The Teenage Brain – by Dr. Frances Jensen
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We realize that we probably have more grandparents of teenagers than parents of teenagers here, but most of us have at least some teenage relative(s). Which makes this book interesting.
There are a lot of myths about the teenage brain, and a lot of popular assumptions that usually have some basis in fact but are often misleading.
Dr. Jensen gives us a strong foundational grounding in the neurophysiology of adolescence, from the obvious-but-often-unclear (such as the role of hormones) to less-known things like the teenage brain’s general lack of myelination. Not just “heightened neuroplasticity” but, if you imagine the brain as an electrical machine, then think of myelin as the insulation between the wires. Little wonder some wires may get crossed sometimes!
She also talks about such things as the teenage circadian rhythm’s innate differences, the impact of success and failure on the brain, and harder topics such as addiction—and the adolescent cortisol functions that can lead to teenagers needing to seek something to relax in the first place.
In criticism, we can only say that sometimes the author makes sweeping generalizations without acknowledging such, but that doesn’t detract from what she has to say on the topic of neurophysiology.
Bottom line: if there’s a teenager in your life whose behavior and/or moods are sometimes baffling to you, and whose mysteries you’d like to unravel, this is a great book.
Click here to check out the Teenage Brain, and better understand those around you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Could not getting enough sleep increase your risk of type 2 diabetes?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Not getting enough sleep is a common affliction in the modern age. If you don’t always get as many hours of shut-eye as you’d like, perhaps you were concerned by news of a recent study that found people who sleep less than six hours a night are at higher risk of type 2 diabetes.
So what can we make of these findings? It turns out the relationship between sleep and diabetes is complex.
The study
Researchers analysed data from the UK Biobank, a large biomedical database which serves as a global resource for health and medical research. They looked at information from 247,867 adults, following their health outcomes for more than a decade.
The researchers wanted to understand the associations between sleep duration and type 2 diabetes, and whether a healthy diet reduced the effects of short sleep on diabetes risk.
As part of their involvement in the UK Biobank, participants had been asked roughly how much sleep they get in 24 hours. Seven to eight hours was the average and considered normal sleep. Short sleep duration was broken up into three categories: mild (six hours), moderate (five hours) and extreme (three to four hours). The researchers analysed sleep data alongside information about people’s diets.
Some 3.2% of participants were diagnosed with type 2 diabetes during the follow-up period. Although healthy eating habits were associated with a lower overall risk of diabetes, when people ate healthily but slept less than six hours a day, their risk of type 2 diabetes increased compared to people in the normal sleep category.
The researchers found sleep duration of five hours was linked with a 16% higher risk of developing type 2 diabetes, while the risk for people who slept three to four hours was 41% higher, compared to people who slept seven to eight hours.
One limitation is the study defined a healthy diet based on the number of servings of fruit, vegetables, red meat and fish a person consumed over a day or a week. In doing so, it didn’t consider how dietary patterns such as time-restricted eating or the Mediterranean diet may modify the risk of diabetes among those who slept less.
Also, information on participants’ sleep quantity and diet was only captured at recruitment and may have changed over the course of the study. The authors acknowledge these limitations.
Why might short sleep increase diabetes risk?
In people with type 2 diabetes, the body becomes resistant to the effects of a hormone called insulin, and slowly loses the capacity to produce enough of it in the pancreas. Insulin is important because it regulates glucose (sugar) in our blood that comes from the food we eat by helping move it to cells throughout the body.
We don’t know the precise reasons why people who sleep less may be at higher risk of type 2 diabetes. But previous research has shown sleep-deprived people often have increased inflammatory markers and free fatty acids in their blood, which impair insulin sensitivity, leading to insulin resistance. This means the body struggles to use insulin properly to regulate blood glucose levels, and therefore increases the risk of type 2 diabetes.
Further, people who don’t sleep enough, as well as people who sleep in irregular patterns (such as shift workers), experience disruptions to their body’s natural rhythm, known as the circadian rhythm.
This can interfere with the release of hormones like cortisol, glucagon and growth hormones. These hormones are released through the day to meet the body’s changing energy needs, and normally keep blood glucose levels nicely balanced. If they’re compromised, this may reduce the body’s ability to handle glucose as the day progresses.
These factors, and others, may contribute to the increased risk of type 2 diabetes seen among people sleeping less than six hours.
Millions of people around the world have diabetes. WESTOCK PRODUCTIONS/Shutterstock While this study primarily focused on people who sleep eight hours or less, it’s possible longer sleepers may also face an increased risk of type 2 diabetes.
Research has previously shown a U-shaped correlation between sleep duration and type 2 diabetes risk. A review of multiple studies found getting between seven to eight hours of sleep daily was associated with the lowest risk. When people got less than seven hours sleep, or more than eight hours, the risk began to increase.
The reason sleeping longer is associated with increased risk of type 2 diabetes may be linked to weight gain, which is also correlated with longer sleep. Likewise, people who don’t sleep enough are more likely to be overweight or obese.
Good sleep, healthy diet
Getting enough sleep is an important part of a healthy lifestyle and may reduce the risk of type 2 diabetes.
Based on this study and other evidence, it seems that when it comes to diabetes risk, seven to eight hours of sleep may be the sweet spot. However, other factors could influence the relationship between sleep duration and diabetes risk, such as individual differences in sleep quality and lifestyle.
While this study’s findings question whether a healthy diet can mitigate the effects of a lack of sleep on diabetes risk, a wide range of evidence points to the benefits of healthy eating for overall health.
The authors of the study acknowledge it’s not always possible to get enough sleep, and suggest doing high-intensity interval exercise during the day may offset some of the potential effects of short sleep on diabetes risk.
In fact, exercise at any intensity can improve blood glucose levels.
Giuliana Murfet, Casual Academic, Faculty of Health, University of Technology Sydney and ShanShan Lin, Senior Lecturer, School of Public Health, University of Technology Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Paris in spring, Bali in winter. How ‘bucket lists’ help cancer patients handle life and death
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In the 2007 film The Bucket List Jack Nicholson and Morgan Freeman play two main characters who respond to their terminal cancer diagnoses by rejecting experimental treatment. Instead, they go on a range of energetic, overseas escapades.
Since then, the term “bucket list” – a list of experiences or achievements to complete before you “kick the bucket” or die – has become common.
You can read articles listing the seven cities you must visit before you die or the 100 Australian bucket-list travel experiences. https://www.youtube.com/embed/UvdTpywTmQg?wmode=transparent&start=0
But there is a more serious side to the idea behind bucket lists. One of the key forms of suffering at the end of life is regret for things left unsaid or undone. So bucket lists can serve as a form of insurance against this potential regret.
The bucket-list search for adventure, memories and meaning takes on a life of its own with a diagnosis of life-limiting illness.
In a study published this week, we spoke to 54 people living with cancer, and 28 of their friends and family. For many, a key bucket list item was travel.
Why is travel so important?
There are lots of reasons why travel plays such a central role in our ideas about a “life well-lived”. Travel is often linked to important life transitions: the youthful gap year, the journey to self-discovery in the 2010 film Eat Pray Love, or the popular figure of the “grey nomad”.
The significance of travel is not merely in the destination, nor even in the journey. For many people, planning the travel is just as important. A cancer diagnosis affects people’s sense of control over their future, throwing into question their ability to write their own life story or plan their travel dreams.
Mark, the recently retired husband of a woman with cancer, told us about their stalled travel plans:
We’re just in that part of our lives where we were going to jump in the caravan and do the big trip and all this sort of thing, and now [our plans are] on blocks in the shed.
For others, a cancer diagnosis brought an urgent need to “tick things off” their bucket list. Asha, a woman living with breast cancer, told us she’d always been driven to “get things done” but the cancer diagnosis made this worse:
So, I had to do all the travel, I had to empty my bucket list now, which has kind of driven my partner round the bend.
People’s travel dreams ranged from whale watching in Queensland to seeing polar bears in the Arctic, and from driving a caravan across the Nullarbor Plain to skiing in Switzerland.
Whale watching in Queensland was on one person’s bucket list. Uwe Bergwitz/Shutterstock Nadia, who was 38 years old when we spoke to her, said travelling with her family had made important memories and given her a sense of vitality, despite her health struggles. She told us how being diagnosed with cancer had given her the chance to live her life at a younger age, rather than waiting for retirement:
In the last three years, I think I’ve lived more than a lot of 80-year-olds.
But travel is expensive
Of course, travel is expensive. It’s not by chance Nicholson’s character in The Bucket List is a billionaire.
Some people we spoke to had emptied their savings, assuming they would no longer need to provide for aged care or retirement. Others had used insurance payouts or charity to make their bucket-list dreams come true.
But not everyone can do this. Jim, a 60-year-old whose wife had been diagnosed with cancer, told us:
We’ve actually bought a new car and [been] talking about getting a new caravan […] But I’ve got to work. It’d be nice if there was a little money tree out the back but never mind.
Not everyone’s bucket list items were expensive. Some chose to spend more time with loved ones, take up a new hobby or get a pet.
Our study showed making plans to tick items off a list can give people a sense of self-determination and hope for the future. It was a way of exerting control in the face of an illness that can leave people feeling powerless. Asha said:
This disease is not going to control me. I am not going to sit still and do nothing. I want to go travel.
Something we ‘ought’ to do?
Bucket lists are also a symptom of a broader culture that emphasises conspicuous consumption and productivity, even into the end of life.
Indeed, people told us travelling could be exhausting, expensive and stressful, especially when they’re also living with the symptoms and side effects of treatment. Nevertheless, they felt travel was something they “ought” to do.
Travel can be deeply meaningful, as our study found. But a life well-lived need not be extravagant or adventurous. Finding what is meaningful is a deeply personal journey.
Names of study participants mentioned in this article are pseudonyms.
Leah Williams Veazey, ARC DECRA Research Fellow, University of Sydney; Alex Broom, Professor of Sociology & Director, Sydney Centre for Healthy Societies, University of Sydney, and Katherine Kenny, ARC DECRA Senior Research Fellow, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Alzheimer’s Sex Differences May Not Be What They Appear
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Alzheimer’s Sex Differences May Not Be What They Appear
Women get Alzheimer’s at nearly twice the rate than men do, and deteriorate more rapidly after onset, too.
So… Why?
There are many potential things to look at, but four stand out for quick analysis:
- Chromosomes: women usually have XX chromosomes, to men’s usual XY. There are outliers to both groups, people with non-standard combinations of chromosomes, but not commonly enough to throw out the stats.
- Hormones: women usually have high estrogen and low testosterone, compared to men. Again there are outliers and this is a huge oversimplification that doesn’t even look at other sex hormones, but broadly speaking (which sounds vague, but is actually what is represented in epidemiological studies), it will be so.
- Anatomy: humans have some obvious sexual dimorphism (again, there are outliers, but again, not enough to throw out the stats); this seems least likely to be relevant (Alzheimer’s is probably not stored in the breasts, for examples), though average body composition (per muscle:fat ratio) could admittedly be a factor.
- Social/lifestyle: once again, #NotAllWomen etc, but broadly speaking, women and men often tend towards different social roles in some ways, and as we know, of course lifestyle can play a part in disease pathogenesis.
As a quick aside before we continue, if you’re curious about those outliers, then a wiki-walk into the fascinating world of intersex conditions, for example, could start here. But by and large, this won’t affect most people.
So… Which parts matter?
Back in 2018, Dr. Maria Teresa Ferretti et al. kicked up some rocks in this regard, looking not just at genes (as much research has focussed on) or amyloid-β (again, well-studied) but also at phenotypes and metabolic and social factors—bearing in mind that all three of those are heavily influenced by hormones. Noting, for example, that (we’ll quote directly here):
- Men and women with Alzheimer disease (AD) exhibit different cognitive and psychiatric symptoms, and women show faster cognitive decline after diagnosis of mild cognitive impairment (MCI) or AD dementia.
- Brain atrophy rates and patterns differ along the AD continuum between the sexes; in MCI, brain atrophy is faster in women than in men.
- The prevalence and effects of cerebrovascular, metabolic and socio-economic risk factors for AD are different between men and women.
See: Sex differences in Alzheimer disease—the gateway to precision medicine
So, have scientists controlled for each of those factors?
Mostly not! But they have found clues, anyway, while noting the limitations of the previous way of conducting studies. For example:
❝Women are more likely to develop Alzheimer’s disease and experience faster cognitive decline compared to their male counterparts. These sex differences should be accounted for when designing medications and conducting clinical trials❞
~ Dr. Feixiong Cheng
Read: Research finds sex differences in immune response and metabolism drive Alzheimer’s disease
Did you spot the clue?
It was “differences in immune response and metabolism”. These things are both influenced by (not outright regulated by, but strongly influenced by) sex hormones.
❝As [hormonal] sex influences both the immune system and metabolic process, our study aimed to identify how all of these individual factors influence one another to contribute to Alzheimer’s disease❞
~ Dr. Justin Lathia
Ignoring for a moment progesterone’s role in metabolism, estrogen is an immunostimulant and testosterone is an immunosuppressant. These thus both also have an effect in inflammation, which yes, includes neuroinflammation.
But wait a minute, shouldn’t that mean that women are more protected, not less?
It should! Except… Alzheimer’s is an age-related disease, and in the age-bracket that generally gets Alzheimer’s (again, there are outliers), menopause has been done and dusted for quite a while.
Which means, and this is critical: post-menopausal women not on HRT are essentially left without the immune boost usually directed by estrogen, while men of the same age will be ticking over with their physiology that (unlike that of the aforementioned women) was already adapted to function with negligible estrogen.
Specifically:
❝The metabolic consequences of estrogen decline during menopause accelerate neuropathology in women❞
~ Dr. Rasha Saleh
Critical idea to take away from all this:
Alzheimer’s research is going to be misleading if it doesn’t take into account sex differences, and not just that, but also specifically age-relevant sex differences—because that can flip the narrative. If we don’t take age into account, we could be left thinking estrogen is to blame, when in fact, it appears to be the opposite.
In the meantime, if you’re a woman of a certain age, you might talk with a doctor about whether HRT could be beneficial for you, if you haven’t already:
❝Women at genetic risk for AD (carrying at least one APOE e4 allele) seem to be particularly benefiting from MHT❞
(MHT = Menopausal Hormone Therapy; also commonly called HRT, which is the umbrella term for Hormone Replacement Therapies in general)
~ Dr. Herman Depypere
Source study: Menopause hormone therapy significantly alters pathophysiological biomarkers of Alzheimer’s disease
Pop-sci press release version: HRT could ward off Alzheimer’s among at-risk women
Take care!
Share This Post
Related Posts
-
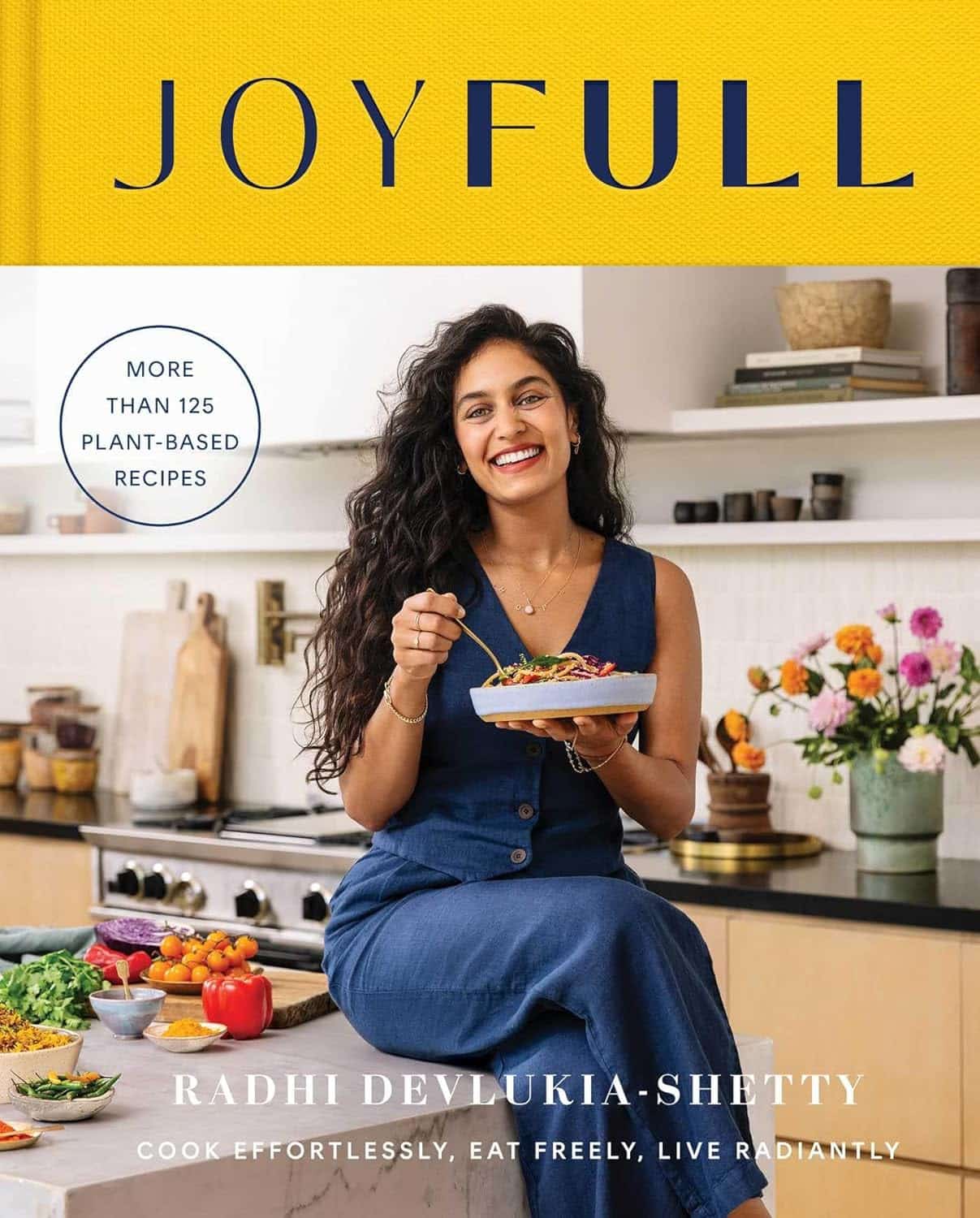
JoyFull – by Radhi Devlukia-Shetty
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We haven’t done a recipe book in a little while, so here’s a good one!
The focus of this book is getting more plants and spices into your diet, and doing it deliciously.
Healthwise, there is nothing controversial here: the recipes are all plant-based, mostly whole-foods, and the items that aren’t whole foods are things like “vanilla extract”.
The recipes themselves (of which there are 125) are presented clearly and simply, one to a double-page (although sometimes there will be a suggested variation on the same double-page), ideal for use in a kitchen bookstand. For each recipe, there’s a clear photo of the end result, so you know what you’re working towards.
The ingredients are not too obscure, and can be acquired from more or less any large supermarket.
Bottom line: if you’re looking to expand your plant-based cooking repertoire in a way that’s not just substitutions, then this book provides an excellent variety.
Click here to check out JoyFull, and get a taste of Ayurvedic cooking!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Coffee, From A Blood Sugar Management Perspective
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our favorite French biochemist (Jessie Inchauspé) is back, and this time, she’s tackling a topic near and dear to this writer’s heart: coffee ☕💕
What to consider
Depending on how you like your coffee, some or all of these may apply to you:
- Is coffee healthy? Coffee is generally healthy, reducing the risk of type 2 diabetes by improving fat burning in the liver and protecting beta cells in the pancreas.
- Does it spike blood sugars? Usually not so long as it’s black and unsweetened. Black coffee can cause small glucose spikes in some people due to stress-induced glucose release, but only if it contains caffeine.
- When is it best to drink it? Drinking coffee after breakfast, especially after a poor night’s sleep, can actually reduce glucose and insulin spikes.
- What about milk? All milks cause some glucose and insulin spikes. While oat milk is generally healthy, for blood sugar purposes unsweetened nut milks or even whole cow’s milk (but not skimmed; it needs the fat) are better options as they cause smaller spikes.
- What about sweetening? Adding sugar to coffee, especially on an empty stomach, obviously leads to large glucose spikes. Alternative sweeteners like stevia or sweet cinnamon are fine substitutes.
For more details on all of those things, plus why Kenyan coffee specifically may be the best for blood sugars, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- The Bitter Truth About Coffee (or is it?)
- Caffeine: Cognitive Enhancer Or Brain-Wrecker?
- 10 Ways To Balance Blood Sugars
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Health Insurers Limit Coverage of Prosthetic Limbs, Questioning Their Medical Necessity
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Michael Adams was researching health insurance options in 2023, he had one very specific requirement: coverage for prosthetic limbs.
Adams, 51, lost his right leg to cancer 40 years ago, and he has worn out more legs than he can count. He picked a gold plan on the Colorado health insurance marketplace that covered prosthetics, including microprocessor-controlled knees like the one he has used for many years. That function adds stability and helps prevent falls.
But when his leg needed replacing last January after about five years of everyday use, his new marketplace health plan wouldn’t authorize it. The roughly $50,000 leg with the electronically controlled knee wasn’t medically necessary, the insurer said, even though Colorado law leaves that determination up to the patient’s doctor, and his has prescribed a version of that leg for many years, starting when he had employer-sponsored coverage.
“The electronic prosthetic knee is life-changing,” said Adams, who lives in Lafayette, Colorado, with his wife and two kids. Without it, “it would be like going back to having a wooden leg like I did when I was a kid.” The microprocessor in the knee responds to different surfaces and inclines, stiffening up if it detects movement that indicates its user is falling.
People who need surgery to replace a joint typically don’t encounter similar coverage roadblocks. In 2021, 1.5 million knee or hip joint replacements were performed in United States hospitals and hospital-owned ambulatory facilities, according to the federal Agency for Healthcare Research and Quality, or AHRQ. The median price for a total hip or knee replacement without complications at top orthopedic hospitals was just over $68,000 in 2020, according to one analysis, though health plans often negotiate lower rates.
To people in the amputee community, the coverage disparity amounts to discrimination.
“Insurance covers a knee replacement if it’s covered with skin, but if it’s covered with plastic, it’s not going to cover it,” said Jeffrey Cain, a family physician and former chair of the board of the Amputee Coalition, an advocacy group. Cain wears two prosthetic legs, having lost his after an airplane accident nearly 30 years ago.
AHIP, a trade group for health plans, said health plans generally provide coverage when the prosthetic is determined to be medically necessary, such as to replace a body part or function for walking and day-to-day activity. In practice, though, prosthetic coverage by private health plans varies tremendously, said Ashlie White, chief strategy and programs officer at the Amputee Coalition. Even though coverage for basic prostheses may be included in a plan, “often insurance companies will put caps on the devices and restrictions on the types of devices approved,” White said.
An estimated 2.3 million people are living with limb loss in the U.S., according to an analysis by Avalere, a health care consulting company. That number is expected to as much as double in coming years as people age and a growing number lose limbs to diabetes, trauma, and other medical problems.
Fewer than half of people with limb loss have been prescribed a prosthesis, according to a report by the AHRQ. Plans may deny coverage for prosthetic limbs by claiming they aren’t medically necessary or are experimental devices, even though microprocessor-controlled knees like Adams’ have been in use for decades.
Cain was instrumental in getting passed a 2000 Colorado law that requires insurers to cover prosthetic arms and legs at parity with Medicare, which requires coverage with a 20% coinsurance payment. Since that measure was enacted, about half of states have passed “insurance fairness” laws that require prosthetic coverage on par with other covered medical services in a plan or laws that require coverage of prostheses that enable people to do sports. But these laws apply only to plans regulated by the state. Over half of people with private coverage are in plans not governed by state law.
The Medicare program’s 80% coverage of prosthetic limbs mirrors its coverage for other services. Still, an October report by the Government Accountability Office found that only 30% of beneficiaries who lost a limb in 2016 received a prosthesis in the following three years.
Cost is a factor for many people.
“No matter your coverage, most people have to pay something on that device,” White said. As a result, “many people will be on a payment plan for their device,” she said. Some may take out loans.
The federal Consumer Financial Protection Bureau has proposed a rule that would prohibit lenders from repossessing medical devices such as wheelchairs and prosthetic limbs if people can’t repay their loans.
“It is a replacement limb,” said White, whose organization has heard of several cases in which lenders have repossessed wheelchairs or prostheses. Repossession is “literally a punishment to the individual.”
Adams ultimately owed a coinsurance payment of about $4,000 for his new leg, which reflected his portion of the insurer’s negotiated rate for the knee and foot portion of the leg but did not include the costly part that fits around his stump, which didn’t need replacing. The insurer approved the prosthetic leg on appeal, claiming it had made an administrative error, Adams said.
“We’re fortunate that we’re able to afford that 20%,” said Adams, who is a self-employed leadership consultant.
Leah Kaplan doesn’t have that financial flexibility. Born without a left hand, she did not have a prosthetic limb until a few years ago.
Growing up, “I didn’t want more reasons to be stared at,” said Kaplan, 32, of her decision not to use a prosthesis. A few years ago, the cycling enthusiast got a prosthetic hand specially designed for use with her bike. That device was covered under the health plan she has through her county government job in Spokane, Washington, helping developmentally disabled people transition from school to work.
But when she tried to get approval for a prosthetic hand to use for everyday activities, her health plan turned her down. The myoelectric hand she requested would respond to electrical impulses in her arm that would move the hand to perform certain actions. Without insurance coverage, the hand would cost her just over $46,000, which she said she can’t afford.
Working with her doctor, she has appealed the decision to her insurer and been denied three times. Kaplan said she’s still not sure exactly what the rationale is, except that the insurer has questioned the medical necessity of the prosthetic hand. The next step is to file an appeal with an independent review organization certified by the state insurance commissioner’s office.
A prosthetic hand is not a luxury device, Kaplan said. The prosthetic clinic has ordered the hand and made the customized socket that will fit around the end of her arm. But until insurance coverage is sorted out, she can’t use it.
At this point she feels defeated. “I’ve been waiting for this for so long,” Kaplan said.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: