What Happens To Your Body When You Stop Drinking Alcohol
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Immediately after we stop drinking is rarely when we feel our best. But how long is it before we can expect to see benefits, instead of just suffering?
Timeline
After stopping drinking alcohol for…
- Seconds: the liver starts making progress filtering out toxins and sugars; ethanol starts to leave the system
- 1 hour: fatigue sets in as the body uses a lot of energy to metabolize and eliminate alcohol. However, sleep quality (if one goes to sleep now) is low because alcohol disrupts the brain patterns required for restful sleep
- 6–12 hours: the immune system starts recovering from the suppression caused by alcohol
- 24 hours: immune system is back to normal; withdrawal symptoms may occur in the case of heavy drinkers
- 3–5 days: resting blood pressure begins to drop, as stress levels decrease (alcohol may seem anxiolytic, but it is actually anxiogenic; it just masks its own effect in this regard). Also, because of insulin responses improving, appetite reduces. The liver, once it has finished dealing your last drinking session (if you used to drink all the time, it probably had a backlog to clear), can now begin to make repairs on itself.
- 1 week: skin will start looking better, as antidiuretic hormone levels neutralize, leading to a healthier maintenance of hydration
- 2 weeks: cognitive abilities improve as the brain begins to make progress in repairing itself. At the same time, kidneys start to heal.
- 3–4 weeks: the liver begins to regenerate in earnest. You may wonder what took it so long given the liver’s famous regenerative abilities, but in this case, the liver was also the organ that took the most damage from drinking, so its regeneration gets off to a slow start (in contrast, if the liver had “merely” suffered physical trauma, such as being shot, stabbed,
or eaten by eagles,it’d start regenerating vigorously as soon as the immediate wound-response had been tended to). Once it is able to pick up the pace though, overall health improves, as the liver can focus on breaking down other toxins. - 1–2 months: the heart is able to repair itself, and start to become stronger again (dependent on other lifestyle factors, of course).
- 3 months and more: bodily repairs continue (for example, the damage to the liver is often so severe that it can take quite a bit longer to recover completely, and repairs in the brain are always slow, for reasons beyond the scope of this article). Looking at the big picture, at this point we also see other benefits, such as reduced cancer risks.
In short… It’s never too soon to stop, but it’s also never too late, unless you are going to die in the next few days. So long as you’ll be in the land of the living for a few days yet, there’s time to enjoy the benefits of stopping.
Most importantly: the timeline for the most important repairs is not as long as many people might think, and that itself can be very motivating.
For more detail on much of the above, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Can We Drink To Good Health?
- How To Reduce Or Quit Alcohol
- Addiction Myths That Are Hard To Quit
- How To Unfatty A Fatty Liver
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Problem With Sweeteners
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The WHO’s view on sugar-free sweeteners
The WHO has released a report offering guidance regards the use of sugar-free sweeteners as part of a weight-loss effort.
In a nutshell, the guidance is: don’t
- Here’s the report itself: Use of non-sugar sweeteners: WHO guideline
- Here’s the WHO’s own press release about it: WHO advises not to use non-sugar sweeteners for weight control in newly released guideline
- And it was based on this huge systematic review: Health effects of the use of non-sugar sweeteners: a systematic review and meta-analysis
They make for interesting reading, so if you don’t have time now, you might want to just quickly open and bookmark them for later!
Some salient bits and pieces:
Besides that some sweeteners can cause gastro-intestinal problems, a big problem is desensitization:
Because many sugar substitutes are many times (in some cases, hundreds of times) sweeter than sugar, this leads to other sweet foods tasting more bland, causing people to crave sweeter and sweeter foods for the same satisfaction level.
You can imagine how that’s not a spiral that’s good for the health!
The WHO recommendation applies to artificial and naturally-occurring non-sugar sweeteners, including:
- Acesulfame K
- Advantame
- Aspartame
- Cyclamates
- Neotame
- Saccharin
- Stevia
Sucralose and erythritol, by the way, technically are sugars, just not “that kind of sugar” so they didn’t make the list of non-sugar sweeteners.
That said, a recent study did find that erythritol was linked to a higher risk of heart attack, stroke, and early death, so it may not be an amazing sweetener either:
Read: The artificial sweetener erythritol and cardiovascular event risk
Want to know a good way of staying healthy in the context of sweeteners?
Just get used to using less. Your taste buds will adapt, and you’ll get just as much pleasure as before, from progressively less sweetening agent.
Share This Post
-
All of your hepatitis B vaccine questions answered
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Hepatitis B is a viral infection that can cause liver disease in people of any age or background. Vaccination is 95 percent effective against the virus. But in recent years, false claims, rumors, and myths about the hepatitis B vaccine have become increasingly common.
Here’s everything you need to know about the lifesaving hepatitis B vaccine.
What is hepatitis B?
Hepatitis B is a liver infection caused by the hepatitis B virus. The virus attacks the liver, causing severe short-term and long-term infections.
Short-term hepatitis B infections may cause “fever, fatigue, loss of appetite, nausea, vomiting, jaundice (yellow skin or eyes, dark urine, clay-colored bowel movements), and pain in the muscles, joints, and stomach,” according to the Centers for Disease Control and Prevention.
A long-term hepatitis B infection occurs when the virus stays in the body beyond the initial infection, causing chronic illness. Hepatitis B infections become chronic in 90 percent of infected infants, half of infected young children, and between 5 to 10 percent of infected adults.
“Most people who go on to develop chronic hepatitis B do not have symptoms, but it is still very serious and can lead to liver damage (cirrhosis), liver cancer, and death. Chronically infected people can spread hepatitis B virus to others, even if they do not feel or look sick themselves,” says the CDC.
How does the hepatitis B virus spread?
The hepatitis B virus is spread through body fluids, including blood, semen, and saliva. It can also be transmitted from birthing parent to child during pregnancy and childbirth.
“While hepatitis B is an infection that lives in bodily fluids, it can survive outside the human body for several days, which means that sharing contaminated household products is a possible source of infection,” said Dr. Christopher Labos, a McGill University cardiologist and epidemiologist, in a 2019 article.
In 2022, over 250 million people worldwide had chronic hepatitis B, and 1.1 million died from the disease. Most of the deaths were from liver damage and liver cancer. Less than 15 percent of people living with hepatitis B have been diagnosed.
How well does the vaccine protect against hepatitis B?
Hepatitis B vaccination is up to 95 percent effective, providing lasting—and possibly lifelong—protection against the virus. Depending on when the first dose is given, the complete vaccine series consists of two to three doses.
The vaccine is most effective for infants and children. The CDC recommends that infants receive it at birth for the most protection.
The first dose is followed by two to three additional doses administered before 18 months. Children, adolescents, and adults who weren’t vaccinated as infants should also receive the vaccine.
Vaccination is particularly important for high-risk groups, including health workers and those who are in close contact with individuals living with chronic hepatitis B, people who use intravenous drugs, and people receiving blood transfusions, dialysis, or organ transplants.
Is the vaccine safe?
Vaccines against hepatitis B were first developed in the 1980s, and they have been proven safe for decades. They have a low risk of serious side effects and are safe enough to be given to newborns, pregnant people, and immunocompromised people.
We also know hepatitis B vaccines work: “Between 1990 (about the time when universal hepatitis B vaccinations started) and 2006, the rate of hepatitis B infection fell by 81 percent to the lowest level ever recorded, and the decline was greatest among children,” added Labos.
Hepatitis B rates have continued to decline across all age groups, with the U.S. exceeding its goal of reducing new hepatitis B infections by 20 percent.
Why do doctors recommend the vaccine for babies?
Hepatitis B vaccination helps protect infants from a lifetime of potentially life-threatening infections and complications. Nine out of 10 unvaccinated infants infected with hepatitis B will develop chronic infections, which increases their risk of liver failure and liver cancer.
The hepatitis B vaccine is administered at birth to help prevent the virus from being transmitted from birthing parent to child. It also helps protect infants who might be in close contact with someone with hepatitis B. This is particularly important because most people who have hepatitis are undiagnosed.
Have more questions? Talk to your health care provider to learn more about hepatitis B vaccination.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Share This Post
-
Strong Bones Forever − by Dr. Raymond Hinish
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This doctor of pharmacy would like for fewer people to take (or need to take) osteoporosis medications. Indeed, as the subtitle suggests, the focus here is on drug-free solutions.
And not just because “natural is better” as an argument without evidence, rather, he talks about the limitations and drawbacks of osteoporosis medications (which we wrote about previously, but he has more room to go into more detail), whereupon some osteoporosis meds may do more harm than good.
His method boasts improvements in bone density by 11% or more in two years, and covers such topics as:
- which calcium (and why no, dairy is not what you want; it contains things that inhibit calcium absorption, so the calcium will be stuck in your arteries instead of your bones)
- which minerals are more important than calcium, and why
- common mistakes that many people make that sabotage their bone density
It’s about more than just diet though; he does also talk about hormones, and not just other lifestyle factors, but also many “industry secrets” that aren’t really secrets per se, it’s just, people outside of the industry don’t usually know them—pertaining to things like how to get the most out of bone density tests (i.e. how to get better accuracy), how to meaningfully assess fracture risk, and, if choosing to take osteoporosis meds, how to minimize the risks and maximize the benefits.
The style is very direct and informational, very easy to read, remarkably jargon-free, and our only criticism is that there is no bibliography.
Bottom line: if you’d like to improve your bone density, this book can certainly help with that.
Click here to check out Strong Bones Forever, and have strong bones forever!
Share This Post
Related Posts
-
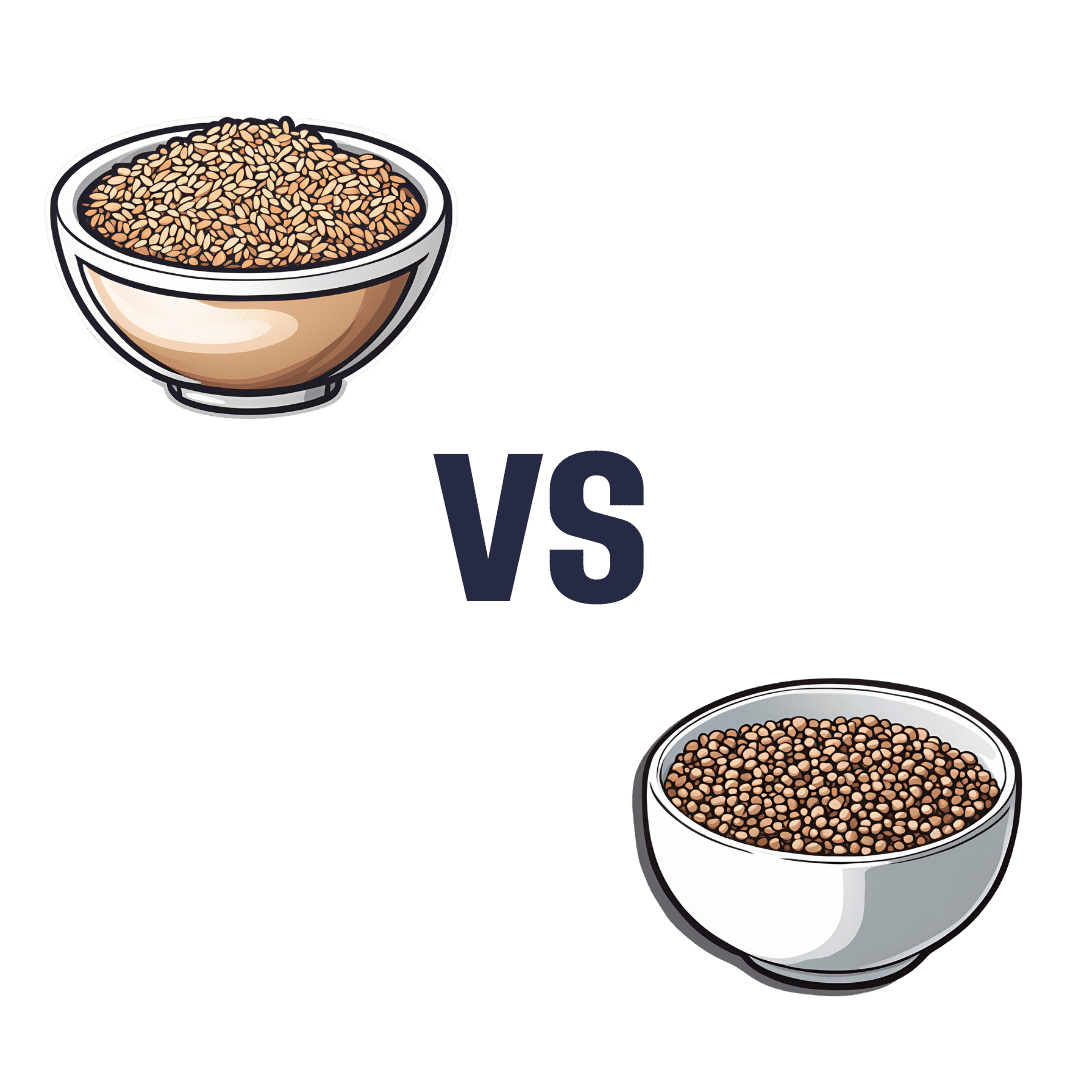
Brown Rice vs Buckwheat – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing brown rice to buckwheat, we picked the buckwheat.
Why?
In terms of macros, brown rice has more carbs, while buckwheat has nearly 2x the fiber, and more protein. An easy choice here: buckwheat for the win.
In the category of vitamins, brown rice has more of vitamins B1, B2, B3, B6, and E, while buckwheat has more of vitamins B9, K, and choline. A win for brown rice this time, although as a point in buckwheat’s favor, while most of the margins of difference are comparable, buckwheat has nearly 10x the vitamin K.
When it comes to minerals, brown rice has more manganese, phosphorus, selenium, and zinc, while buckwheat has more calcium, copper, iron, and magnesium. A win for buckwheat again this time.
A quick note on gluten: both of these are naturally gluten-free, so that’s not an issue here. Buckwheat, despite its name, is not a wheat, nor even closely related to wheat. It’s not even technically a grain; it’s a flowering plant of which we eat the groats. In taxonomic terms, buckwheat is about as related to wheat as a lionfish is to a lion.
Adding up the sections makes for an overall 2:1 win for buckwheat, though even if it weren’t for that, which is someone more likely to hear from a doctor, “you need to eat more fiber”, or “you need to eat more vitamin E”? Thus, even had the categories been tied (let’s imagine it had been tied on minerals, say) that’d have been a tiebreaker in favor of buckwheat. As it is, buckwheat already won by strength of numbers anyway.
Of course, do enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
Grains: Bread Of Life, Or Cereal Killer?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Our ‘food environments’ affect what we eat. Here’s how you can change yours to support healthier eating
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In January, many people are setting new year’s resolutions around healthy eating. Achieving these is often challenging – it can be difficult to change our eating habits. But healthy diets can enhance physical and mental health, so improving what we eat is a worthwhile goal.
One reason it’s difficult to change our eating habits relates to our “food environments”. This term describes:
The collective physical, economic, policy and sociocultural surroundings, opportunities and conditions that influence people’s food and beverage choices and nutritional status.
Our current food environments are designed in ways that often make it easier to choose unhealthy foods than healthy ones. But it’s possible to change certain aspects of our personal food environments, making eating healthier a little easier.
Unhealthy food environments
It’s not difficult to find fast-food restaurants in Australian cities. Meanwhile, there are junk foods at supermarket checkouts, service stations and sporting venues. Takeaway and packaged foods and drinks routinely come in large portion sizes and are often considered tastier than healthy options.
Our food environments also provide us with various prompts to eat unhealthy foods via the media and advertising, alongside health and nutrition claims and appealing marketing images on food packaging.
At the supermarket, unhealthy foods are often promoted through prominent displays and price discounts.
We’re also exposed to various situations in our everyday lives that can make healthy eating challenging. For example, social occasions or work functions might see large amounts of unhealthy food on offer.
Not everyone is affected in the same way
People differ in the degree to which their food consumption is influenced by their food environments.
This can be due to biological factors (for example, genetics and hormones), psychological characteristics (such as decision making processes or personality traits) and prior experiences with food (for example, learned associations between foods and particular situations or emotions).
People who are more susceptible will likely eat more and eat more unhealthy foods than those who are more immune to the effects of food environments and situations.
Those who are more susceptible may pay greater attention to food cues such as advertisements and cooking smells, and feel a stronger desire to eat when exposed to these cues. Meanwhile, they may pay less attention to internal cues signalling hunger and fullness. These differences are due to a combination of biological and psychological characteristics.
These people might also be more likely to experience physiological reactions to food cues including changes in heart rate and increased salivation.
It’s common to eat junk food in front of the TV.
PR Image Factory/ShutterstockOther situational cues can also prompt eating for some people, depending on what they’ve learned about eating. Some of us tend to eat when we’re tired or in a bad mood, having learned over time eating provides comfort in these situations.
Other people will tend to eat in situations such as in the car during the commute home from work (possibly passing multiple fast-food outlets along the way), or at certain times of day such as after dinner, or when others around them are eating, having learned associations between these situations and eating.
Being in front of a TV or other screen can also prompt people to eat, eat unhealthy foods, or eat more than intended.
Making changes
While it’s not possible to change wider food environments or individual characteristics that affect susceptibility to food cues, you can try to tune into how and when you’re affected by food cues. Then you can restructure some aspects of your personal food environments, which can help if you’re working towards healthier eating goals.
Although both meals and snacks are important for overall diet quality, snacks are often unplanned, which means food environments and situations may have a greater impact on what we snack on.
Foods consumed as snacks are often sugary drinks, confectionery, chips and cakes. However, snacks can also be healthy (for example, fruits, nuts and seeds).
Try removing unhealthy foods, particularly packaged snacks, from the house, or not buying them in the first place. This means temptations are removed, which can be especially helpful for those who may be more susceptible to their food environment.
Planning social events around non-food activities can help reduce social influences on eating. For example, why not catch up with friends for a walk instead of lunch at a fast-food restaurant.
Creating certain rules and habits can reduce cues for eating. For example, not eating at your desk, in the car, or in front of the TV will, over time, lessen the effects of these situations as cues for eating.
You could also try keeping a food diary to identify what moods and emotions trigger eating. Once you’ve identified these triggers, develop a plan to help break these habits. Strategies may include doing another activity you enjoy such as going for a short walk or listening to music – anything that can help manage the mood or emotion where you would have typically reached for the fridge.
Write (and stick to) a grocery list and avoid shopping for food when hungry. Plan and prepare meals and snacks ahead of time so eating decisions are made in advance of situations where you might feel especially hungry or tired or be influenced by your food environment.
Georgie Russell, Senior Lecturer, Institute for Physical Activity and Nutrition (IPAN), Deakin University and Rebecca Leech, NHMRC Emerging Leadership Fellow, School of Exercise and Nutrition Sciences, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is Dairy Scary?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is Dairy Scary?
Milk and milk products are popularly enjoyed as a good source of calcium and vitamin D.
In contrast, critics of dairy products (for medical reasons, rather than ethical, which is another matter entirely and beyond the scope of this article) point to risks of cancer, heart disease, and—counterintuitively—osteoporosis. We’ll focus more on the former, but touch on the latter two before closing.
Dairy & Cancer
Evidence is highly conflicting. There are so many studies with so many different results. This is partially explicable by noting that not only is cancer a many-headed beast that comes in more than a hundred different forms and all or any of them may be affected one way or another by a given dietary element, but also… Not all milk is created equal, either!
Joanna Lampe, of the Public Health Sciences division, Fred Hutchinson Cancer Research Center in Seattle, writes:
❝Dairy products are a complex group of foods and composition varies by region, which makes evaluation of their association with disease risk difficult. For most cancers, associations between cancer risk and intake of milk and dairy products have been examined only in a small number of cohort studies, and data are inconsistent or lacking❞
In her systematic review of studies, she noted, for example, that:
- Milk and dairy products contain micronutrients and several bioactive constituents that may influence cancer risk and progression
- There’s probable association between milk intake and lower risk of colorectal cancer
- There’s a probable association between diets high in calcium and increased risk of prostate cancer
- Some studies show an inverse association between intake of cultured dairy products and bladder cancer (i.e., if you eat yogurt you’re less likely to get bladder cancer)
Since that systemic review was undertaken, more research has been conducted, and the results are… Not conclusive, but converging towards a conclusion:
- Dairy products can increase or decrease cancer risk
- The increase in cancer risk seems strongest when milk is consumed in quantities that result in too much calcium. When it comes to calcium, you can absolutely have too much of a good thing—just ask your arteries!
- The decrease in cancer seems to be mostly, if not exclusively, from fermented dairy products. This usually means yogurts. The benefit here is not from the milk itself, but rather from the gut-friendly bacteria.
You may be wondering: “Hardened arteries, gut microbiome health? I thought we were talking about cancer?” and yes we are. No part of your health is an island unrelated to other parts of your health. One thing can lead to another. Sometimes we know how and why, sometimes we don’t, but it’s best to not ignore the data.
The bottom line on dairy products and cancer is:
- Consuming dairy products in general is probably fine
- Yogurt, specifically, is probably beneficial
Dairy and Heart Disease
The reason for the concern is clear enough: it’s largely assumed to be a matter of saturated fat intake.
The best combination of “large” and “recent” that we found was a three-cohort longitudinal study in 2019, which pretty much confirms what was found in smaller or less recent studies:
- There is some evidence to suggest that consumption of dairy can increase all-cause mortality in general, and death from (cancer and) cardiovascular disease in particular
- The evidence is not, however, overwhelming. It is marginal.
Dairy and Osteoporosis
Does dairy cause osteoporosis? Research here tends to fall into one of two categories when it comes to conclusions, so we’ll give an example of each:
- “Results are conflicting, saying yes/no/maybe, and basically we just don’t know”
- “Results are conflicting, but look: cross-sectional and case-control studies say yes; cohort studies say maybe or no; we prefer the cohort studies”
See them for yourself:
- Osteoporosis: Is milk a kindness or a curse?
- Consumption of milk and dairy products and risk of osteoporosis and hip fracture
Conclusion: really, the jury is very much still out on this one
Summary:
- Moderate consumption of dairy products is almost certainly fine
- More specifically: it probably has some (small) pros and some (small) cons
- Yogurt is almost certainly healthier than other dairy products, and is almost universally considered a healthy food (assuming not being full of added sugar etc, of course)
- If you’re going to have non-dairy alternatives to milk, choose wisely!
That’s all we have time for today, but perhaps in a future edition we’ll do a run-down of the pros and cons of various dairy alternatives!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: