical goal: fat justice.
In a world where you may be turned away from medical treatment if you are over a certain size, told to lose half your bodyweight before you can have something you need, she demands better. The battle extends further than healthcare though, and indeed to all areas of life.
Ultimately, she argues, any society that will disregard the needs of the few because they’re a marginal demographic, is a society that will absolutely fail you if you ever differ from the norm in some way.
All in all, an important (and for many, perhaps eye-opening) book to read if you are fat, care about fat people, are a person of any size, or care about people in general.
Pick Up Your Copy of “What We Don’t Talk About When We Talk About Fat”, on Amazon Today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Glucomannan For Weight Loss, Gut Health, & More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Glucomannan is a water-soluble dietary fiber found in the root of the konjac plant.
If you’ve had konjac noodles, also called shirataki, that’s what those are mostly made of, and it’s why they have next-to-no calories.
You may be wondering: if it’s water-soluble, how do the noodles not dissolve in water? And the answer is that the noodle-making process involves making a gel out of the fiber and water, which is then extruded into noodle shapes. In this gelatinous form, they’re fairly stable (it’s one of the most viscous dietary fibers), but yes, if you were to boil them for a long time, they would indeed turn the entire liquid contents of the saucepan into gel.
How it works for weight loss
Because of its viscosity, adding even a small amount of powdered* glucomannan to a glass of water will turn the whole thing into gel in seconds. This means that if you take glucomannan capsules with a glass of water, then so far as your stomach is concerned, you just ate a cup of gel, and the water is now processed as food, staying longer in the stomach than it otherwise would, and promoting feelings of fullness.
*i.e. dry powder, not in a gelatinous form like the noodles
As for its efficacy in weight loss, see for example:
❝Glucomannan was well-tolerated and resulted in significant weight loss in overweight and obese individuals❞
Read more: Glucomannan and obesity: a critical review
So, that covers the basic requirements, but may be wondering: does it have other benefits? And the answer is yes, it does:
❝Glucomannan appears to beneficially affect total cholesterol, LDL cholesterol, triglycerides, body weight, and fasting blood glucose❞
To further corroborate that and comment on safety…
❝Results showed a significant mean weight loss using glucomannan over an eight-week period. Serum cholesterol and low-density lipoprotein cholesterol were significantly reduced in the glucomannan treated group. No adverse reactions to glucomannan were reported.❞
Read more: Effect of glucomannan on obese patients: a clinical study
As to whether other gel-making agents work the same way, the answer is no, they don’t seem to:
❝Glucomannan induced body weight reduction in healthy overweight subjects, whereas the addition of guar gum and alginate did not seem to cause additional loss of weight❞
Read more: Experiences with three different fiber supplements in weight reduction
How it works for gut health
In the words of Dr. Yu Li et al.,
❝Konjaku flour can achieve positive effects on treating obesity, which manifest on reducing BMI, fat mass, blood glucose, and blood lipid, improving hepatic function, and also regulating intestinal microfloral structure.
Therefore, changes in gut microbiota may explain in part the effects of konjaku flour.❞
Read in full: Effects of Konjaku Flour on the Gut Microbiota of Obese Patients
This has extra positive knock-on effects too:
Want to try some?
We don’t sell it, but here for your convenience are example products on Amazon:
Konjac noodles | Glucomannan capsules
Enjoy!
Share This Post
-
Oscar contender Poor Things is a film about disability. Why won’t more people say so?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Readers are advised this article includes an offensive and outdated disability term in a quote from the film.
Poor Things is a spectacular film that has garnered critical praise, scooped up awards and has 11 Oscar nominations. That might be the problem. Audiences become absorbed in another world, so much so our usual frames of reference disappear.
There has been much discussion about the film’s feminist potential (or betrayal). What’s not being talked about in mainstream reviews is disability. This seems strange when two of the film’s main characters are disabled.
Set in a fantasy version of Victorian London, unorthodox Dr Godwin Baxter (William Dafoe) finds the just-dead body of a heavily pregnant woman in the Thames River. In keeping with his menagerie of hybrid animals, Godwin removes the unborn baby’s brain and puts it into the skull of its mother, who becomes Bella Baxter (Emma Stone).
Is Bella really disabled?
Stone has been praised for her ability to embody a small child who rapidly matures into a hypersexual person – one who has not had time to absorb the restrictive rules of gender or patriarchy.
But we also see a woman using her behaviour to express herself because she has complex communication barriers. We see a woman who is highly sensitive and responsive to the sensory world around her. A woman moving through and seeing the world differently – just like the fish-eye lens used in many scenes.
Women like this exist and they have historically been confined, studied and monitored like Bella. When medical student Max McCandless (Ramy Youssef) first meets Bella, he offensively exclaims “what a very pretty retard!” before being told the truth and promptly declared her future husband.
Even if Bella is not coded as disabled through her movements, speech and behaviour, her onscreen creator and guardian is. Godwin Baxter has facial differences and other impairments which require assistive technology.
So ignoring disability as a theme of the film seems determined and overt. The absurd humour for which the film is being lauded is often at Bella’s “primitive”, “monstrous” or “damaged” actions: words which aren’t usually used to describe children, but have been used to describe disabled people throughout history.
In reviews, Bella’s walk and speech are compared to characters like the Scarecrow in The Wizard of Oz, rather than a disabled woman. So why the resistance?
Freak shows and displays
Disability studies scholar Rosemarie Gardland-Thomson writes “the history of disabled people in the Western world is in part the history of being on display”.
In the 19th century, when Poor Things is set, “freak shows” featuring disabled people, Indigenous people and others with bodily differences were extremely popular.
Doctors used freak shows to find specimens – like Joseph Merrick (also known as the Elephant Man and later depicted on screen) who was used for entertainment before he was exhibited in lecture halls. In the mid-1800s, as medicine became a profession, observing the disabled body shifted from a public spectacle to a private medical gaze that labelled disability as “sick” and pathologised it.
Poor Things doesn’t just circle around these discourses of disability. Bella’s body is a medical experiment, kept locked away for the private viewing of male doctors who take notes about her every move in small pads. While there is something glorious, intimate and familiar about Bella’s discovery of her own sexual pleasure, she immediately recognises it as worth recording in the third person:
I’ve discovered something that I must share […] Bella discover happy when she want!
The film’s narrative arc ends with Bella herself training to be a doctor but one whose more visible disabilities have disappeared.
Framing charity and sexual abuse
Even the film’s title is an expression often used to describe disabled people. The charity model of disability sees disabled people as needing pity and support from others. Financial poverty is briefly shown at a far-off port in the film and Bella initially becomes a sex worker in Paris for money – but her more pressing concern is sexual pleasure.
Disabled women’s sexuality is usually seen as something that needs to be controlled. It is frequently assumed disabled women are either hypersexual or de-gendered and sexually innocent.
In the real world disabled people experience much higher rates of abuse, including sexual assault, than others. Last year’s Royal Commission into Violence, Abuse, Neglect and Exploitation of People with Disability found women with disability are nearly twice as likely as women without disability to have been assaulted. Almost a third of women with disability have experienced sexual assault by the age of 15. Bella’s hypersexual curiosity appears to give her some layer of protection – but that portrayal denies the lived experience of many.
Watch but don’t ignore
Poor Things is a stunning film. But ignoring disability in the production ignores the ways in which the representation of disabled bodies play into deep and historical stereotypes about disabled people.
These representations continue to shape lives.
Louisa Smith, Senior lecturer, Deakin University; Gemma Digby, Lecturer – Health & Social Development, Deakin University, and Shane Clifton, Associate Professor of Practice, School of Health Sciences and the Centre for Disability Research and Policy, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
How Your Sleep Position Changes Dementia Risk
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is not just about sleep duration or even about sleep quality… It really is about which way your body is positioned.
Goodnight, glymphatic system
The association between sleeping position and dementia risk is about glymphatic drainage, which is largely powered by gravity (and thus dependent on which way around your head and neck are oriented), and very important for clearing toxins out of the brain—including beta-amyloid proteins.
This becomes particularly important when the glymphatic system becomes less efficient in midlife, often 15–20 years before cognitive decline symptoms appear.
The video’s thumbnail headline, “SCIENTISTS REVEAL: THE WAY YOUR SLEEP CAN CAUSE DEMENTIA” is overstated and inaccurate, but our adjusted headline “how your sleep position changes dementia risk” is actually representative of the paper on which this video was based; we’ll quote from the paper itself here:
❝This paper concludes that 1. glymphatic clearance plays a major role in Alzheimer’s pathology; 2. the vast majority of waste clearance occurs during sleep; 3. dementias are associated with sleep disruption, alongside an age-related decline in AQP4 polarization; and 4. lifestyle choices such as sleep position, alcohol intake, exercise, omega-3 consumption, intermittent fasting and chronic stress all modulate* glymphatic clearance. Lifestyle choices could therefore alter Alzheimer’s disease risk through improved glymphatic clearance, and could be used as a preventative lifestyle intervention for both healthy brain ageing and Alzheimer’s disease.❞
…and specifically, they found:
❝Glymphatic transport is most efficient in the right lateral sleeping position, with more CSF clearance occurring compared to supine and prone. The average person changes sleeping position 11 times per night, but there was no difference in the number of position changes between neurodegenerative and control groups, making the percentage of time spent in supine position the risk factor, not the number of position changes❞
Read the paper in full here: The Sleeping Brain: Harnessing the Power of the Glymphatic System through Lifestyle Choices
*saying “modulate” here is not as useful as it could be, because they modulate it differently: side-sleeping improves clearance; back sleeping decreases it; front-sleeping isn’t great either. Alcohol intake reduces clearance, exercise (especially cardiovascular exercise) improves it; omega-3 consumption improves it up a degree and does depend on omega-3/6 ratios, intermittent fasting improves it, and chronic stress worsens it.
And for a more pop-science presentation, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Clean Your Brain (Glymphatic Health Primer)
Take care!
Share This Post
Related Posts
-
Dealing With Waking Up In The Night
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I’m now in my sixties and find that I invariably wake up at least once during the night. Is this normal? Even if it is, I would still like, once in a while, to sleep right through like a teenager. How might this be achieved, without pills?❞
Most people wake up briefly between sleep cycles, and forget doing so. But waking up for more than a brief moment is indeed best avoided. In men of your age, if you’re waking to pee (especially if it’s then not actually that easy to pee), it can be a sign of an enlarged prostate. Which is again a) normal b) not optimal.
By “without pills” we’ll assume you mean “without sleeping pills”. There are options to treat an enlarged prostate, including well-established supplements. We did a main feature on this:
Prostate Health: What You Should Know
If the cause of waking up is something else, then again this is common for everyone as we get older, and again it’s not optimal. But since there are so many possible causes (and thus solutions), it’s more than we can cover in less than a main feature, so we’ll have to revisit this later.
Meanwhile, take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What is AuDHD? 5 important things to know when someone has both autism and ADHD
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may have seen some new ways to describe when someone is autistic and also has attention-deficit hyperactivity disorder (ADHD). The terms “AuDHD” or sometimes “AutiADHD” are being used on social media, with people describing what they experience or have seen as clinicians.
It might seem surprising these two conditions can co-occur, as some traits appear to be almost opposite. For example, autistic folks usually have fixed routines and prefer things to stay the same, whereas people with ADHD usually get bored with routines and like spontaneity and novelty.
But these two conditions frequently overlap and the combination of diagnoses can result in some unique needs. Here are five important things to know about AuDHD.
Kosro/Shutterstock 1. Having both wasn’t possible a decade ago
Only in the past decade have autism and ADHD been able to be diagnosed together. Until 2013, the Diagnostic and Statistical Manual of Mental Disorders (DSM) – the reference used by health workers around the world for definitions of psychological diagnoses – did not allow for ADHD to be diagnosed in an autistic person.
The manual’s fifth edition was the first to allow for both diagnoses in the same person. So, folks diagnosed and treated prior to 2013, as well as much of the research, usually did not consider AuDHD. Instead, children and adults may have been “assigned” to whichever condition seemed most prominent or to be having the greater impact on everyday life.
2. AuDHD is more common than you might think
Around 1% to 4% of the population are autistic.
They can find it difficult to navigate social situations and relationships, prefer consistent routines, find changes overwhelming and repetition soothing. They may have particular sensory sensitivities.
ADHD occurs in around 5–8% of children and adolescents and 2–6% of adults. Characteristics can include difficulties with focusing attention in a flexible way, resulting in procrastination, distraction and disorganisation. People with ADHD can have high levels of activity and impulsivity.
Studies suggest around 40% of those with ADHD also meet diagnostic criteria for autism and vice versa. The co-occurrence of having features or traits of one condition (but not meeting the full diagnostic criteria) when you have the other, is even more common and may be closer to around 80%. So a substantial proportion of those with autism or ADHD who don’t meet full criteria for the other condition, will likely have some traits.
3. Opposing traits can be distressing
Autistic people generally prefer order, while ADHDers often struggle to keep things organised. Autistic people usually prefer to do one thing at a time; people with ADHD are often multitasking and have many things on the go. When someone has both conditions, the conflicting traits can result in an internal struggle.
For example, it can be upsetting when you need your things organised in a particular way but ADHD traits result in difficulty consistently doing this. There can be periods of being organised (when autistic traits lead) followed by periods of disorganisation (when ADHD traits dominate) and feelings of distress at not being able to maintain organisation.
There can be eventual boredom with the same routines or activities, but upset and anxiety when attempting to transition to something new.
Autistic special interests (which are often all-consuming, longstanding and prioritised over social contact), may not last as long in AuDHD, or be more like those seen in ADHD (an intense deep dive into a new interest that can quickly burn out).
Autism can result in quickly being overstimulated by sensory input from the environment such as noises, lighting and smells. ADHD is linked with an understimulated brain, where intense pressure, novelty and excitement can be needed to function optimally.
For some people the conflicting traits may result in a balance where people can find a middle ground (for example, their house appears tidy but the cupboards are a little bit messy).
There isn’t much research yet into the lived experience of this “trait conflict” in AuDHD, but there are clinical observations.
4. Mental health and other difficulties are more frequent
Our research on mental health in children with autism, ADHD or AuDHD shows children with AuDHD have higher levels of mental health difficulites than autism or ADHD alone.
This is a consistent finding with studies showing higher mental health difficulties such as depression and anxiety in AuDHD. There are also more difficulties with day-to-day functioning in AuDHD than either condition alone.
So there is an additive effect in AuDHD of having the executive foundation difficulties found in both autism and ADHD. These difficulties relate to how we plan and organise, pay attention and control impulses. When we struggle with these it can greatly impact daily life.
5. Getting the right treatment is important
ADHD medication treatments are evidence-based and effective. Studies suggest medication treatment for ADHD in autistic people similarly helps improve ADHD symptoms. But ADHD medications won’t reduce autistic traits and other support may be needed.
Non-pharmacological treatments such as psychological or occupational therapy are less researched in AuDHD but likely to be helpful. Evidence-based treatments include psychoeducation and psychological therapy. This might include understanding one’s strengths, how traits can impact the person, and learning what support and adjustments are needed to help them function at their best. Parents and carers also need support.
The combination and order of support will likely depend on the person’s current functioning and particular needs. https://www.youtube.com/embed/pMx1DnSn-eg?wmode=transparent&start=0 ‘Up until recently … if you had one, you couldn’t have the other.’
Do you relate?
Studies suggest people may still not be identified with both conditions when they co-occur. A person in that situation might feel misunderstood or that they can’t fully relate to others with a singular autism and ADHD diagnosis and something else is going on for them.
It is important if you have autism or ADHD that the other is considered, so the right support can be provided.
If only one piece of the puzzle is known, the person will likely have unexplained difficulties despite treatment. If you have autism or ADHD and are unsure if you might have AuDHD consider discussing this with your health professional.
Tamara May, Psychologist and Research Associate in the Department of Paediatrics, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Older adults need another COVID-19 vaccine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What you need to know
- The CDC recommends people 65 and older and immunocompromised people receive an additional dose of the updated COVID-19 vaccine this spring—if at least four months have passed since they received a COVID-19 vaccine.
- Updated COVID-19 vaccines are effective at protecting against severe illness, hospitalization, death, and long COVID.
- The CDC also shortened the isolation period for people who are sick with COVID-19.
Last week, the CDC said people 65 and older should receive an additional dose of the updated COVID-19 vaccine this spring. The recommendation also applies to immunocompromised people, who were already eligible for an additional dose.
Older adults made up two-thirds of COVID-19-related hospitalizations between October 2023 and January 2024, so enhancing protection for this group is critical.
The CDC also shortened the isolation period for people who are sick with COVID-19, although the contagiousness of COVID-19 has not changed.
Read on to learn more about the CDC’s updated vaccination and isolation recommendations.
Who is eligible for another COVID-19 vaccine this spring?
The CDC recommends that people ages 65 and older and immunocompromised people receive an additional dose of the updated COVID-19 vaccine this spring—if at least four months have passed since they received a COVID-19 vaccine. It’s safe to receive an updated COVID-19 vaccine from Pfizer, Moderna, or Novavax, regardless of which COVID-19 vaccines you received in the past.
Updated COVID-19 vaccines are available at pharmacies, local clinics, or doctor’s offices. Visit Vaccines.gov to find an appointment near you.
Under- and uninsured adults can get the updated COVID-19 vaccine for free through the CDC’s Bridge Access Program. If you’re over 60 and unable to leave your home, call the Aging Network at 1-800-677-1116 to learn about free at-home vaccination options.
What are the benefits of staying up to date on COVID-19 vaccines?
Staying up to date on COVID-19 vaccines prevents severe illness, hospitalization, death, and long COVID.
Additionally, the CDC says staying up to date on COVID-19 vaccines is a safer and more reliable way to build protection against COVID-19 than getting sick from COVID-19.
What are the new COVID-19 isolation guidelines?
According to the CDC’s general respiratory virus guidance, people who are sick with COVID-19 or another common respiratory illness, like the flu or RSV, should isolate until they’ve been fever-free for at least 24 hours without the use of fever-reducing medication and their symptoms improve.
After that, the CDC recommends taking additional precautions for the next five days: wearing a well-fitting mask, limiting close contact with others, and improving ventilation in your home if you live with others.
If you’re sick with COVID-19, you can infect others for five to 12 days, or longer. Moderately or severely immunocompromised patients may remain infectious beyond 20 days.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: