To tackle gendered violence, we also need to look at drugs, trauma and mental health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
After several highly publicised alleged murders of women in Australia, the Albanese government this week pledged more than A$925 million over five years to address men’s violence towards women. This includes up to $5,000 to support those escaping violent relationships.
However, to reduce and prevent gender-based and intimate partner violence we also need to address the root causes and contributors. These include alcohol and other drugs, trauma and mental health issues.
Why is this crucial?
The World Health Organization estimates 30% of women globally have experienced intimate partner violence, gender-based violence or both. In Australia, 27% of women have experienced intimate partner violence by a co-habiting partner; almost 40% of Australian children are exposed to domestic violence.
By gender-based violence we mean violence or intentionally harmful behaviour directed at someone due to their gender. But intimate partner violence specifically refers to violence and abuse occurring between current (or former) romantic partners. Domestic violence can extend beyond intimate partners, to include other family members.
These statistics highlight the urgent need to address not just the aftermath of such violence, but also its roots, including the experiences and behaviours of perpetrators.
What’s the link with mental health, trauma and drugs?
The relationships between mental illness, drug use, traumatic experiences and violence are complex.
When we look specifically at the link between mental illness and violence, most people with mental illness will not become violent. But there is evidence people with serious mental illness can be more likely to become violent.
The use of alcohol and other drugs also increases the risk of domestic violence, including intimate partner violence.
About one in three intimate partner violence incidents involve alcohol. These are more likely to result in physical injury and hospitalisation. The risk of perpetrating violence is even higher for people with mental ill health who are also using alcohol or other drugs.
It’s also important to consider traumatic experiences. Most people who experience trauma do not commit violent acts, but there are high rates of trauma among people who become violent.
For example, experiences of childhood trauma (such as witnessing physical abuse) can increase the risk of perpetrating domestic violence as an adult.

Early traumatic experiences can affect the brain and body’s stress response, leading to heightened fear and perception of threat, and difficulty regulating emotions. This can result in aggressive responses when faced with conflict or stress.
This response to stress increases the risk of alcohol and drug problems, developing PTSD (post-traumatic stress disorder), and increases the risk of perpetrating intimate partner violence.
How can we address these overlapping issues?
We can reduce intimate partner violence by addressing these overlapping issues and tackling the root causes and contributors.
The early intervention and treatment of mental illness, trauma (including PTSD), and alcohol and other drug use, could help reduce violence. So extra investment for these are needed. We also need more investment to prevent mental health issues, and preventing alcohol and drug use disorders from developing in the first place.

Preventing trauma from occuring and supporting those exposed is crucial to end what can often become a vicious cycle of intergenerational trauma and violence. Safe and supportive environments and relationships can protect children against mental health problems or further violence as they grow up and engage in their own intimate relationships.
We also need to acknowledge the widespread impact of trauma and its effects on mental health, drug use and violence. This needs to be integrated into policies and practices to reduce re-traumatising individuals.
How about programs for perpetrators?
Most existing standard intervention programs for perpetrators do not consider the links between trauma, mental health and perpetrating intimate partner violence. Such programs tend to have little or mixed effects on the behaviour of perpetrators.
But we could improve these programs with a coordinated approach including treating mental illness, drug use and trauma at the same time.
Such “multicomponent” programs show promise in meaningfully reducing violent behaviour. However, we need more rigorous and large-scale evaluations of how well they work.
What needs to happen next?
Supporting victim-survivors and improving interventions for perpetrators are both needed. However, intervening once violence has occurred is arguably too late.
We need to direct our efforts towards broader, holistic approaches to prevent and reduce intimate partner violence, including addressing the underlying contributors to violence we’ve outlined.
We also need to look more widely at preventing intimate partner violence and gendered violence.
We need developmentally appropriate education and skills-based programs for adolescents to prevent the emergence of unhealthy relationship patterns before they become established.
We also need to address the social determinants of health that contribute to violence. This includes improving access to affordable housing, employment opportunities and accessible health-care support and treatment options.
All these will be critical if we are to break the cycle of intimate partner violence and improve outcomes for victim-survivors.
The National Sexual Assault, Family and Domestic Violence Counselling Line – 1800 RESPECT (1800 737 732) – is available 24 hours a day, seven days a week for any Australian who has experienced, or is at risk of, family and domestic violence and/or sexual assault.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14. In an emergency, call 000.
Siobhan O’Dean, Postdoctoral Research Associate, The Matilda Centre for Research in Mental Health and Substance Use, University of Sydney; Lucinda Grummitt, Postdoctoral Research Fellow, The Matilda Centre for Research in Mental Health and Substance Use, University of Sydney, and Steph Kershaw, Research Fellow, The Matilda Centre for Research in Mental Health and Substance Use, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Growing Young – by Marta Zaraska
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This one will be a slightly mixed review, but we think the book has more than enough of value to make it a very worthwhile read.
The premise of the book is that, as the subtitle suggests, positive social qualities increase personal longevity.
Author (and science journalist) Marta Zaraska looks at a lot of research to back this up, and also did a lot of travelling and digging into stories. This is of great value, because she notes where a lot of misconceptions have arisen.
To give one example, it’s commonly noted that marriage (or as-though-marriage life partnerships) is generally* associated with longer life.
*Statistics suggest that marriage-related longevity is enjoyed by men married to women, and people in same-sex marriages regardless of gender, but is not so much the case for women married to men.
However! Zaraska notes a factor she learned from Gottman’s research (yes, that Gottman), that what matters is not the official status of a relationship, so much as the sense of secure lifelong commitment to it.
These kinds of observations (throughout the book) add an extra layer beyond “common wisdom”, and allow us to better understand what’s really going on. The book’s main weaknesses, meanwhile, are twofold:
- The author is (in this reviewer’s opinion) unduly dismissive of physical health lifestyle factors such as diet and exercise, because they “only” account for a similar bonus to healthy longevity.
- Like many, she does not always consider where correlation might not mean causation. For example, she cites that volunteering free time increases healthspan by 22%, but neglects to note that perhaps it is having the kind of socioeconomic situation that allows one free time to volunteer, that gives the benefit.
Bottom line: the book has its flaws, but we think that only serves to make it more engaging. After all, reading should not be a purely passive activity! Zaraska’s well-studied insights give plenty of pointers for tweaking the social side of anyone’s quest for healthy longevity.
Click here to check out Growing Young, increase your healthspan, and take joy in doing it!
Share This Post
-
For Many Rural Women, Finding Maternity Care Outweighs Concerns About Abortion Access
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
BAKER CITY, Ore. — In what has become a routine event in rural America, a hospital maternity ward closed in 2023 in this small Oregon town about an hour from the Idaho border.
For Shyanne McCoy, 23, that meant the closest hospital with an obstetrician on staff when she was pregnant was a 45-mile drive away over a mountain pass.
When McCoy developed symptoms of preeclampsia last January, she felt she had the best chance of getting the care she needed at a larger hospital in Boise, Idaho, two hours away. She spent the final week of her pregnancy there, too far from home to risk leaving, before giving birth to her daughter.
Six months later, she said it seems clear to her that the health care needs of rural young women like her are largely ignored.
For McCoy and others, figuring out how to obtain adequate care to safely have a baby in Baker City has quickly eclipsed concerns about another medical service lacking in the area: abortion. But in Oregon and elsewhere in the country, progressive lawmakers’ attempts to expand abortion access sometimes clash with rural constituencies.
Oregon is considered one of the most protective states in the country when it comes to abortion. There are no legal limits on when someone can receive an abortion in the state, and the service is covered by its Medicaid system. Still, efforts to expand access in the rural, largely conservative areas that cover most of the state have encountered resistance and incredulity.
It’s a divide that has played out in elections in such states as Nevada, where voters passed a ballot measure in November that seeks to codify abortion protections in the state constitution. Residents in several rural counties opposed the measure.
In Oregon, during the months just before the Baker City closure was announced, Democratic state lawmakers were focused on a proposed pilot program that would launch two mobile reproductive health care clinics in rural areas. The bill specified that the van-based clinics would include abortion services.
State Rep. Christine Goodwin, a Republican from a southwestern Oregon district, called the proposal the “latest example” of urban legislators telling rural leaders what their communities need.
The mobile health clinic pilot was eventually removed from the bill that was under discussion. That means no new abortion options in Oregon’s Baker County — and no new state-funded maternity care either.
“I think if you expanded rural access in this community to abortions before you extended access to maternal health care, you would have an uprising on your hands,” said Paige Witham, 27, a member of the Baker County health care steering committee and the mother of two children, including an infant born in October.
A study published in JAMA in early December that examined nearly 5,000 acute care hospitals found that by 2022, 52% of rural hospitals lacked obstetrics care after more than a decade of unit closures. The health implications of those closures for young women, the population most likely to need pregnancy care, and their babies can be significant. Research has shown that added distance between a patient and obstetric care increases the likelihood the baby will be admitted to a neonatal intensive care unit, or NICU.
Witham said that while she does not support abortion, she believes the government should not “legislate it away completely.” She said that unless the government provides far more support for young families, like free child care and better mental health care, abortion should remain legal.
Conversations with a liberal school board member, a moderate owner of a timber company, members of Baker City’s Republican Party chapter, a local doula, several pregnant women, and the director of the Baker County Health Department — many of whom were not rigidly opposed to abortion — all turned up the same answer: No mobile clinics offering abortions here, please.
Kelle Osborn, a nurse supervisor for the Baker County Health Department, loved the idea of a mobile clinic that would provide education and birth control services to people in outlying areas. She was less thrilled about including abortion services in a clinic on wheels.
“It’s not something that should just be handed out from a mobile van,” she said of abortion services. She said people in her conservative rural county would probably avoid using the clinics for anything if they were understood to provide abortion services.
Both Osborn and Meghan Chancey, the health department’s director, said they would rank many health care priorities higher, including the need for a general surgeon, an ICU, and a dialysis clinic.
Nationally, reproductive health care services of all types tend to be limited for people in rural areas, even within states that protect abortion access. More than two-thirds of people in “maternity care deserts” — all of which are in rural counties — must drive more than a half-hour to get obstetric care, according to a 2024 March of Dimes report. For people in the Southern states where lawmakers installed abortion bans, abortion care can be up to 700 miles away, according to a data analysis by Axios.
Nathan Defrees grew up in Baker City and has practiced medicine here since 2017. He works for a family medicine clinic. If a patient asks about abortion, he provides information about where and how one can be obtained, but he doesn’t offer abortions himself.
“There’s not a lot of anonymity in small towns for physicians who provide that care,” he said. “Many of us aren’t willing to sacrifice the rest of our career for that.”
He also pointed to the small number of patients requesting the service locally. Just six people living in Baker County had an abortion in 2023, according to data from the Oregon Department of Public Health. Meanwhile, 125 residents had a baby that year.
A doctor with obstetric training living in another rural part of the state has chosen to quietly provide early-stage abortions when asked. The doctor, concerned for their family’s safety in the small, conservative town where they live, asked not to be identified.
The idea that better access to abortion is not needed in rural areas seems naive, the doctor said. People most in need of abortion often don’t have access to any medical service not already available in town, the doctor pointed out. The first patient the doctor provided an abortion for at the clinic was a meth user with no resources to travel or to manage an at-home medication abortion.
“It seemed entirely inappropriate for me to turn her away for care I had the training and the tools to do,” the doctor said.
Defrees said it has been easier for Baker County residents to get an abortion since the U.S. Supreme Court overturned Roe v. Wade.
A new Planned Parenthood clinic in Ontario, Oregon, 70 miles away in neighboring Malheur County, was built primarily to provide services to people from the Boise metro area, but it also created an option for many living in rural eastern Oregon.
Idaho is one of the 16 states with near-total bans on abortion. Like many states with bans, Idaho has struggled to maintain its already small fleet of fetal medicine doctors. The loss of regional expertise touches Baker City, too, Defrees said.
For example, he said, the treatment plan for women who have a desired pregnancy but need a termination for medical reasons is now far less clear. “It used to be those folks could go to Boise,” he said. “Now they can’t. That does put us in a bind.”
Portland is the next closest option for that type of care, and that means a 300-mile drive along a set of highways that can be treacherous in winter.
“It’s a lot scarier to be pregnant now in Baker City than it ever has been,” Defrees said.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
-
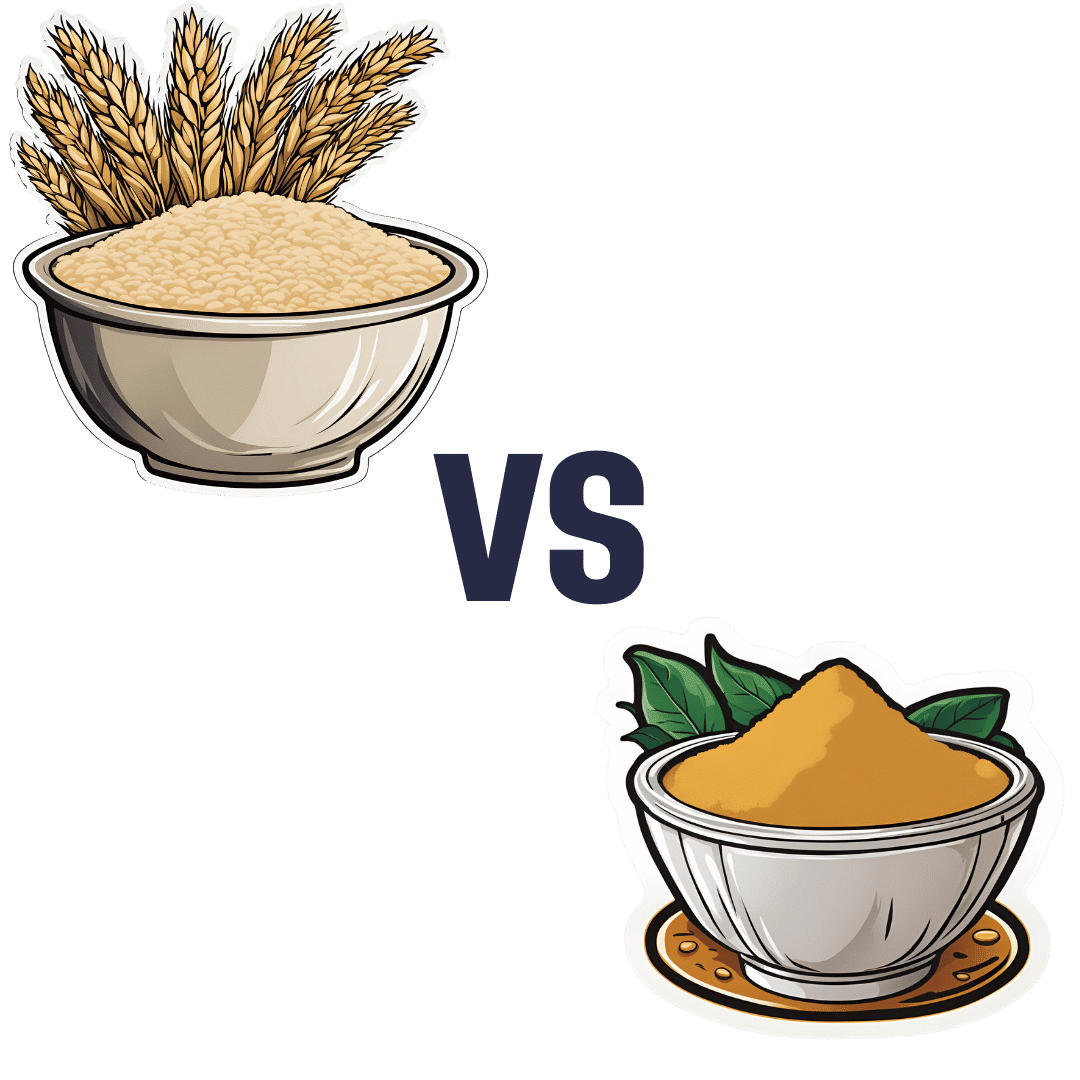
Barley Malt Flour vs chickpea flour – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing barley malt flour to chickpea flour, we picked the chickpea.
Why?
First, some notes:
About chickpea flour: this is also called besan flour, gram flour, and garbanzo bean flour; they are all literally the same thing by different names, and are all flour made from ground chickpeas.
About barley malt flour: barley is a true grain, and does contain gluten. We’re not going to factor that into today’s decision, but if you are avoiding gluten, avoid barley. As for “malt”; malting grains means putting them in an environment (with appropriate temperature and humidity) that they can begin germination, and then drying them with hot air to stop the germination process from continuing, so that we still have grains to make flour out of, and not little green sprouting plants. It improves the nutritional qualities and, subjectively, the flavor.
To avoid repetition, we’re just going to write “barley” instead of “barley malt” now, but it’s still malted.
Now, let’s begin:
Looking at the macros first, chickpea flour has 2x the protein and also more fiber, while barley flour has more carbs. An easy win for chickpea flour.
In the category of vitamins, chickpea flour has more of vitamins A, B1, B5, B9, E, and K, while barley flour has more of vitamins B2, B3, B6, and C. A modest 6:4 victory for chickpea flour.
When it comes to minerals, things are much more one-sided; chickpea flour has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and zinc, while barley flour has more selenium. An overwhelming win for chickpea flour.
Adding up these three wins for chickpea flour makes for a convincing story in favor of using that where reasonably possible as a flour! It has a slight nutty taste, so you might not want to use it in everything, but it is good for a lot of things.
Want to learn more?
You might like to read:
- Grains: Bread Of Life, Or Cereal Killer?
- Gluten: What’s The Truth?
- Sprout Your Seeds, Grains, Beans, Etc
Take care!
Share This Post
Related Posts
-
Yoga Therapy for Arthritis – by Dr. Steffany Moonaz & Erin Byron
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Two quick notes to start with:
- One of the problems with arthritis and exercise is that arthritis can often impede exercise.
- Another of the problems with arthritis and exercise is that some kinds of exercise can exacerbate arthritis.
This book deals with both of those issues, by providing yoga specifically tailored to living with arthritis. Indeed, the first-listed author’s PhD in public health was the result of 8 years of study developing an evidence-based yoga program for people with arthritis, including osteoarthritis and rheumatoid arthritis.
The authors take the view that arthritis is a whole-person disease (i.e. it affects all parts of you), and so addressing it requires a whole-person approach, which is what this book delivers.
As such, this is not just a book of asana (yoga postures). It does provide that, of course (as well as breathing exercises), but also its 328 pages additionally cover a lot of conscious work from the inside out, including attention to the brain, energy levels, pain, and so forth, and that the practice of yoga should not merely directly improve the joints via gentle physical exercise, but also should help to heal the whole person, including reducing stress levels, reducing physical tension, and with those two things, reducing inflammation also—and also, due to both that and the asana side of practice, better-functioning organs, which is always a bonus.
The style is interesting, as it refers to both science (8 pages of hard-science bibliography) and yogic principles (enough esoterica to put off, say, James Randi or Penn & Teller). This reviewer is very comfortable with both, and so if you, dear reader, are comfortable with both too, then you will surely enjoy this book.
Bottom line: if you or a loved one has arthritis, you’ll wish you got this book sooner.
Click here to check out Yoga Therapy For Arthritis, and live better!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
15 Easy Japanese Habits That Will Transform Your Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The original title says “no-cost habits”, but in fairness, for most of us food is not usually free (alas). So, we will say “easy” instead, because they are indeed easy to build into your life:
15 Healthy Habits To Adopt
We’ll not keep them a mystery; they are:
- Intermittent fasting: naturally fasting for at least 12 hours overnight improves digestion and sleep quality.
- Fermented foods: regularly consuming fermented foods (like kimchi, or even just sauces like miso and shio koji) supports gut health.
- Rice & legumes over wheat: choosing wholegrain rice as a staple reduces bloating and benefits skin health (lentils are even better).
- Big breakfast, light dinner: eating a heavier breakfast and a lighter dinner gives energy in the morning and allows digestion to rest at night.
- Balancing indulgences: enjoying social meals without guilt and balancing food intake the next day.
- Daily gentle exercise: doing at least 15 minutes of yoga, Pilates, or light walking for long-term health.
- Daily baths: taking a warm bath boosts blood circulation and relaxation.
- Eating seasonal & diverse foods: including a variety of fresh, seasonal ingredients for balanced nutrition.
- Consistent morning routine: waking up at the same time, cleansing and moisturizing, and having a proper breakfast.
- Enjoying soup with meals: consuming nutrient-rich soups with vegetables and protein to prevent overeating.
- Chewing food thoroughly: eating slowly and chewing well aids digestion and enhances enjoyment.
- Light seasoning in food: avoiding overly salty or flavorful meals to appreciate natural tastes.
- Maintaining good posture: paying attention to posture during daily activities for better overall health.
- Prioritizing protein intake: eating protein-rich foods like tofu, beans, eggs, and fish, to maintain skin firmness as well as muscletone.
- Confidence in aging: focusing on internal well-being over external opinions and embracing health at every age.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The #1 Foot Health Secret Everyone Over 50 Should Know
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our favorite over-50s specialist physio Will Harlow is here to keep us on our toes:
Mobility requires mobilization
As we age, our toes are inclined to become stiffer. Stiff toes lead to balance issues and increased risk of falling.
A study cited in the video showed that two weeks of toe mobilization improved foot-ground contact by 30% in older adults, enhancing balance and reducing falls.
Here’s the routine:
- Toe flexion:
- Apply moisturizer or oil to your hands.
- Pull your toes downwards, then let them return their normal position.
- Repeat for one minute per foot.
- Toe extension:
- Rub hands from the heel under the toes.
- Push your toes upwards, then let them return to their normal position.
- Repeat for one minute per foot.
- Foot rotation:
- Hold both sides of your foot and twist it in one direction, then the other.
- This helps loosen foot joints and improve flexibility.
- Perform for one minute in each direction per foot.
For more on each of these plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Steps For Keeping Your Feet A Healthy Foundation
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Toe flexion: