What happens in my brain when I get a migraine? And what medications can I use to treat it?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Migraine is many things, but one thing it’s not is “just a headache”.
“Migraine” comes from the Greek word “hemicrania”, referring to the common experience of migraine being predominantly one-sided.
Some people experience an “aura” preceding the headache phase – usually a visual or sensory experience that evolves over five to 60 minutes. Auras can also involve other domains such as language, smell and limb function.
Migraine is a disease with a huge personal and societal impact. Most people cannot function at their usual level during a migraine, and anticipation of the next attack can affect productivity, relationships and a person’s mental health.

What’s happening in my brain?
The biological basis of migraine is complex, and varies according to the phase of the migraine. Put simply:
The earliest phase is called the prodrome. This is associated with activation of a part of the brain called the hypothalamus which is thought to contribute to many symptoms such as nausea, changes in appetite and blurred vision.
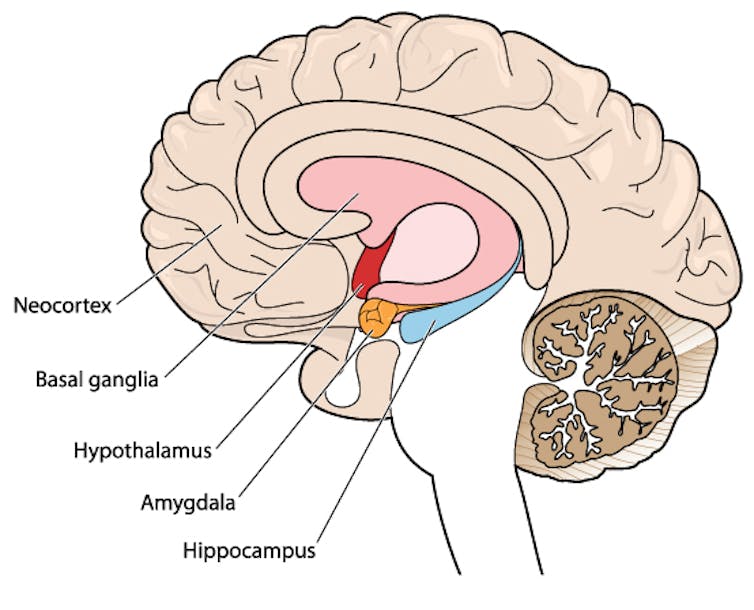
Next is the aura phase, when a wave of neurochemical changes occur across the surface of the brain (the cortex) at a rate of 3–4 millimetres per minute. This explains how usually a person’s aura progresses over time. People often experience sensory disturbances such as flashes of light or tingling in their face or hands.
In the headache phase, the trigeminal nerve system is activated. This gives sensation to one side of the face, head and upper neck, leading to release of proteins such as CGRP (calcitonin gene-related peptide). This causes inflammation and dilation of blood vessels, which is the basis for the severe throbbing pain associated with the headache.
Finally, the postdromal phase occurs after the headache resolves and commonly involves changes in mood and energy.
What can you do about the acute attack?
A useful way to conceive of migraine treatment is to compare putting out campfires with bushfires. Medications are much more successful when applied at the earliest opportunity (the campfire). When the attack is fully evolved (into a bushfire), medications have a much more modest effect.
Aspirin
For people with mild migraine, non-specific anti-inflammatory medications such as high-dose aspirin, or standard dose non-steroidal medications (NSAIDS) can be very helpful. Their effectiveness is often enhanced with the use of an anti-nausea medication.
Triptans
For moderate to severe attacks, the mainstay of treatment is a class of medications called “triptans”. These act by reducing blood vessel dilation and reducing the release of inflammatory chemicals.
Triptans vary by their route of administration (tablets, wafers, injections, nasal sprays) and by their time to onset and duration of action.
The choice of a triptan depends on many factors including whether nausea and vomiting is prominent (consider a dissolving wafer or an injection) or patient tolerability (consider choosing one with a slower onset and offset of action).
As triptans constrict blood vessels, they should be used with caution (or not used) in patients with known heart disease or previous stroke.

Gepants
Some medications that block or modulate the release of CGRP, which are used for migraine prevention (which we’ll discuss in more detail below), also have evidence of benefit in treating the acute attack. This class of medication is known as the “gepants”.
Gepants come in the form of injectable proteins (monoclonal antibodies, used for migraine prevention) or as oral medication (for example, rimegepant) for the acute attack when a person has not responded adequately to previous trials of several triptans or is intolerant of them.
They do not cause blood vessel constriction and can be used in patients with heart disease or previous stroke.
Ditans
Another class of medication, the “ditans” (for example, lasmiditan) have been approved overseas for the acute treatment of migraine. Ditans work through changing a form of serotonin receptor involved in the brain chemical changes associated with the acute attack.
However, neither the gepants nor the ditans are available through the Pharmaceutical Benefits Scheme (PBS) for the acute attack, so users must pay out-of-pocket, at a cost of approximately A$300 for eight wafers.
What about preventing migraines?
The first step is to see if lifestyle changes can reduce migraine frequency. This can include improving sleep habits, routine meal schedules, regular exercise, limiting caffeine intake and avoiding triggers such as stress or alcohol.
Despite these efforts, many people continue to have frequent migraines that can’t be managed by acute therapies alone. The choice of when to start preventive treatment varies for each person and how inclined they are to taking regular medication. Those who suffer disabling symptoms or experience more than a few migraines a month benefit the most from starting preventives.

Almost all migraine preventives have existing roles in treating other medical conditions, and the physician would commonly recommend drugs that can also help manage any pre-existing conditions. First-line preventives include:
- tablets that lower blood pressure (candesartan, metoprolol, propranolol)
- antidepressants (amitriptyline, venlafaxine)
- anticonvulsants (sodium valproate, topiramate).
Some people have none of these other conditions and can safely start medications for migraine prophylaxis alone.
For all migraine preventives, a key principle is starting at a low dose and increasing gradually. This approach makes them more tolerable and it’s often several weeks or months until an effective dose (usually 2- to 3-times the starting dose) is reached.
It is rare for noticeable benefits to be seen immediately, but with time these drugs typically reduce migraine frequency by 50% or more.
‘Nothing works for me!’
In people who didn’t see any effect of (or couldn’t tolerate) first-line preventives, new medications have been available on the PBS since 2020. These medications block the action of CGRP.
The most common PBS-listed anti-CGRP medications are injectable proteins called monoclonal antibodies (for example, galcanezumab and fremanezumab), and are self-administered by monthly injections.
These drugs have quickly become a game-changer for those with intractable migraines. The convenience of these injectables contrast with botulinum toxin injections (also effective and PBS-listed for chronic migraine) which must be administered by a trained specialist.
Up to half of adolescents and one-third of young adults are needle-phobic. If this includes you, tablet-form CGRP antagonists for migraine prevention are hopefully not far away.
Data over the past five years suggest anti-CGRP medications are safe, effective and at least as well tolerated as traditional preventives.
Nonetheless, these are used only after a number of cheaper and more readily available first-line treatments (all which have decades of safety data) have failed, and this also a criterion for their use under the PBS.
Mark Slee, Associate Professor, Clinical Academic Neurologist, Flinders University and Anthony Khoo, Lecturer, Flinders University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Menopause Brain – by Dr. Lisa Mosconi
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
With her PhD in neuroscience and nuclear medicine (a branch of radiology, used for certain types of brain scans, amongst other purposes), whereas many authors will mention “brain fog” as a symptom of menopause, Dr. Mosconi can (and will) point to a shadowy patch on a brain scan and say “that’s the brain fog, there”.
And so on for many other symptoms of menopause that are commonly dismissed as “all in your head”, notwithstanding that “in your head” is the worst place for a problem to be. You keep almost your entire self in there!
Dr. Mosconi covers how hormones influence not just our moods in a superficial way, but also change the structure of our brain over time.
Importantly, she also gives an outline of how to stay on the ball; what things to watch out for when your doctor probably won’t, and what things to ask for when your doctor probably won’t suggest them.
Bottom line: if menopause is a thing in your life (or honestly, even if it isn’t but you are running on estrogen rather than testosterone), then this is a book for you.
Click here to check out The Menopause Brain, and look after yours!
Share This Post
-
What Mattress Is Best, By Science?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Foundations of Good Sleep
You probably know the importance of good sleep for good health. If not, here’s a quick refresher:
- Why You Probably Need More Sleep
- How Sleep-Deprived Are You, Really?
- The 6 Dimensions Of Sleep (And Why They Matter)
You should also definitely check out this quite famous book on the topic:
Why We Sleep – by Dr Matthew Walker
What helps, to get that good sleep
We’ve covered this a little before too, for example:
- Safe Effective Sleep Aids For Seniors
- Sleep Better With Better Air
- How To Nap Like A Pro (No More “Sleep Hangovers”!)
How to level-up from there
One of the biggest barriers to good sleep for many people is obstructive sleep apea:
Healthier, Natural Sleep Without Obstruction!
We covered (in the above article) a whole lot of ways of mitigating/managing obstructive sleep apnea. One of the things we mentioned as beneficial was avoiding sleeping on one’s back, and this is something Mayo Clinic’s Dr. Somers agreed with:
Back Sleeping, And Sleeping Differently After 50
“But side-sleeping is uncomfortable”
If this is you, then chances are you have the wrong mattress.
If your mattress is too firm, you can get around it by using this “five pillow” method:
Click Here If The Embedded Video Doesn’t Load Automatically
If your mattress is too soft, then sorry, you really just have to throw that thing out and start again.
The Goldilocks mattress
While different people will have different subjective preferences, the science is quite clear on what is actually best for people’s spines. As this review of 39 qualified scholarly articles concluded:
❝Results of this systematic review show that a medium-firm mattress promotes comfort, sleep quality and rachis alignment❞
~ Dr. Gianfilippo Caggiari et al.
Read in full: What type of mattress should be chosen to avoid back pain and improve sleep quality? Review of the literature
Note: to achieve “medium-firm” that remains “medium firm” has generally been assumed to require a memory-foam mattress.
How memory-foam works: memory-foam is a moderately thermosoftening material, designed to slightly soften at the touch of human body temperature, and be firmer at room temperature. This will result in it molding itself to the form of a human body, providing what amounts to personalized support for your personal shape and size, meaning your spine can stay exactly as it’s supposed to when you’re sleeping on your side, instead of (for example) your hips being wider meaning that your lumbar vertebrae are raised higher than your thoracic vertebrae, giving you the equivalent of a special nocturnal scoliosis.
It will, therefore, stop working if
- the ambient temperature is comparable to human body temperature (as happens in some places sometimes, and increasingly often these days)
- you die, and thus lose your body temperature (but in that case, your spinal alignment will be the least of your concerns)
Here’s a good explanation of the mechanics of memory foam from the Sleep Foundation:
Sleep Foundation | What is Memory Foam?
An alternative to memory foam?
If you don’t like memory foam (one criticism is that it doesn’t allow good ventilation underneath the body), there is an alterative, the grid mattress.
It’s very much “the new kid on the block” and the science is young for this, but for example this recent (April 2024) study that concluded:
❝The grid mattress is a simple, noninvasive, and nonpharmacological intervention that improved adults sleep quality and health. Controlled trials are encouraged to examine the effects of this mattress in a variety of populations and environments.❞
~ Dr. Heather Hausenblas et al.
Read in full: Effectiveness of a grid mattress on adults’ sleep quality and health: A quasi-experimental intervention study
However, that was a small (n=39) uncontrolled (i.e. there was no control group) study, and the conflict of interest statement is, well, interesting:
❝Heather A. Hausenblas, Stephanie L. Hooper, Martin Barragan, and Tarah Lynch declare no conflict of interest. Michael Breus served as a former consultant for Purple, LLC.❞
~ Ibid.
…which is a fabulous way of distracting from the mention in the “Acknowledgements” section to follow, that…
❝Purple, LLC, provided financial support for the study❞
~ Ibid.
Purple is the company that invented the mattress being tested. So while this doesn’t mean the study is necessarily dishonest and/or corrupt, it does at the very least raise a red flag for a potential instance of publication bias (because Purple may have funded multiple studies and then pulled funding of the ones that weren’t going their way).
If you are interested in Purple’s mattress and how it works, you can check it out here ← this is a link for your interest and information; not an advertisement or an endorsement. We look forward to seeing more science for this though, and echo their own call for randomized controlled trials!
Summary
Sleep is important, and while it’s a popular myth that we need less as we get older, the truth is that we merely get less on average, while still needing the same amount.
A medium-firm memory-foam mattress is a very good, well-evidenced way to support that (both figuratively and literally!).
A grid mattress is an interesting innovation, and/but we’d like to see more science for it.
Take care!
Share This Post
-
It’s A Wrap
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We hope all our readers have had a great and healthy week! Here are some selections from health news from around the world:
A lack of transparency
Thousands of chemicals blanket-approved for food contact in packaging, under the FDA’s “Generally Recognized As Safe” umbrella, have been found in humans.
This highlights a gap in the safeguarding system, because the GRAS classification is given when there’s no known significant association with disease—but in this case, a problem can occur when the build-up in the blood and brain cause problems much later.
Read in full: Thousands of toxins from food packaging found in humans – research
Learn more: We Are Such Stuff As Bottles Are Made Of (It’s Not Fantastic To Be Plastic)
Cafestol for weight loss?
Most coffee intervention studies use instant coffee. Which is understandable; they are scientists on a budget, not coffee shop baristas. But, instant coffee is low in some of coffee’s important compounds, such as cafestol—which as it turns out, can lower not only overall body fat, but also (importantly!) visceral fat.
Read in full: 12-week coffee compound study shows promising results for weight and fat reduction in at-risk individuals
Learn more: The Bitter Truth About Coffee (or is it?)
Doing something is better than doing nothing
While a lot of the bad news both locally and around the world can be infuriating and/or depressing, turning a blind eye may not be the best approach for dealing with it. This study was in teens, but it’s likely that the benefits are similar for other ages too:
Read in full: Racial justice activism, advocacy found to reduce depression, anxiety in some teens
Learn more: Make Social Media Work For Your Mental Health
A ray of hope!
Sometimes, the topic of sun and sunscreens can seem like “damned if you do; damned if you don’t”, with regard to the harmful effects of the sun, and in some cases, potentially harmful effects of some sunscreen chemicals. We’ve argued ultimately in favor of sunscreens in this tug-of-war, but it’s nice to see improvements being made, in this case, with lignin-based sunscreen (a plant-based by-product of the pulp industry).
Read in full: Researchers create high-performing, eco-friendly sunscreen
Learn more: Who Screens The Sunscreens?
All about the pores
Researchers have identified a protein, and from that, a stack of protein fragments, that are involved in the formation of large pores. This is important, as it’s pointing to a means of relief for a lot of inflammatory diseases.
Read in full: Scientists unravel the process of pore formation in cells
Learn more: Why Do We Have Pores, And Could We Not?
Getting to the bottom of Crohn’s
If you have Crohn’s, or perhaps someone close to you has it, then you’ll be familiar with the common medical refrain of “we don’t know”. While this honesty is laudable, it’s not reassuring. So, it’s good that researchers are making progress in understanding why many people with Crohn’s may respond differently not only to lifestyle interventions, but also to various relevant drugs—allowing doctors to prescribe the right treatment for the right person.
Read in full: Patient-derived gut organoids reveal new insights into Crohn’s disease subtypes
Learn more: Diet Tips for Crohn’s Disease
Another carotenoid that holds back Alzheimer’s
Phytoene is a carotenoid that is found in many red, orange, or yellow foods, including tomatoes, carrots, apricots, red peppers, oranges, mandarins and passion fruit, among others. Researchers have found that it slows the onset of symptoms associated with the formation of amyloid plaques, by 30–40%, and increases longevity by 10–19%:
Read in full: Carotenoid phytoene shows potential in slowing Alzheimer’s plaque formation and increasing lifespan
Learn more: Brain Food? The Eyes Have It! ← this is about a different carotenoid, lutein, found mostly in dark green leafy vegetables, but it’s best to enjoy both 😎
Take care!
Share This Post
Related Posts
-
Studies of Parkinson’s disease have long overlooked Pacific populations – our work shows why that must change
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
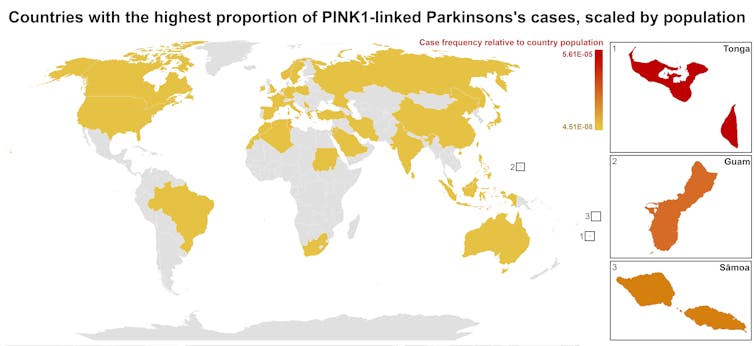
A form of Parkinson’s disease caused by mutations in a gene known as PINK1 has long been labelled rare. But our research shows it’s anything but – at least for some populations.
Our meta-analysis revealed that people in specific Polynesian communities have a much higher rate of PINK1-linked Parkinson’s than expected. This finding reshapes not only our understanding of who is most at risk, but also how soon symptoms may appear and what that might mean for treatment and testing.
Parkinson’s disease is often thought of as a single condition. In reality, it is better understood as a group of syndromes caused by different factors – genetic, environmental or a combination of both.
These varying causes lead to differences in disease patterns, progression and subsequent diagnosis. Recognising this distinction is crucial as it paves the way for targeted interventions and may even help prevent the disease altogether.
Shutterstock/sfam_photo Why we focus on PINK1-linked Parkinson’s
We became interested in this gene after a 2021 study highlighted five people of Samoan and Tongan descent living in New Zealand who shared the same PINK1 mutation.
Previously, this mutation had been spotted only in a few more distant places –Malaysia, Guam and the Philippines. The fact it appeared in people from Samoan and Tongan backgrounds suggested a historical connection dating back to early Polynesian migrations.
One person in 1,300 West Polynesians carries this mutation. This is a frequency well above what scientists usually classify as rare (below one in 2,200). This discovery means we may be overlooking entire communities in Parkinson’s research if we continue to assume PINK1-linked cases are uncommon.
This world map shows people in some Polynesian communities have a much higher rate of PINK1-linked Parkinson’s than the global population. Eden Yin, CC BY-SA Traditional understanding says PINK1-linked Parkinson’s is both rare and typically strikes younger people, mostly in their 30s or 40s, if they inherit two faulty copies of the gene. In other words, it’s considered a recessive condition, needing two matching puzzle pieces before the disease can unfold.
Our work challenges this view. We show that even one defective PINK1 gene can cause Parkinson’s at an average age of 43, much earlier than the typical onset after 65. That’s a significant departure from the standard belief that only people with two defective gene copies are at risk.
Why this matters for people with the disease
It’s not just genetics that challenge long-held views. Historically, PINK1-linked Parkinson’s was thought to lack some of the classic features of the disease, such as toxic clumps of alpha-synuclein protein.
In typical Parkinson’s, alpha-synuclein builds up in the brain, forming sticky clumps known as Lewy bodies. Our results, contrary to prior beliefs, show that alpha-synuclein pathology is present in 87.5% of PINK1 cases. This finding opens up a promising new avenue for future treatment development.
The biggest concern is early onset. PINK1-linked Parkinson’s can begin as early as 11 years old, although a more common starting point is around the mid-30s. This early onset means living longer with the disease, which can profoundly affect education, work opportunities and family life.
Current treatments (such as levodopa, a precursor of dopamine) help manage symptoms, but they’re not designed to address the root cause. If we know someone has a PINK1 mutation, scientists and clinicians can explore therapies for specific genetic pathways, potentially delivering relief beyond symptom management.
Sex differences add a layer of complexity
In Parkinson’s, generally, men are at higher risk and tend to develop symptoms earlier. However, our findings suggest the opposite pattern for PINK1-linked cases. Particularly, women with two defective copies of the gene experience onset earlier than men.
This highlights the need to consider sex-related factors in Parkinson’s research. Overlooking them risks missing key elements of the disease.
Genetic testing could be a game-changer for PINK1-linked Parkinson’s. Because it often appears earlier, doctors may not recognise it immediately, especially if they are more familiar with the common, later-onset form of Parkinson’s.
Early genetic testing could lead to a faster, more accurate diagnosis, allowing treatment to begin when interventions are most effective. It would help families understand how the disease is inherited, enabling relatives to get tested.
In some cases, where appropriate and culturally acceptable, embryo screening may be considered to prevent the passing of the faulty gene.
Knowing you have a PINK1 mutation could also make finding the right treatment more efficient. Instead of a lengthy trial-and-error process with different medications, doctors could use emerging therapies designed to target the underlying PINK1 mutation rather than relying on general Parkinson’s treatments meant for the broader population.
Addressing research gaps
These findings underscore how crucial it is to include diverse populations in health research.
Many communities, such as those in Samoa, Tonga and other Pacific nations, have had little to no involvement in global Parkinson’s genetics studies. This has created gaps in knowledge and real-world consequences for people who may not receive timely or accurate diagnoses.
Researchers, funding bodies and policymakers must prioritise projects beyond the usual focus on European or industrialised countries to ensure research findings and treatments are relevant to all affected populations.
To better diagnose and treat Parkinson’s, we need a more inclusive approach. Recognising that PINK1-linked Parkinson’s is not as rare as previously thought – and that genetics, sex differences and cultural factors all play a role – allows us to improve care for everyone.
By expanding genetic testing, refining treatments and ensuring research reflects the full spectrum of Parkinson’s, we can move closer to more precise diagnoses, targeted therapies and better support systems for all.
Victor Dieriks, Research Fellow in Health Sciences, University of Auckland, Waipapa Taumata Rau and Eden Paige Yin, PhD candidate in Health Sciences, University of Auckland, Waipapa Taumata Rau
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Foam Rolling – by Karina Inkster
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you’ve ever bought a foam roller only to place it under your lower back once and then put it somewhere for safekeeping and never use it again, this book will help fix that.
Karina Inkster (what a cool name) is a personal trainer, and the book also features tips and advice from physiotherapists and sports medicine specialist doctors too, so all bases are well and truly covered.
This is not, in case you’re wondering, a book that could have been a pamphlet, with photos of the exercises and one-liner explanation and that’s it. Rather, Inkster takes us through the anatomy and physiology of what’s going on, so that we can actually use this thing correctly and get actual noticeable improvements to our health from it—as promised in the subtitle’s mention of “for massage, injury prevention, and core strength”. To be clear, a lot of it is also about soft tissue mobilization, and keeping our fascia healthy (an oft-underestimated aspect of general mobility).
We would mention that since the photos are pleasantly colorful (like those on the cover) and this adds to the clarity, we’d recommend springing for the (quite inexpensive) physical copy, rather than a Kindle edition (if your e-reader is a monochrome e-ink device like this reviewer’s, anyway).
Bottom line: this book will enable your foam roller to make a difference to your life.
Click here to check out Foam Rolling, and get rolling (correctly)!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Seeds: The Good, The Bad, And The Not-Really-Seeds!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Doctors are great at saving lives like mine. I’m a two time survivor of colon cancer and have recently been diagnosed with Chron’s disease at 62. No one is the health system can or is prepared to tell me an appropriate diet to follow or what to avoid. Can you?❞
Congratulations on the survivorship!
As to Crohn’s, that’s indeed quite a pain, isn’t it? In some ways, a good diet for Crohn’s is the same as a good diet for most other people, with one major exception: fiber
…and unfortunately, that changes everything, in terms of a whole-foods majority plant-based diet.
What stays the same:
- You still ideally want to eat a lot of plants
- You definitely want to avoid meat and dairy in general
- Eating fish is still usually* fine, same with eggs
- Get plenty of water
What needs to change:
- Consider swapping grains for potatoes or pasta (at least: avoid grains)
- Peel vegetables that are peelable; discard the peel or use it to make stock
- Consider steaming fruit and veg for easier digestion
- Skip spicy foods (moderate spices, like ginger, turmeric, and black pepper, are usually fine in moderation)
Much of this latter list is opposite to the advice for people without Crohn’s Disease.
*A good practice, by the way, is to keep a food journal. There are apps that you can get for free, or you can do it the old-fashioned way on paper if prefer.
But the important part is: make a note not just of what you ate, but also of how you felt afterwards. That way, you can start to get a picture of patterns, and what’s working (or not) for you, and build up a more personalized set of guidelines than anyone else could give to you.
We hope the above pointers at least help you get going on the right foot, though!
❝Why do baked goods and deep fried foods all of a sudden become intolerable? I used to b able to ingest bakery foods and fried foods. Lately I developed an extreme allergy to Kiwi… what else should I “fear”❞
About the baked goods and the deep-fried foods, it’s hard to say without more information! It could be something in the ingredients or the method, and the intolerance could be any number of symptoms that we don’t know. Certainly, pastries and deep-fried foods are not generally substantial parts of a healthy diet, of course!
Kiwi, on the other hand, we can answer… Or rather, we can direct you to today’s “What’s happening in the health world” section below, as there is news on that front!
We turn the tables and ask you a question!
We’ll then talk about this tomorrow:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: