What are heart rate zones, and how can you incorporate them into your exercise routine?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you spend a lot of time exploring fitness content online, you might have come across the concept of heart rate zones. Heart rate zone training has become more popular in recent years partly because of the boom in wearable technology which, among other functions, allows people to easily track their heart rates.
Heart rate zones reflect different levels of intensity during aerobic exercise. They’re most often based on a percentage of your maximum heart rate, which is the highest number of beats your heart can achieve per minute.
But what are the different heart rate zones, and how can you use these zones to optimise your workout?
The three-zone model
While there are several models used to describe heart rate zones, the most common model in the scientific literature is the three-zone model, where the zones may be categorised as follows:
- zone 1: 55%–82% of maximum heart rate
- zone 2: 82%–87% of maximum heart rate
- zone 3: 87%–97% of maximum heart rate.
If you’re not sure what your maximum heart rate is, it can be calculated using this equation: 208 – (0.7 × age in years). For example, I’m 32 years old. 208 – (0.7 x 32) = 185.6, so my predicted maximum heart rate is around 186 beats per minute.
There are also other models used to describe heart rate zones, such as the five-zone model (as its name implies, this one has five distinct zones). These models largely describe the same thing and can mostly be used interchangeably.
What do the different zones involve?
The three zones are based around a person’s lactate threshold, which describes the point at which exercise intensity moves from being predominantly aerobic, to predominantly anaerobic.
Aerobic exercise uses oxygen to help our muscles keep going, ensuring we can continue for a long time without fatiguing. Anaerobic exercise, however, uses stored energy to fuel exercise. Anaerobic exercise also accrues metabolic byproducts (such as lactate) that increase fatigue, meaning we can only produce energy anaerobically for a short time.
On average your lactate threshold tends to sit around 85% of your maximum heart rate, although this varies from person to person, and can be higher in athletes.

In the three-zone model, each zone loosely describes one of three types of training.
Zone 1 represents high-volume, low-intensity exercise, usually performed for long periods and at an easy pace, well below lactate threshold. Examples include jogging or cycling at a gentle pace.
Zone 2 is threshold training, also known as tempo training, a moderate intensity training method performed for moderate durations, at (or around) lactate threshold. This could be running, rowing or cycling at a speed where it’s difficult to speak full sentences.
Zone 3 mostly describes methods of high-intensity interval training, which are performed for shorter durations and at intensities above lactate threshold. For example, any circuit style workout that has you exercising hard for 30 seconds then resting for 30 seconds would be zone 3.
Striking a balance
To maximise endurance performance, you need to strike a balance between doing enough training to elicit positive changes, while avoiding over-training, injury and burnout.
While zone 3 is thought to produce the largest improvements in maximal oxygen uptake – one of the best predictors of endurance performance and overall health – it’s also the most tiring. This means you can only perform so much of it before it becomes too much.
Training in different heart rate zones improves slightly different physiological qualities, and so by spending time in each zone, you ensure a variety of benefits for performance and health.
So how much time should you spend in each zone?
Most elite endurance athletes, including runners, rowers, and even cross-country skiers, tend to spend most of their training (around 80%) in zone 1, with the rest split between zones 2 and 3.
Because elite endurance athletes train a lot, most of it needs to be in zone 1, otherwise they risk injury and burnout. For example, some runners accumulate more than 250 kilometres per week, which would be impossible to recover from if it was all performed in zone 2 or 3.
Of course, most people are not professional athletes. The World Health Organization recommends adults aim for 150–300 minutes of moderate intensity exercise per week, or 75–150 minutes of vigorous exercise per week.
If you look at this in the context of heart rate zones, you could consider zone 1 training as moderate intensity, and zones 2 and 3 as vigorous. Then, you can use heart rate zones to make sure you’re exercising to meet these guidelines.
What if I don’t have a heart rate monitor?
If you don’t have access to a heart rate tracker, that doesn’t mean you can’t use heart rate zones to guide your training.
The three heart rate zones discussed in this article can also be prescribed based on feel using a simple 10-point scale, where 0 indicates no effort, and 10 indicates the maximum amount of effort you can produce.
With this system, zone 1 aligns with a 4 or less out of 10, zone 2 with 4.5 to 6.5 out of 10, and zone 3 as a 7 or higher out of 10.
Heart rate zones are not a perfect measure of exercise intensity, but can be a useful tool. And if you don’t want to worry about heart rate zones at all, that’s also fine. The most important thing is to simply get moving.
Hunter Bennett, Lecturer in Exercise Science, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How does the drug abemaciclib treat breast cancer?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The anti-cancer drug abemaciclib (also known as Vernezio) has this month been added to the Australian Pharmaceutical Benefits Scheme (PBS) to treat certain types of breast cancer.
This significantly reduces the cost of the drug. A patient can now expect to pay A$31.60 for a 28-day supply ($7.70 with a health care concession card). The price of abemaciclib without government subsidy is $4,250.
So what is abemaciclib, and how did we get to this point?
It stops cells dividing
Researchers at the pharmaceutical company Eli Lilly developed abemaciclib and published the first study on the drug (then known as LY2835219) in 2014.
Abemaciclib is a type of drug known as a “cyclin-dependent kinase inhibitor”. It’s taken as a pill twice a day.
To maintain our health, many of the cells in our bodies need to grow and divide to produce new cells. Cancers develop when cells grow and divide out of control. Therefore, stopping cells from dividing into new cells is one way that cancer can be fought.
When cells divide, they have to make a copy of their DNA to pass onto the new cell. “Cyclin-dependent kinases” (CDKs for short) are essential for this process. So, if you stop the CDKs, you stop the DNA copying, you stop cells dividing, and you fight the cancer.
However, there are different types of CDKs, and not all cancers need them all to grow. Abemaciclib specifically targets CDK4 and CDK6. Thankfully, a lot of cancers do need these CDKs, including some breast cancers.
The drug targets CDK4 and CDK6. Photoroyalty/Shutterstock But abemaciclib will only be effective against cancers that rely on CDK4 and CDK6 for continued growth. This specificity also means abemaciclib is fairly unique, so it can’t easily be replaced with a different drug.
Two other CDK4/6 inhibitors were developed around the same time as abemaciclib, and are called ribociclib and palbociclib. Both of these drugs are also on the PBS for specific types of breast cancer. As the drugs differ in their chemical structures, they have slight differences in the way they are taken up and processed by the body. The preferred drug given to a breast cancer patient will depend on their unique circumstances.
What are the side effects?
Research is still ongoing into the differences between each of these CDK4/6 inhibitors, but it is known that the side effects are largely similar, but can differ in severity.
The most common side effects of abemaciclib are fatigue, diarrhoea and neutropenia (reduced white blood cells). The gastrointestinal issues are generally more severe with abemaciclib.
If these side effects are too severe, abemaciclib treatment can be stopped.
What types of cancer has abemaciclib been approved for?
In 2017, the United States Food and Drug Administration (FDA) approved abemaciclib for the treatment of patients with metastatic HR+/HER2- (hormone receptor-positive and human epidermal growth factor receptor 2-negative) breast cancer who did not respond to standard endocrine therapy.
Australia’s Therapeutic Goods Administration (TGA) similarly approved abemaciclib in 2022 as an “adjuvant” therapy (after the initial surgery to remove the tumour) for patients with HR+/HER2- invasive early breast cancer which had spread to lymph nodes and was at high risk of returning.
The drug is approved for people with early breast cancer which is at high risk of returning. PeopleImages.com – Yuri A/Shutterstock As of May 1 2024, the PBS covers this use of abemaciclib in combination with endocrine therapy such as fulvestrant, which is also listed on the PBS. Endocrine therapy, also known as hormonal therapy, blocks hormone receptor positive (HR+) cancers from receiving the hormones they need to survive.
Could abemaciclib be used for other cancers in the future?
Abemaciclib is of great interest to scientists and medical practitioners, and testing is ongoing to assess the effectiveness of abemaciclib in treating a range of other cancers, including gastrointestinal cancers and blood cancers.
Abemaciclib may even be usable in brain cancers, as it has long been known to be capable of crossing the blood-brain barrier, a common stumbling block for potential anti-cancer drugs.
Time will tell whether the role of abemaciclib in health care will be expanded. But for now, its inclusion on the PBS is sure to bring some relief to breast cancer patients nationwide.
Sarah Diepstraten, Senior Research Officer, Blood Cells and Blood Cancer Division, Walter and Eliza Hall Institute and John (Eddie) La Marca, Senior Resarch Officer, Walter and Eliza Hall Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Survival of the Prettiest – by Dr. Nancy Etcoff
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Beauty is in the eye of the beholder, right? And what does it matter, in this modern world, especially if we are already in a happy stable partnership?
The science of it, as it turns out, is less poetic. Not only is evolutionary psychology still the foundation of our perception of human beauty (yes, even if we have zero possibility of further procreation personally), but also, its effects are far, far wider than partner selection.
From how nice people are to you, to how much they trust you, to how easily they will forgive a (real or perceived) misdeed, to what kind of medical care you get (or don’t), your looks shape your experiences.
In this very easy-reading work that nevertheless contains very many references, Dr. Etcoff explores the science of beauty. Not just what traits are attractive and why, but also, what they will do for (or against) us—in concrete terms, with numbers.
Bottom line: if you’d like to better understand the subconscious biases held by yourself and others, this book is a top-tier primer.
Share This Post
-
Moringa Oleifera Against CVD, Diabetes, Alzheimer’s & Arsenic?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Healthiest Drumstick
Moringa oleifera is a tree, whose leaves and pods have medicinal properties (as well as simply being very high in nutrients). It’s also called the drumstick tree in English, but equally often it’s referred to simply as Moringa. It has enjoyed use in traditional medicine for thousands of years, and its many benefits have caught scientists’ attention more recently. For an overview before we begin, see:
Now, let’s break it down…
Anti-inflammatory
It is full of antioxidants, which we’ll come to shortly, and they have abundant anti-inflammatory effects. Research into these so far has mostly beennon-human animal studies or else in vitro, hence the guarded “potential” for now:
Potential anti-inflammatory phenolic glycosides from the medicinal plant Moringa oleifera fruits
Speaking of potential though, it has been found to also reduce neuroinflammation specifically, which is good, because not every anti-inflammatory agent does that:
Antioxidant
It was hard to find studies that talked about its antioxidant powers that didn’t also add “and this, and this, and this” because of all its knock-on benefits, for example:
❝The results indicate that this plant possesses antioxidant, hypolipidaemic and antiatherosclerotic activities and has therapeutic potential for the prevention of cardiovascular diseases.
These effects were at degrees comparable to those of simvastatin.❞
~ Dr. Pilaipark Chumark et al.
Likely a lot of its benefits in these regards come from the plant’s very high quercetin content, because quercetin does that too:
Quercetin reduces blood pressure in hypertensive subjects
For more about quercetin, you might like our previous main feature:
Fight Inflammation & Protect Your Brain, With Quercetin
Antidiabetic
It also has been found to lower fasting blood sugar levels by 13.5%:
Anti-arsenic?
We put a question mark there, because studies into this have only been done with non-human animals such as mice and rats so far, largely because there are not many human volunteers willing to sign up for arsenic poisoning (and no ethics board would pass it anyway).
However, as arsenic contamination in some foods (such as rice) is a big concern, this is very promising. Here are some example studies, with mice and rats respectively:
- Protective effects of Moringa oleifera Lam. leaves against arsenic-induced toxicity in mice
- Therapeutic effects of Moringa oleifera on arsenic-induced toxicity in rats
Is it safe?
A popular food product through parts of Africa and (especially) South & West Asia, it has a very good safety profile. Generally the only health-related criticism of it is that it contains some anti-nutrients (that hinder bioavailability of its nutrients), but the nutrients outweigh the antinutrients sufficiently to render this a trifling trivium.
In short: as ever, do check with your doctor/pharmacist to be sure, but in general terms, this is about as safe as most vegan whole foods; it just happens to also be something of a superfood, which puts it into the “nutraceutical” category. See also:
Review of the Safety and Efficacy of Moringa oleifera
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Share This Post
Related Posts
-
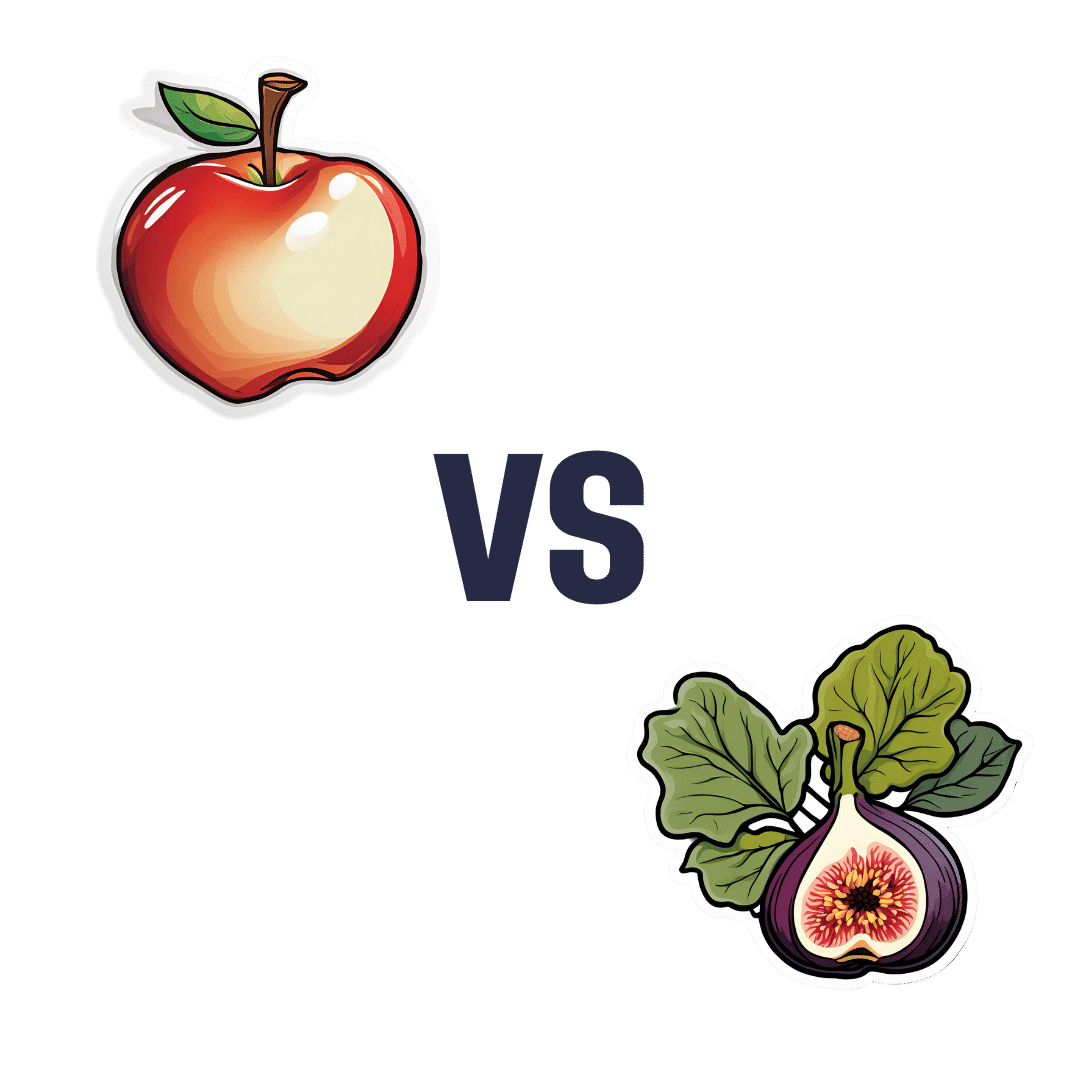
Apples vs Figs – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing apples to figs, we picked the figs.
Why?
These two fruits are both known for being quite rich in sugar (but also rich in fiber, which offsets it metabolically), and indeed their macros are quite similar. That said, figs have slightly more protein, fiber, and carbs. Both are considered low glycemic index foods. We can consider this category a tie, or perhaps a nominal win for apples, whose glycemic index is the lower of the two. But since figs’ GI is also low, it’s really not a deciding factor.
In terms of vitamins, apples have more of vitamins C and E, while figs have more of vitamins A, B1, B2, B3, B5, B6, B9, and choline, with noteworthy margins of difference. A clear for figs here.
When it comes to minerals, apples are not higher in any minerals, while figs are several times higher in calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. An overwhelming win for figs.
Of course, enjoy either or both, but if you want nutritional density, apples simply cannot compete with figs.
Want to learn more?
You might like to read:
Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Science of Stretch – by Dr. Leada Malek
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book is part of a “Science of…” series, of which we’ve reviewed some others before (Yoga | HIIT | Pilates), and needless to say, we like them.
You may be wondering: is this just that thing where a brand releases the same content under multiple names to get more sales, and no, it’s not (long-time 10almonds readers will know: if it were, we’d say so!).
While flexibility and mobility are indeed key benefits in yoga and Pilates, they looked into the science of what was going on in yoga asanas and Pilates exercises, stretchy or otherwise, so the stretching element was not nearly so deep as in this book.
In this one, Dr. Malek takes us on a wonderful tour of (relevant) human anatomy and physiology, far deeper than most pop-science books go into when it comes to stretching, so that the reader can really understand every aspect of what’s going on in there.
This is important, because it means busting a lot of myths (instead of busting tendons and ligaments and things), understanding why certain things work and (critically!) why certain things don’t, how certain stretching practices will sabotage our progress, things like that.
It’s also beautifully clearly illustrated! The cover art is a fair representation of the illustrations inside.
Bottom line: if you want to get serious about stretching, this is a top-tier book and you won’t regret it.
Click here to check out Science of Stretching, and learn what you can do and how!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Sunflower Oil vs Canola Oil – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing sunflower oil to canola oil, we picked the sunflower oil.
Why?
They’re both terrible! But canola oil is worse. Sunflower oil is marketed as being higher in polyunsaturated fats, which it is, albeit not by much.
Canola oil is very bad for the heart, and sunflower oil is only moderately bad for the heart, to the point that it can be heart-neutral if used sparingly.
As seed oils, they are both sources of vitamin E, but you’d need to drink a cup of oil to get your daily dose, so please just eat some seeds (or nuts, or fruit, or something) instead. It can even be sunflower seeds if you like! Rapeseed* itself (the seed that canola oil is made from) isn’t really sold as a foodstuff, so that one’s less of an option.
*Fun fact: if you’re N. American and wondering what this “rapeseed” is, know that most of the rest of the Anglosphere calls canola oil “rapeseed oil”, as it’s made from rapeseed, which comes from a plant called rape, whose name is unrelated to the crime of the same name, and comes from rāpa, the Latin word for turnip. Anyway, “canola” is a portmanteau of “Canadian” and “Ola” meaning oil, and is a trademark that has made its way into generic use throughout N. America, as a less alarming name.
Back to health matters: while sunflower seeds are healthy in moderation, the ultraprocessed and refined sunflower and canola oils are not.
Canola oil has also been found to be implicated in age-related cognitive decline, whereas sunflower oil has had mixed results in that regard.
In summary
Sunflower oil is relatively, and we stress relatively, healthier than canola oil. Please use a healthier oil than either if you can. Olive oil is good for most things, and if you need something with a higher smoke point (and/or less distinctive flavor), consider avocado oil, which is also very healthy and whose smoke point is even higher than the seed oils we’ve been discussing today.
Want to know more?
Check out:
Avocado Oil vs Olive Oil – Which is Healthier?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: