Veg in One Bed New Edition – by Huw Richards
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We all know that growing our own veg is ultimately not only healthier on the plate, but also a very healthy activity. Cheaper too. So why don’t more of us do it?
For many of us, it’s a matter of not having the skills or knowledge to do so. This book bridges that knowledge-gap.
Richards gives, as promised, a month-by-month well-illustrated guide to growing a wide variety of vegetables. He does, by the way, assume that we are in a temperate climate in the Northern Hemisphere. So if you’re not, you may need to make some adjustments.
The book doesn’t assume prior knowledge, and does give the reader everything we need from an initial basic shopping list onwards.
A particular strength of this book is that it’s about growing veg in a single raised bed—this ensures keeping everything very manageable.
Bottom line: if you have ever thought it would be good to grow your own veg, but didn’t know where to start and want something practical for a beginner, this is an excellent guide that will get you going!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Worst Cookware Lurking In Your Kitchen (Toxicologist Explains)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Yvonne Burkart gives us a rundown of the worst offenders, and what to use instead:
Hot mess
The very worst offender is non-stick cookware, the kind with materials such as Teflon. These are the most toxic, due to PFAS chemicals.
Non-stick pans release toxic gases, leach chemicals into food, and release microplastic particles, which can accumulate in the body.
One that a lot of people don’t think about, in that category, is the humble air-fryer, which often as not has a non-stick cooking “basket”. These she describes as highly toxic, as they combine plastic, non-stick coatings, and high heat, which can release fumes and other potentially dangerous chemicals into the air and food.
You may be wondering: how bad is it? And the answer is, quite bad. PFAS chemicals are linked to infertility, hypertension in pregnancy, developmental issues in children, cancer, weakened immune systems, hormonal disruption, obesity, and intestinal inflammation.
Dr. Burkart’s top picks for doing better:
- Pure ceramic cookware: top choice for safety, particularly brands like Xtrema, which are tested for heavy metal leaching.
- Carbon steel & cast iron: durable and safe; can leach iron in acidic foods (for most people, this is a plus, but some may need to be aware of it)
- Stainless steel: lightweight and affordable but can leach nickel and chromium in acidic foods at high temperatures. Use only if nothing better is available.
And specifically as alternatives to air-fryers: glass convection ovens or stainless steel ovens are safer than conventional air fryers. The old “combination oven” can often be a good choice here.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- PFAS Exposure & Cancer: The Numbers Are High
- It’s Not Fantastic To Be Plastic ← for the closely related topic of microplastics and nanoplastics
Take care!
Share This Post
-
Hardwiring Happiness – by Dr. Rick Hanson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Publishers are very excitable about “the new science of…”, and it’s almost never actually a new science of. But what about in this case?
No, it isn’t. It’s the very well established science of! And that’s a good thing, because it means this book is able to draw on quite a lot of research and established understanding of how neuroplasticity works, to leverage that and provide useful guidance.
A particular strength of this book is that while it polarizes the idea that some people have “happy amygdalae” and some people have “sad amygdalae”, it acknowledges that it’s not just a fated disposition and is rather the result of the lives people have led… And then provides advice on upgrading from sad to happy, based on the assumption that the reader is quite possibly coming from a non-ideal starting point.
The bookdoes an excellent job of straddling neuroscience and psychology, which sounds like not much of a straddle (the two are surely very connected, after all, right?) but this does mean that we’re hearing about the chemical structure of DNA inside the nuclei of the neurons of the insula, not long after reading an extended gardening metaphor about growth, choices, and vulnerabilities.
Bottom line: if you’d like a guide to changing your brain for the better (happier) that’s not just “ask yourself: what if it goes well?” and similar CBTisms, then this is a fine book for you.
Click here to check out Hardwiring Happiness, and indeed hardwire happiness!
Share This Post
-
Older adults need another COVID-19 vaccine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What you need to know
- The CDC recommends people 65 and older and immunocompromised people receive an additional dose of the updated COVID-19 vaccine this spring—if at least four months have passed since they received a COVID-19 vaccine.
- Updated COVID-19 vaccines are effective at protecting against severe illness, hospitalization, death, and long COVID.
- The CDC also shortened the isolation period for people who are sick with COVID-19.
Last week, the CDC said people 65 and older should receive an additional dose of the updated COVID-19 vaccine this spring. The recommendation also applies to immunocompromised people, who were already eligible for an additional dose.
Older adults made up two-thirds of COVID-19-related hospitalizations between October 2023 and January 2024, so enhancing protection for this group is critical.
The CDC also shortened the isolation period for people who are sick with COVID-19, although the contagiousness of COVID-19 has not changed.
Read on to learn more about the CDC’s updated vaccination and isolation recommendations.
Who is eligible for another COVID-19 vaccine this spring?
The CDC recommends that people ages 65 and older and immunocompromised people receive an additional dose of the updated COVID-19 vaccine this spring—if at least four months have passed since they received a COVID-19 vaccine. It’s safe to receive an updated COVID-19 vaccine from Pfizer, Moderna, or Novavax, regardless of which COVID-19 vaccines you received in the past.
Updated COVID-19 vaccines are available at pharmacies, local clinics, or doctor’s offices. Visit Vaccines.gov to find an appointment near you.
Under- and uninsured adults can get the updated COVID-19 vaccine for free through the CDC’s Bridge Access Program. If you’re over 60 and unable to leave your home, call the Aging Network at 1-800-677-1116 to learn about free at-home vaccination options.
What are the benefits of staying up to date on COVID-19 vaccines?
Staying up to date on COVID-19 vaccines prevents severe illness, hospitalization, death, and long COVID.
Additionally, the CDC says staying up to date on COVID-19 vaccines is a safer and more reliable way to build protection against COVID-19 than getting sick from COVID-19.
What are the new COVID-19 isolation guidelines?
According to the CDC’s general respiratory virus guidance, people who are sick with COVID-19 or another common respiratory illness, like the flu or RSV, should isolate until they’ve been fever-free for at least 24 hours without the use of fever-reducing medication and their symptoms improve.
After that, the CDC recommends taking additional precautions for the next five days: wearing a well-fitting mask, limiting close contact with others, and improving ventilation in your home if you live with others.
If you’re sick with COVID-19, you can infect others for five to 12 days, or longer. Moderately or severely immunocompromised patients may remain infectious beyond 20 days.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
Metformin For Weight-Loss & More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Metformin Without Diabetes?
Metformin is a diabetes drug; it works by:
- decreasing glucose absorption from the gut
- decreasing glucose production in the liver
- increasing glucose sensitivity
It doesn’t change how much insulin is secreted, and is unlikely to cause hypoglycemia, making it relatively safe as diabetes drugs go.
It’s a biguanide drug, and/but so far as science knows (so far), its mechanism of action is unique (i.e. no other drug works the same way that metformin does).
Today we’ll examine its off-label uses and see what the science says!
A note on terms: “off-label” = when a drug is prescribed to treat something other than the main purpose(s) for which the drug was approved.
Other examples include modafinil against depression, and beta-blockers against anxiety.
Why take it if not diabetic?
There are many reasons people take it, including just general health and life extension:
However, its use was originally expanded (still “off-label”, but widely prescribed) past “just for diabetes” when it showed efficacy in treating pre-diabetes. Here for example is a longitudinal study that found metformin use performed similarly to lifestyle interventions (e.g. diet, exercise, etc). In their words:
❝ Lifestyle intervention or metformin significantly reduced diabetes development over 15 years. There were no overall differences in the aggregate microvascular outcome between treatment groups❞
But, it seems it does more, as this more recent review found:
❝Long-term weight loss was also seen in both [metformin and intensive lifestyle intervention] groups, with better maintenance under metformin.
Subgroup analyses from the DPP/DPPOS have shed important light on the actions of metformin, including a greater effect in women with prior gestational diabetes, and a reduction in coronary artery calcium in men that might suggest a cardioprotective effect.
Long-term diabetes prevention with metformin is feasible and is supported in influential guidelines for selected groups of subjects.❞
Source: Metformin for diabetes prevention: update of the evidence base
We were wondering about that cardioprotective effect, so…
Cardioprotective effect
In short, another review (published a few months after the above one) confirmed the previous findings, and also added:
❝Patients with BMI > 35 showed an association between metformin use and lower incidence of CVD, including African Americans older than age 65. The data suggest that morbidly obese patients with prediabetes may benefit from the use of metformin as recommended by the ADA.❞
We wondered about the weight loss implications of this, and…
For weight loss
The short version is, it works:
- Effectiveness of metformin on weight loss in non-diabetic individuals with obesity
- Metformin for weight reduction in non-diabetic patients: a systematic review and meta-analysis
- Metformin induces weight loss associated with gut microbiota alteration in non-diabetic obese women
…and many many more where those came from. As a point of interest, it has also been compared and contrasted to GLP-1 agonists.
Compared/contrasted with GLP-1 agonists
It’s not quite as effective for weight loss, and/but it’s a lot cheaper, is tablets rather than injections, has fewer side effects (for most people), and doesn’t result in dramatic yoyo-ing if there’s an interruption to taking it:
Or if you prefer a reader-friendly pop-science version:
Ozempic vs Metformin: Comparing The Two Diabetes Medications
Is it safe?
For most people yes, but there are a stack of contraindications, so it’s best to speak with your doctor. However, particular things to be aware of include:
- Usually contraindicated if you have kidney problems of any kind
- Usually contraindicated if you have liver problems of any kind
- May be contraindicated if you have issues with B12 levels
See also: Metformin: Is it a drug for all reasons and diseases?
Where can I get it?
As it’s a prescription-controlled drug, we can’t give you a handy Amazon link for this one.
However, many physicians are willing to prescribe it for off-label use (i.e., for reasons other than diabetes), so speak with yours (telehealth options may also be available).
If you do plan to speak with your doctor and you’re not sure they’ll be agreeable, you might want to get this paper and print it to take it with you:
Off-label indications of Metformin – Review of Literature
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Cold Truth About Respiratory Infections
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Pathogens That Came In From The Cold
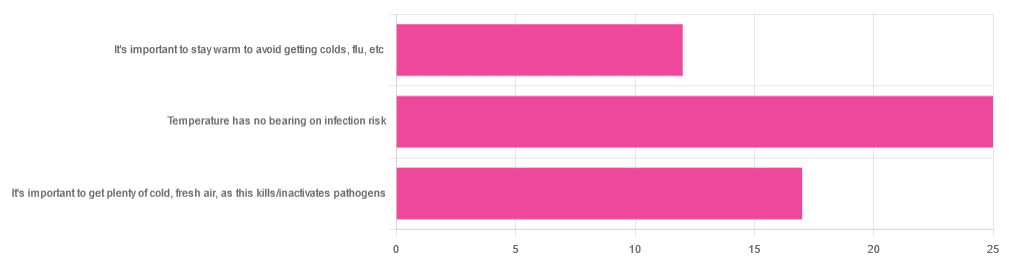
Yesterday, we asked you about your climate-themed policy for avoiding respiratory infections, and got the above-depicted, below-described, set of answers:
- About 46% of respondents said “Temperature has no bearing on infection risk”
- About 31% of respondents said “It’s important to get plenty of cold, fresh air, as this kills/inactivates pathogens”
- About 22% of respondents said “It’s important to stay warm to avoid getting colds, flu, etc”
Some gave rationales, including…
For “stay warm”:
❝Childhood lessons❞
For “get cold, fresh air”:
❝I just feel that it’s healthy to get fresh air daily. Whether it kills germs, I don’t know❞
For “temperature has no bearing”:
❝If climate issue affected respiratory infections, would people in the tropics suffer more than those in colder climates? Pollutants may affect respiratory infections, but I doubt just temperature would do so.❞
So, what does the science say?
It’s important to stay warm to avoid getting colds, flu, etc: True or False?
False, simply. Cold weather does increase the infection risk, but for reasons that a hat and scarf won’t protect you from. More on this later, but for now, let’s lay to rest the idea that bodily chilling will promote infection by cold, flu, etc.
In a small-ish but statistically significant study (n=180), it was found that…
❝There was no evidence that chilling caused any acute change in symptom scores❞
Read more: Acute cooling of the feet and the onset of common cold symptoms
Note: they do mention in their conclusion that chilling the feet “causes the onset of cold symptoms in about 10% of subjects who are chilled”, but the data does not support that conclusion, and the only clear indicator is that people who are more prone to colds generally, were more prone to getting a cold after a cold water footbath.
In other words, people who were more prone to colds remained more prone to colds, just the same.
It’s important to get plenty of cold, fresh air, as this kills/inactivates pathogens: True or False?
Broadly False, though most pathogens do have an optimal operating temperature that (for obvious reasons) is around normal human body temperature.
However, given that they don’t generally have to survive outside of a host body for long to get passed on, the fact that the pathogens may be a little sluggish in the great outdoors will not change the fact that they will be delighted by the climate in your respiratory tract as soon as you get back into the warm.
With regard to the cold air not being a reliable killer/inactivator of pathogens, we call to the witness stand…
Polar Bear Dies From Bird Flu As H5N1 Spreads Across Globe
(it was found near Utqiagvik, one of the northernmost communities in Alaska)
Because pathogens like human body temperature, raising the body temperature is a way to kill/inactivate them: True or False?
True! Unfortunately, it’s also a way to kill us. Because we, too, cannot survive for long above our normal body temperature.
So, for example, bundling up warmly and cranking up the heating won’t necessarily help, because:
- if the temperature is comfortable for you, it’s comfortable for the pathogen
- if the temperature is dangerous to the pathogen, it’s dangerous to you too
This is why the fever response evolved, and/but why many people with fevers die anyway. It’s the body’s way of playing chicken with the pathogen, challenging “guess which of us can survive this for longer!”
Temperature has no bearing on infection risk: True or False?
True and/or False, circumstantially. This one’s a little complex, but let’s break it down to the essentials.
- Temperature has no direct effect, for the reasons we outlined above
- Temperature is often related to humidity, which does have an effect
- Temperature does tend to influence human behavior (more time spent in open spaces with good ventilation vs more time spent in closed quarters with poor ventilation and/or recycled air), which has an obvious effect on transmission rates
The first one we covered, and the third one is self-evident, so let’s look at the second one:
Temperature is often related to humidity, which does have an effect
When the environmental temperature is warmer, water droplets in the air will tend to be bigger, and thus drop to the ground much more quickly.
When the environmental temperature is colder, water droplets in the air will tend to be smaller, and thus stay in the air for longer (along with any pathogens those water droplets may be carrying).
Some papers on the impact of this:
- Cold temperature and low humidity are associated with increased occurrence of respiratory tract infections
- A Decrease in Temperature and Humidity Precedes Human Rhinovirus Infections in a Cold Climate
So whatever temperature you like to keep your environment, humidity is a protective factor against respiratory infections, and dry air is a risk factor.
So, for example:
- If the weather doesn’t suit having good ventilation, a humidifier is a good option
- Being in an airplane is one of the worst places to be for this, outside of a hospital
Don’t have a humidifier? Here’s an example product on Amazon, but by all means shop around.
A crock pot with hot water in and the lid off is also a very workable workaround too
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
An Elegant Defense – by Matt Richtel
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In a way, Richtel got the best and worst of the publication date lottery. This book, which he’d obviously been working on for however long, was published in March 2020. Yes, that March 2020. So, it obviously got a huge boost in sales that launced it to bestseller status, and/but it doesn’t actually discuss COVID at all.
What it does discuss, is—as one might expect—the immune system. Or really, the immune systems, plural, several systems working alongside each other. How we got to have such, how our immune functions work, where all the various immune cells come from and what part they play. What pathogens can do to fight and/or confuse (or even co-opt) our immune response, and what modern medicine can do to counteract the pathogens’ anti-countermeasure countermeasures. And how it can still go wrong.
The “Four Lives” promised in the subtitle are stories, and Richtel explains the immune system through specific people’s specific battles. In particular, a friend of his who had quite a remarkable battle against cancer, which was of course terrible for him, but illustrative for us.
The style of the book is very readably journalistic. The author is a Pulitzer-winning NYT journalist, and not normally a science writer. Here at 10almonds, “we like big bibliographies and we cannot lie”, and we didn’t get to enjoy that in this case. The book contained no bibliography (nor appropriate inline citations, nor equivalent footnotes). Maybe a future addition will include this.
Bottom line: there’s a lot of “science for the lay reader” here. While the lack of references is a big oversight, the book does give a very good overview of what both sides (immune response and pathogenic invasion) bring to the battle of your body.
Click here to check out Elegant Defense, and demystify immunology!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: