What immunocompromised people want you to know
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
While many people in the U.S. have abandoned COVID-19 mitigations like vaccines and masking, the virus remains dangerous for everyone, and some groups face higher risks than others. Immunocompromised people—whose immune systems don’t work as well as they should due to health conditions or medications—are more vulnerable to infection and severe symptoms from the virus.
Public Good News spoke with three immunocompromised people about the steps they take to protect themselves and what they want others to know about caring for each other.
[Editor’s note: The contents of these interviews have been condensed for length.]
PGN: What measures have you been taking to protect yourself since the COVID-19 pandemic began?
Tatum Spears, Virginia
From less than a year old, I had serious, chronic infections and have missed huge chunks of my life. In 2020, I quit my public job, and I have not worked publicly since.
I have a degree in vocal performance and have been singing my whole life, but I haven’t performed publicly since 2019. I feel like a bird without wings. I had to stop traveling. Since no one wears a mask anymore, I can’t go to the movies or social outings or any party.
All my friends live in my phone now. It’s a community of people—a lot of them are immunocompromised or disabled in some way.
There are a good portion of them who just take COVID-19 seriously and want to protect their health, who feel the existential abandonment and the burden of all of this. It’s really isolating having to step back from any sort of social life. I have to assess my risk every single time I leave the house.
Gwendolyn Alyse Bishop, Washington
I was hit by a car when I was very young. I woke up from surgery, and doctors told me I had lost almost all of my spleen. So, I was always the sickest kid in my school.
When COVID-19 hit, I started working from home. At first, I wore cloth masks. I didn’t really learn about KN95 masks until right around the time that COVID-19 disabled me. [Editor’s note: N95 and KN95 masks have been shown to be significantly more effective at preventing the transmission of viral particles than cloth masks.]
I actually don’t get out much anymore because I am disabled by long COVID now, but when I do leave, I wear a respirator in all shared air spaces. My roommate and I have HEPA filters going in every room.
And then we test. I have a Pluslife testing dock, and so we keep a weekly testing schedule with that and then test if there are any symptoms. I got reinfected [with COVID-19] last winter, and a Pluslife test helped me catch it early and get Paxlovid. [Editor’s note: Pluslife is a brand of an at-home COVID-19 nucleic acid amplification test, which has been shown to be significantly more effective at detecting COVID-19 than at-home antigen rapid tests.]
Abby Mahler, California
I have lupus, and in 2016, I started taking the drug hydroxychloroquine, which is an immunomodulator. I’m not as immunocompromised as some people, but I certainly don’t have a normal immune system, which has resulted in long-term infections like C. diff.
I started masking early. My roommates and I prioritize going outside. We don’t remove our masks inside in public places.
We are in a pod with one other household, and the pod has agreements on the way that we interact with public space. So, we will only unmask with people who have tested ahead of time. We use Metrix, an at-home nucleic acid amplification test.
While it’s not easy and it’s not the life that we had prior to COVID-19’s existence, it is a life that has provided us quite a lot of freedom, in the sense that we are not sick all the time. We are conscientiously making decisions that allow us to have a nice time without a monkey on our backs, which is freeing.
PGN: What do you want people who are not immunocompromised to know?
T.S.: Don’t be afraid to be the only person in a room wearing a mask. Your own health is worth it. And you have to realize how callous [people who don’t wear a mask are] by existing in spaces and breathing [their] air [on immunocompromised people].
People think that vaccines are magic, but vaccines alone are not enough. I would encourage people to look at the Swiss cheese model of risk assessment.
Each slice of Swiss cheese has holes in it in different places, and each layer represents a layer of virus mitigation. One layer is vaccines. Another layer is masks. Then there’s staying home when you’re sick and testing.
G.A.B.: I wish people were masking. I wish people understood how likely it is that they are also now immunocompromised and vulnerable because of the widespread immune dysregulation that COVID-19 is causing. [Editor’s note: Research shows that COVID-19 infections may cause long-term harm to the immune system in some people.]
I want people to be invested in being good community members, and part of that is understanding that COVID-19 hits the poorest the hardest—gig workers, underpaid employees, frontline service workers, people who were already disabled or immunocompromised.
If people want to be good community members, they not only need to protect immunocompromised and disabled people by wearing a mask when they leave their homes, but they also need to actually start taking care of their community members and participating in mutual aid. [Editor’s note: Mutual aid is the exchange of resources and services within a community, such as people sharing extra N95 masks.]
I spend pretty much all of my time working on LongCOVIDAidBot, which promotes mutual aid for people who have been harmed by COVID-19.
A.M.: An important thing to think about when you’re not disabled is that it becomes a state of being for all people, if they’re lucky. You will become disabled, or you will die.
It is a privilege, in my opinion, to become disabled because I can learn different ways of living my life. And being able to see yourself as a body that changes over time, I hope, opens up a way of looking at your body as the porous reality that it is.
Some people think of themselves as being willing to make concessions or change their behavior when immunocompromised people are around, but you don’t always know when someone is immunocompromised.
So, if you’re not willing to change the way that you think about yourself as a person who is susceptible [to illness], then you should change the way that you consider other people around you. Wearing a mask—at the very least in public indoor spaces—means considering the unknown realities of all the people who are interacting with that space.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Better Than BMI
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
BMI is a very flawed system, and there are several more useful ways of measuring our bodies. Let’s take a look at them!
What’s wrong with BMI?
Oof, what isn’t wrong with BMI?
In short, it was developed as a demographic-based tool to specifically chart the weight-related health of working-age European white men a little under 200 years ago.
This means that if you are, perchance, not a working-age European white man in 1830 or so, then it’s not so useful. It’d be like first establishing height norms based on NBA basketball players, and then applying it to the general population, and thus coming to the conclusion that someone who is 6’2″ is very short.
In long, we did a deep-dive into it here, and in particular what things go dangerously wrong when it’s applied to women, non-white people, athletic people, pregnant people, people under 16 or over 65 and more:
When BMI Doesn’t Quite Measure Up
What we usually recommend instead
For heart disease risk and diabetes risk both, waist circumference is a much more universally reliable indicator. And since those two things tend to affect a lot of other health risks, it becomes an excellent starting point for being aware of many aspects of health.
Pregnancy will still throw off waist circumference a little (measure below the bump, not around it!), but it will nevertheless be more helpful than BMI even then, as it becomes necessary to just increase the numbers a little, according to gestational month and any confounding factors e.g. twins, triplets, etc. Ask your obstetrician about this, as it’s beyond the scope of our article today!
As to what’s considered a risk:
- Waist circumference of more than 35 inches for women
- Waist circumference of more than 40 inches for men
These numbers are considered applicable across demographics of age, ethnicity, and lifestyle.
Bonus extra measurement based on the above
Important also is waist to hip ratio.
How to calculate it:
- measure your waist circumference
- measure your hip circumference
- divide the first measurement by the second one
Because it’s a ratio, it doesn’t matter what units you use (e.g. inches, cm, etc) so long as you use the same units for both measurements.
The World Health Organization offers the following chart:
Health risk Women Men Low 0.80 or lower 0.95 or lower Moderate 0.81–0.85 0.96–1.0 High 0.86 or higher 1.1 or higher Source: Waist Circumference and Waist-Hip Ratio: Report of a WHO Expert Consultation
This is especially relevant for cardiovascular disease risk:
…and also holds true for all-cause mortality:
Waist-Hip-Ratio as a Predictor of All-Cause Mortality in High-Functioning Older Adults
An ancient contender that’s still more useful than BMI
Remember Archimedes? The (perhaps apocryphal) story of his “Eureka” moment in the bathtub when he realized that water displacement could be used to measure the volume of an irregular shape?
Just like Archimedes (who, the story goes, had been hired to determine the composition of a crown that might or might not have been pure gold), we can use this method to determine body composition, because we have references for how much a given volume of a given substance will weigh, so combing what we know about a body’s weight and volume will tell us about its composition in ways that neither metric could give us alone.
Indeed, it’s one of the commonly-mentioned flaws of BMI that muscle weighs more than fat, and Archimedes’ method not only avoids that problem, but also, actually turns that knowledge (muscle weighs more than fat) to our advantage.
It’s called “hydrostatic weighing” now:
You may be wondering: what about bones? Or internal organs?
The fact is that those are slightly confounding factors that do get in the way of a truly accurate analysis, but the variation in how much one person’s skeleton weighs vs another’s, or one person’s set of organs weigh than another’s, is too small to make an important difference to the health implications.
Lastly…
Hydrostatic weighing isn’t the only way to work out how much of our body is made of fat; if you have for example a smart scale at home (like this one) that tells you your body fat percentage, that is an estimate based on bioelectrical impedance analysis.
It’s less accurate than the hydrostatic method, but easier to do at home!
As to what percentages are “best”, healthy body fat percentages are (assuming normal hormones) generally considered to be in the range of 20–25% for women and 15–20% for men.
You can read more about this here:
Is A Visible Six-Pack Obtainable Regardless Of Genetic Predisposition?
Take care!
Share This Post
-
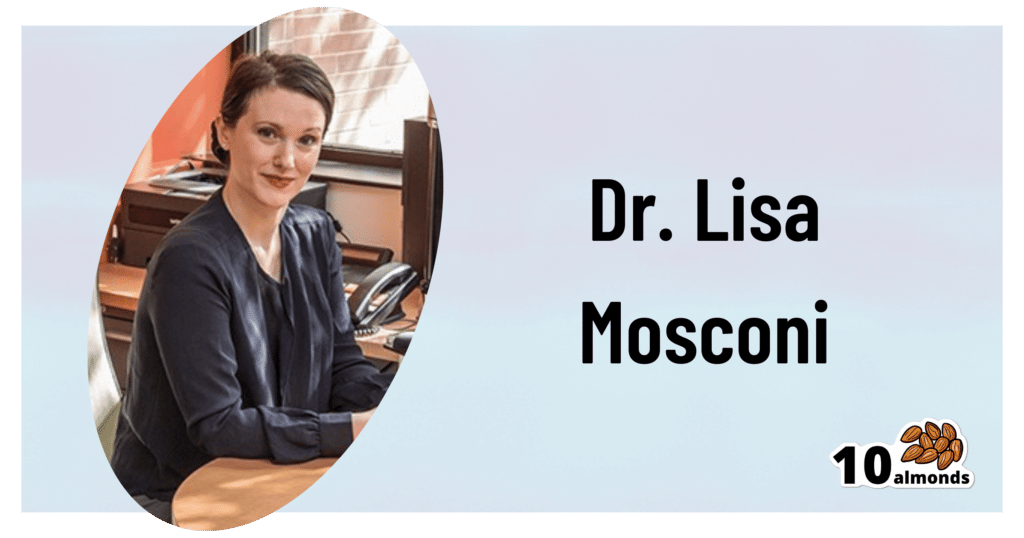
Your Brain On (And Off) Estrogen
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Dr. Lisa Mosconi. She’s a professor of Neuroscience in Neurology and Radiology, and is one of the 1% most influential scientists of the 21st century. That’s not a random number or an exaggeration; it has to do with citation metrics collated over 20 years:
A standardized citation metrics author database annotated for scientific field
What does she want us to know?
Women’s brains age differently from men’s
This is largely, of course, due to menopause, and as such is a generalization, but it’s a statistically safe generalization, because:
- Most women go through menopause—and most women who don’t, avoid it by dying pre-menopause, so the aging also does not occur in those cases
- Menopause is very rarely treated immediately—not least of all because menopause is diagnosed officially when it has been one year since one’s last period, so there’s almost always a year of “probably” first, and often numerous years, in the case of periods slowing down before stopping
- Menopausal HRT is great, but doesn’t completely negate that menopause occurred—because of the delay in starting HRT, some damage can be done already and can take years to reverse.
Medicated and unmedicated menopause proceed very differently from each other, and this fact has historically caused obfuscation of a lot of research into age-related neurodegeneration.
For example, it is well-established that women get Alzheimer’s at nearly twice the rate than men do, and deteriorate more rapidly after onset, too.
Superficially, one might conclude “estrogen is to blame” or maybe “the xx-chromosomal karyotype is to blame”.
The opposite, however, is true with regard to estrogen—estrogen appears to be a protective factor in women’s neurological health, which is why increased neurodegeneration occurs when estrogen levels decline (for example, in menopause).
For a full rundown on this, see:
Alzheimer’s Sex Differences May Not Be What They Appear
It’s not about the extra X
Dr. Mosconi examines this in detail in her book “The XX Brain”. To summarize and oversimplify a little: the XX karyotype by itself makes no difference, or more accurately, the XY karyotype by itself makes no difference (because biologically speaking, female physiological attributes are more “default” than male ones; it is only 12,000ish* years of culture that has flipped the social script on this).
*Why 12,000ish years? It’s because patriarchalism largely began with settled agriculture, for reasons that are fascinating but beyond the scope of this article, which is about health science, not archeology.
The topic of “which is biologically default” is relevant, because the XY karyotype (usually) informs the body “ignore previous instructions about ovaries, and adjust slightly to make them into testes instead”, which in turn (usually) results in a testosterone-driven system instead of an estrogen-driven system. And that is what makes the difference to the brain.
One way we can see that it’s about the hormones not the chromosomes, is in cases of androgen insensitivity syndrome, in which the natal “congratulations, it’s a girl” pronouncement may later be in conflict with the fact it turns out she had XY chromosomes all along, but the androgenic instructions never got delivered successfully, so she popped out with fairly typical female organs. And, relevantly for Dr. Mosconi, a typically female brain that will age in a typically female fashion, because it’s driven by estrogen, regardless of the Y-chromosome.
The good news
The good news from all of this is that while we can’t (with current science, anyway) do much about our chromosomes, we can do plenty about our hormones, and also, the results of changes in same.
Remember, Dr. Mosconi is not an endocrinologist, nor a gynecologist, but a neurologist. As such, she makes the case for how a true interdisciplinary team for treating menopause should not confined to the narrow fields usually associated with “bikini medicine”, but should take into account that a lot of menopause-related changes are neurological in nature.
We recently reviewed another book by Dr. Mosconi:
The Menopause Brain – by Dr. Lisa Mosconi
…and as we noted there, many sources will mention “brain fog” as a symptom of menopause, Dr. Mosconi can (and will) point to a shadowy patch on a brain scan and say “that’s the brain fog, there”.
And so on, for other symptoms that are often dismissed as “all in your head”, as though that’s a perfectly acceptable place for problems to be.
This is critical, because it’s treating real neurological things as the real things they are.
Dr. Mosconi’s advice, beyond HRT
Dr. Mosconi notes that brain health tends to dip during perimenopause but often recovers, showing the brain’s resilience to hormonal shifts. As such, all is not lost if for whatever reason, hormone replacement therapy isn’t a viable option for you.
Estrogen plays a crucial role in brain energy, and women’s declining estrogen levels during menopause increase the need for antioxidants to protect brain health—something not often talked about.
Specifically, Dr. Mosconi tells us, women need more antioxidants and have different metabolic responses to diets compared to men.*
*Yes, even though men usually have negligible estrogen, because their body (and thus brain, being also part of their body) is running on testosterone instead, which is something that will only happen if either you are producing normal male amounts of testosterone (requires normal male testes) or you are taking normal male amounts of testosterone (requires big bottles of testosterone; this isn’t the kind of thing you can get from a low dose of testogel as sometimes prescribed as part of menopausal HRT to perk your metabolism up).
Note: despite women being a slight majority on Earth, and despite an aging population in wealthy nations, meaning “a perimenopausal woman” is thus the statistically average person in, for example, the US, and despite the biological primacy of femaleness… Medicine still mostly looks to men as the “default person”, which in this case can result in seriously low-balled estimates of what antioxidants are needed.
In terms of supplements, therefore, she recommends:
- Antioxidants: key for brain health, especially in women. Rich sources include fruits (especially berries) and vegetables. Then there’s the world’s most-consumed antioxidant, which is…
- Coffee: Italian-style espresso has the highest antioxidant power. Adding a bit of fat (e.g. oat milk) helps release caffeine more slowly, reducing jitters. Taking it alongside l-theanine also “flattens the curve” and thus improves its overall benefits.
- Flavonoids: important for both men and women but particularly essential for women. Found in many fruits and vegetables.
- Chocolate: dark chocolate is an excellent source of antioxidants and flavonoids!
- Turmeric: a natural neuroprotectant with anti-inflammatory properties, best boosted by taking with black pepper, which improves absorption as well as having many great qualities of its own.
- B Vitamins: B6, B9, and B12 are essential for anti-aging and brain health; deficiency in B6 is rare, while deficiency in B9 (folate) and especially B12 is very common later in life.
- Vitamins C & E: important antioxidants, but caution is needed with fat-soluble vitamins to avoid toxicity.
- Omega-3s: important for brain health; can be consumed in the diet, but supplements may be necessary.
- Caution with zinc: zinc can support immunity and endocrine health (and thus, indirectly, brain health) but may be harmful in excess, particularly for brain health.
- Probiotics & Prebiotics: beneficial for gut health, and in Dr. Mosconi’s opinion, hard to get sufficient amounts from diet alone.
For more pointers, you might want to check out the MIND diet, that is to say, the “Mediterranean-DASH Intervention for Neurodegenerative Delay” upgrade to make the Mediterranean diet even brain-healthier than it is by default:
Four Ways To Upgrade The Mediterranean Diet
Want to know more from Dr. Mosconi?
Here’s her TED talk:
Click Here If The Embedded Video Doesn’t Load Automatically!
Enjoy!
Share This Post
-
Syringe Exchange Fears Hobble Fight Against West Virginia HIV Outbreak
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
CHARLESTON, http://w.va/. — More than three years have passed since federal health officials arrived in central Appalachia to assess an alarming outbreak of HIV spread mostly between people who inject opioids or methamphetamine.
Infectious disease experts from the Centers for Disease Control and Prevention made a list of recommendations following their visit, including one to launch syringe service programs to stop the spread at its source. But those who’ve spent years striving to protect people who use drugs from overdose and illness say the situation likely hasn’t improved, in part because of politicians who contend that such programs encourage illegal drug use.
Joe Solomon is a Charleston City Council member and co-director of SOAR WV, a group that works to address the health needs of people who use drugs. He’s proud of how his close-knit community has risen to this challenge but frustrated with the restraints on its efforts.
“You see a city and a county willing to get to work at a scale that’s bigger than ever before,” Solomon said, “but we still have one hand tied behind our back.”
The hand he references is easier access to clean syringes.
In April 2021, the CDC came to Charleston — the seat of Kanawha County and the state capital, tucked into the confluence of the Kanawha and Elk rivers — to investigate dozens of newly detected HIV infections. The CDC’s HIV intervention chief called it “the most concerning HIV outbreak in the United States” and warned that the number of reported diagnoses could be just “the tip of the iceberg.”
Now, despite attention and resources directed toward the outbreak, researchers and health workers say HIV continues to spread. In large part, they say, the outbreak lingers because of restrictions state and local policymakers have placed on syringe exchange efforts.
Research indicates that syringe service programs are associated with an estimated 50% reduction in HIV and hepatitis C, and the CDC issued recommendations to steer a response to the outbreak that emphasized the need for improved access to those services.
That advice has thus far gone unheeded by local officials.
In late 2015, the Kanawha-Charleston Health Department launched a syringe service program but shuttered it in 2018 under pressure, with then-Mayor Danny Jones calling it a “mini-mall for junkies and drug dealers.”
SOAR stepped in, hosting health fairs at which it distributed naloxone, an opioid overdose reversal drug; offered treatment and referrals; provided HIV testing; and exchanged clean syringes for used ones.
But in April 2021, the state legislature passed a bill limiting the number of syringes people could exchange and made it mandatory to present a West Virginia ID. The Charleston City Council subsequently added guidelines of its own, including requiring individual labeling of syringes.
As a result of these restrictions, SOAR ceased exchanging syringes. West Virginia Health Right now operates an exchange program in the city under the restrictions.
Robin Pollini is a West Virginia University epidemiologist who conducts community-based research on injection drug use. “Anyone I’ve talked to who’s used that program only used it once,” she said. “And the numbers they report to the state bear that out.”
A syringe exchange run by the health department in nearby Cabell County — home to Huntington, the state’s largest city after Charleston — isn’t so constrained. As Solomon notes, that program exchanges more than 200 syringes for every one exchanged in Kanawha.
A common complaint about syringe programs is that they result in discarded syringes in public spaces. Jan Rader, director of Huntington’s Mayor’s Office of Public Health and Drug Control Policy, is regularly out on the streets and said she seldom encounters discarded syringes, pointing out that it’s necessary to exchange a used syringe for a new one.
In August 2023, the Charleston City Council voted down a proposal from the Women’s Health Center of West Virginia to operate a syringe exchange in the city’s West Side community, with opponents expressing fears of an increase in drug use and crime.
Pollini said it’s difficult to estimate the number of people in West Virginia with HIV because there’s no coordinated strategy for testing; all efforts are localized.
“You would think that in a state that had the worst HIV outbreak in the country,” she said, “by this time we would have a statewide testing strategy.”
In addition to the testing SOAR conducted in 2021 at its health fairs, there was extensive testing during the CDC’s investigation. Since then, the reported number of HIV cases in Kanawha County has dropped, Pollini said, but it’s difficult to know if that’s the result of getting the problem under control or the result of limited testing in high-risk groups.
“My inclination is the latter,” she said, “because never in history has there been an outbreak of injection-related HIV among people who use drugs that was solved without expanding syringe services programs.”
“If you go out and look for infections,” Pollini said, “you will find them.”
Solomon and Pollini praised the ongoing outreach efforts — through riverside encampments, in abandoned houses, down county roads — of the Ryan White HIV/AIDS Program to test those at highest risk: people known to be injecting drugs.
“It’s miracle-level work,” Solomon said.
But Christine Teague, Ryan White Program director at the Charleston Area Medical Center, acknowledged it hasn’t been enough. In addition to HIV, her concerns include the high incidence of hepatitis C and endocarditis, a life-threatening inflammation of the lining of the heart’s chambers and valves, and the cost of hospital resources needed to address them.
“We’ve presented that data to the legislature,” she said, “that it’s not just HIV, it’s all these other lengthy hospital admissions that, essentially, Medicaid is paying for. And nothing seems to penetrate.”
Frank Annie is a researcher at CAMC specializing in cardiovascular diseases, a member of the Charleston City Council, and a proponent of syringe service programs. Research he co-authored found 462 cases of endocarditis in southern West Virginia associated with injection drug use, at a cost to federal, state, and private insurers of more than $17 million, of which less than $4 million was recovered.
Teague is further concerned for West Virginia’s rural counties, most of which don’t have a syringe service program.
Tasha Withrow, a harm reduction advocate in bordering rural Putnam County, said her sense is that HIV numbers aren’t alarmingly high there but said that, with little testing and heightened stigma in a rural community, it’s difficult to know.
In a January 2022 follow-up report, the CDC recommended increasing access to harm reduction services such as syringe service programs through expansion of mobile services, street outreach, and telehealth, using “patient-trusted” individuals, to improve the delivery of essential services to people who use drugs.
Teague would like every rural county to have a mobile unit, like the one operated by her organization, offering harm reduction supplies, medication, behavioral health care, counseling, referrals, and more. That’s an expensive undertaking. She suggested opioid settlement money through the West Virginia First Foundation could pay for it.
Pollini said she hopes state and local officials allow the experts to do their jobs.
“I would like to see them allow us to follow the science and operate these programs the way they’re supposed to be run, and in a broader geography,” she said. “Which means that it shouldn’t be a political decision; it should be a public health decision.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
Goat Milk Greek Yogurt vs Almond Milk Greek Yogurt – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing goat milk yogurt to almond milk yogurt, we picked the almond milk yogurt.
Why?
Surprised? Honestly, we were too!
Much as we love almonds, we were fully expecting to write about how they’re very close in nutritional value, but the dairy yogurt has more probiotics, but no, as it turns out when we looked into them, they’re quite comparable in that regard.
It’s easy to assume “goat milk yogurt is more natural and therefore healthier”, but in both cases, it was a case of taking a fermentable milk, and fermenting it (an ancient process). “But almond milk is a newfangled thing”, well, new-ish…
So what was the deciding factor?
In this case, the almond milk yogurt has about twice the protein per (same size) serving, compared to the goat milk; all the other macros are about the same, and the micronutrients are similar. Like many plant-based milks and yogurts, this one is fortified with calcium and vitamin D, so that wasn’t an issue either.
In short: the only meaningful difference was the protein, and the almond came out on top.
However!
The almond came out on top only because it is strained; this can be done (or not) with any kind of yogurt, be it from an animal or a plant.
In other words: if it had been different brands, the goat milk yogurt could have come out on top!
The take-away idea here is: always read labels, because as you’ve just seen, even we can get surprised sometimes!
seriously if you only remember one thing from this today, make it the above
Other thing worth mentioning: yogurts, and dairy products in general, are often made with common allergens (e.g. dairy, nuts, soy, etc). So if you are allergic or intolerant, obviously don’t choose the one to which you are allergic or intolerant.
That said… If you are lactose-intolerant, but not allergic, goat’s milk does have less lactose than cow’s milk. But of course, you know your limits better than we can in this regard.
Want to try some?
Amazon is not coming up with the goods for this one (or anything even similar, at time of writing), so we recommend trying your local supermarket (and reading labels, because products vary widely!)
What you’re looking for (be it animal- or plant-based):
- Live culture probiotic bacteria
- No added sugar
- Minimal additives in general
- Lastly, check out the amounts for protein, calcium, vitamin D, etc.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Much Alcohol Does It Take To Increase Cancer Risk?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Alcohol is, of course, unhealthy. Not even the famous “small glass of red” is recommended:
Alcohol also increases all-cause mortality at any dose (even “low-risk drinking”):
Alcohol Consumption Patterns and Mortality Among Older Adults
…and the World Health Organization has declared that the only safe amount of alcohol is zero:
WHO: No level of alcohol consumption is safe for our health
But what of alcohol and cancer? According to the American Association of Cancer Research’s latest report, more than half of Americans do not know that alcohol increases the risk of cancer:
Source: AACR Cancer Progress Report
Why/how does alcohol increase the risk of cancer?
There’s an obvious aspect and a less obvious but very important aspect:
- The obvious: alcohol damages almost every system in the body, and so it’s little surprise if that includes systems whose job it is to keep us safe from cancer.
- The less obvious: alcohol is largely metabolized by certain enzymes that have an impact on DNA repair, such as alcohol dehydrogenases and aldehyde dehydrogenases, amongst others, and noteworthily, acetaldehyde (the main metabolite of alcohol) is itself genotoxic.
Read more: Alcohol & Cancer
This is important, because it means alcohol also increases the risk of cancers other than the obvious head/neck, laryngeal, esophageal, liver, and colorectal cancers.
However, those cancers are of course the most well-represented of alcohol-related cancers, along with breast cancer (this has to do with alcohol’s effect on estrogen metabolism).
If you’re curious about the numbers, and the changes in risk if one reduces/quits/reprises drinking:
❝The increased alcohol-related cancer incidence was associated with dose; those who changed from nondrinking to mild (adjusted hazard ratio [aHR], 1.03; 95% CI, 1.00-1.06), moderate (aHR, 1.10; 95% CI, 1.02-1.18), or heavy (aHR, 1.34; 95% CI, 1.23-1.45) drinking levels had an associated higher risk than those who did not drink.
Those with mild drinking levels who quit drinking had a lower risk of alcohol-related cancer (aHR, 0.96; 95% CI, 0.92-0.99) than those who sustained their drinking levels.
Those with moderate (aHR, 1.07; 95% CI, 1.03-1.12) or heavy (aHR, 1.07; 95% CI, 1.02-1.12) drinking levels who quit drinking had a higher all cancer incidence than those who sustained their levels, but when quitting was sustained, this increase in risk disappeared.
Results of this study showed that increased alcohol consumption was associated with higher risks for alcohol-related and all cancers, whereas sustained quitting and reduced drinking were associated with lower risks of alcohol-related and all cancers.
Alcohol cessation and reduction should be reinforced for the prevention of cancer.❞
Source: Association Between Changes in Alcohol Consumption and Cancer Risk
Worried it’s too late?
If you’re reading this (and thus, evidently, still alive), it isn’t. It’s never too late (nor too early) to reduce, or ideally stop, drinking. Even if you already have cancer, drinking more alcohol will only exacerbate things, and abstaining from alcohol will improve your chances of recovery.
For a reassuring timeline of recovery from alcohol-related damage, see:
What Happens To Your Body When You Stop Drinking Alcohol
Want to stop, but have tried before and find it daunting?
There are a few ways to make it a lot easier:
Rethinking Drinking: How To Reduce Or Quit Alcohol
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Yes, adults can develop food allergies. Here are 4 types you need to know about
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you didn’t have food allergies as a child, is it possible to develop them as an adult? The short answer is yes. But the reasons why are much more complicated.
Preschoolers are about four times more likely to have a food allergy than adults and are more likely to grow out of it as they get older.
It’s hard to get accurate figures on adult food allergy prevalence. The Australian National Allergy Council reports one in 50 adults have food allergies. But a US survey suggested as many as one in ten adults were allergic to at least one food, with some developing allergies in adulthood.
What is a food allergy
Food allergies are immune reactions involving immunoglobulin E (IgE) – an antibody that’s central to triggering allergic responses. These are known as “IgE-mediated food allergies”.
Food allergy symptoms that are not mediated by IgE are usually delayed reactions and called food intolerances or hypersensitivity.
Food allergy symptoms can include hives, swelling, difficulty swallowing, vomiting, throat or chest tightening, trouble breathing, chest pain, rapid heart rate, dizziness, low blood pressure or anaphylaxis.
Symptoms include hives. wisely/Shutterstock IgE-mediated food allergies can be life threatening, so all adults need an action management plan developed in consultation with their medical team.
Here are four IgE-mediated food allergies that can occur in adults – from relatively common ones to rare allergies you’ve probably never heard of.
1. Single food allergies
The most common IgE-mediated food allergies in adults in a US survey were to:
- shellfish (2.9%)
- cow’s milk (1.9%)
- peanut (1.8%)
- tree nuts (1.2%)
- fin fish (0.9%) like barramundi, snapper, salmon, cod and perch.
In these adults, about 45% reported reacting to multiple foods.
This compares to most common childhood food allergies: cow’s milk, egg, peanut and soy.
Overall, adult food allergy prevalence appears to be increasing. Compared to older surveys published in 2003 and 2004, peanut allergy prevalence has increased about three-fold (from 0.6%), while tree nuts and fin fish roughly doubled (from 0.5% each), with shellfish similar (2.5%).
While new adult-onset food allergies are increasing, childhood-onset food allergies are also more likely to be retained into adulthood. Possible reasons for both include low vitamin D status, lack of immune system challenges due to being overly “clean”, heightened sensitisation due to allergen avoidance, and more frequent antibiotic use.
Some adults develop allergies to cow’s milk, while others retain their allergy from childhood. Sarah Swinton/Unsplash 2. Tick-meat allergy
Tick-meat allergy, also called α-Gal syndrome or mammalian meat allergy, is an allergic reaction to galactose-alpha-1,3-galactose, or α-Gal for short.
Australian immunologists first reported links between α-Gal syndrome and tick bites in 2009, with cases also reported in the United States, Japan, Europe and South Africa. The US Centers for Disease Control estimates about 450,000 Americans could be affected.
The α-Gal contains a carbohydrate molecule that is bound to a protein molecule in mammals.
The IgE-mediated allergy is triggered after repeated bites from ticks or chigger mites that have bitten those mammals. When tick saliva crosses into your body through the bite, antibodies to α-Gal are produced.
When you subsequently eat foods that contain α-Gal, the allergy is triggered. These triggering foods include meat (lamb, beef, pork, rabbit, kangaroo), dairy products (yoghurt, cheese, ice-cream, cream), animal-origin gelatin added to gummy foods (jelly, lollies, marshmallow), prescription medications and over-the counter supplements containing gelatin (some antibiotics, vitamins and other supplements).
Tick-meat allergy reactions can be hard to recognise because they’re usually delayed, and they can be severe and include anaphylaxis. Allergy organisations produce management guidelines, so always discuss management with your doctor.
3. Fruit-pollen allergy
Fruit-pollen allergy, called pollen food allergy syndrome, is an IgE-mediated allergic reaction.
In susceptible adults, pollen in the air provokes the production of IgE antibodies to antigens in the pollen, but these antigens are similar to ones found in some fruits, vegetables and herbs. The problem is that eating those plants triggers an allergic reaction.
The most allergenic tree pollens are from birch, cypress, Japanese cedar, latex, grass, and ragweed. Their pollen can cross-react with fruit and vegetables, including kiwi, banana, mango, avocado, grapes, celery, carrot and potato, and some herbs such as caraway, coriander, fennel, pepper and paprika.
Fruit-pollen allergy is not common. Prevalence estimates are between 0.03% and 8% depending on the country, but it can be life-threatening. Reactions range from itching or tingling of lips, mouth, tongue and throat, called oral allergy syndrome, to mild hives, to anaphylaxis.
4. Food-dependent, exercise-induced food allergy
During heavy exercise, the stomach produces less acid than usual and gut permeability increases, meaning that small molecules in your gut are more likely to escape across the membrane into your blood. These include food molecules that trigger an IgE reaction.
If the person already has IgE antibodies to the foods eaten before exercise, then the risk of triggering food allergy reactions is increased. This allergy is called food-dependent exercise-induced allergy, with symptoms ranging from hives and swelling, to difficulty breathing and anaphylaxis.
This type of allergy is extremely rare. Ben O’Sullivan/Unsplash Common trigger foods include wheat, seafood, meat, poultry, egg, milk, nuts, grapes, celery and other foods, which could have been eaten many hours before exercising.
To complicate things even further, allergic reactions can occur at lower levels of trigger-food exposure, and be more severe if the person is simultaneously taking non-steroidal inflammatory medications like aspirin, drinking alcohol or is sleep-deprived.
Food-dependent exercise-induced allergy is extremely rare. Surveys have estimated prevalence as between one to 17 cases per 1,000 people worldwide with the highest prevalence between the teenage years to age 35. Those affected often have other allergic conditions such as hay fever, asthma, allergic conjunctivitis and dermatitis.
Allergies are a growing burden
The burden on physical health, psychological health and health costs due to food allergy is increasing. In the US, this financial burden was estimated as $24 billion per year.
Adult food allergy needs to be taken seriously and those with severe symptoms should wear a medical information bracelet or chain and carry an adrenaline auto-injector pen. Concerningly, surveys suggest only about one in four adults with food allergy have an adrenaline pen.
If you have an IgE-mediated food allergy, discuss your management plan with your doctor. You can also find more information at Allergy and Anaphylaxis Australia.
Clare Collins, Laureate Professor in Nutrition and Dietetics, University of Newcastle
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: