The Science of Nutrition – by Rhiannon Lambert
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
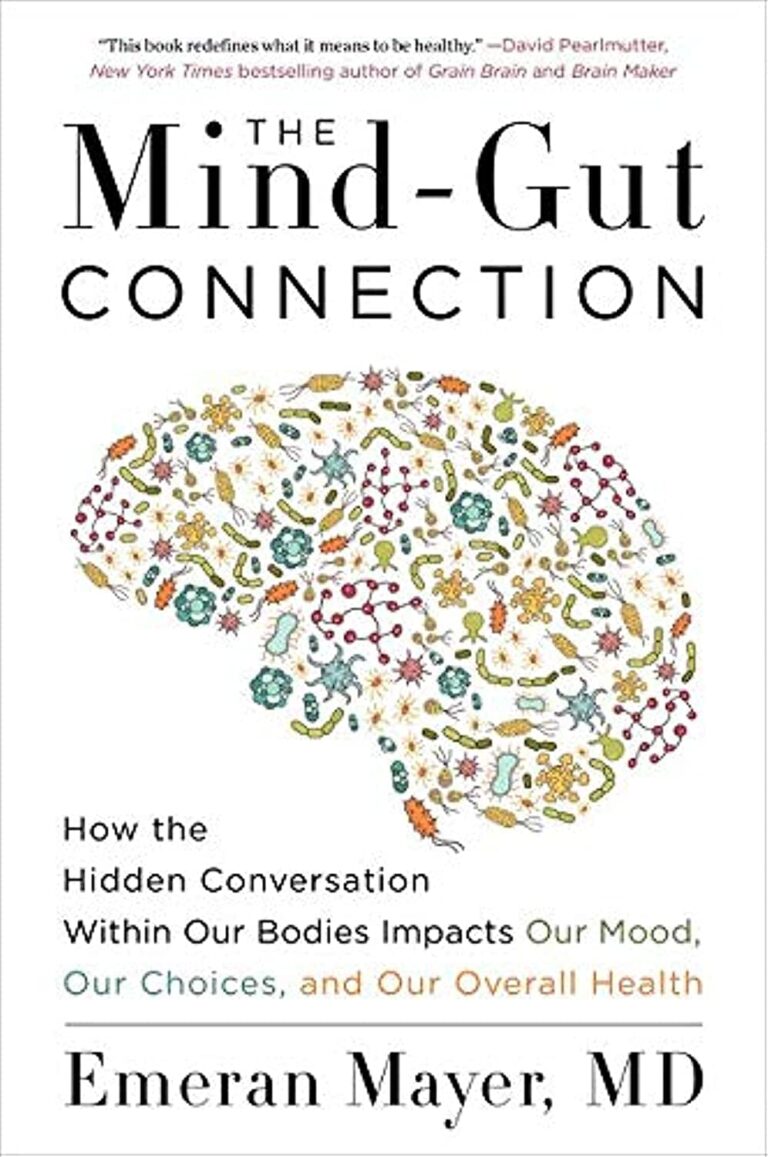
While there are a lot of conflicting dietary approaches out there, the science itself is actually fairly cohesive in most regards. This book does a lot of what we do here at 10almonds, and presents the science in a clear fashion without having any particular agenda to push.
The author is a nutritionist (BSc, MSc, RNutr) and therefore provides an up-to-date evidence-based approach for eating.
As a result, the only part of this book that brings it down in this reviewer’s opinion is the section on Intermittent Fasting. Being not strictly about nutrition, she has less expertise on that topic, and it shows.
The information is largely presented in double-page spreads each answering a particular question. Because of this, and the fact there are colorful graphic representations of information too, we do recommend the print version over Kindle*.
Bottom line: if you like the notion of real science being presented in a clear and simple fashion (we like to think our subscribers do!), then you’ll surely enjoy this book.
Click here to check out the Science of Nutrition, and get a clear overview!
*Writer’s note: I realize I’ve two days in a row recommended this (yesterday because there are checkboxes to check, worksheets to complete, etc), but it’s not a new trend; just how it happened to be with these two books. I love my Kindle dearly, but sometimes print has the edge for one reason or another!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
10 Ways To Delay Aging
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Dr. Colin Rose; he is a Senior Associate of the Royal Society of Medicine. He’s also a main contributor to EduScience, a program funded by the E.U. which is designed to enhance the teaching and learning of science in schools in Europe.
His most recent work has been about aging—and how to delay it. We also reviewed his latest book, here:
Delay Ageing – by Dr. Colin Rose
So, what does he want us to know? The key lies in his compilation of ten ways in which we age on a cellular level, and what we can to do slow each one of those:
Damage to DNA accumulates
While DNA can get damaged without any external stimulus to cause that, there are a lot of modifiable factors that we can do to reduce DNA damage. The list is easy: if it causes cancer, it causes aging.
Thus, check out: Stop Cancer 20 Years Ago
Cells become senescent
Our cells are replaced all the time; some sooner than others, but all of them at some point. The problem occurs when cells are outliving their usefulness. If a cell becomes completely immortal, that is cancer, but happily most don’t. Nevertheless, having senescent (aging) cells in the body means that those senescent cells are what get copied forwards by mitosis, and our DNA becomes like a photocopy of a tattered old photocopy of a tattered old photocopy. Which, needless to say, is not good for our health. So, the best thing to do is to kill them earlier:
Yes, really: Fisetin: The Anti-Aging Assassin
Mitochondria become dysfunctional
Without properly functional mitochondria, no living human cell can do its job properly.
Options: 7 Ways To Boost Mitochondrial Health To Fight Disease
Beneficial genes are switched off, harmful genes are on
It’s easy to think of our genes as being immutable, but epigenetics means that our environment (amongst other factors) can mean that our gene expression changes.
Imagine it this way: your genes are a set of instructions for your body. However, your body will act or not on those instructions, depending on other factors. Hormones often play a big part in this; for example sex hormones tell the body which set of genetic instructions to read (and thus what kind of body to build/rebuild), and cortisol or oxytocin can tell the body which set of contingency plans to activate or suppress (respectively). A milder example is gray hair; genes have the program for it, but many other factors inform the body when, if, and how to do it.
Of more concern when it comes to aging is what goes on with more critical systems, such as the brain, in which the aforementioned DNA damage can cause unhelpful instructions to get interpreted, resulting in epigenetic changes that in turn facilitate age-related degeneration.
As to what can be done, see : Klotho: Unzipping The Genes Of Aging?
Stem cells become exhausted
Stem cells can become different kinds of cells, and thus they’re very useful for maintaining a healthy body. However, they get depleted with age. We can slow down the rate of loss, though; for example, intermittent fasting can help:
Per Dr. Li’s 5 Ways To Beat Cancer (And Other Diseases)
And for more detail, see:
Doctor’s Tip: Regeneration (stem cells) — one of your body’s five defense systems
(complete with lists of foods to eat or avoid for stem cell health)
Cells fail to communicate properly
Cells need to talk to each other constantly, to continue doing their jobs. We are one big organism, after all, and not a haphazard colony of the countless cells that constitute such. However, cell signalling gets worse with age, which in turn precipitates others age-related problems. Fortunately, there are nutrients that can improve cellular communication.
For example: PS, We Love You ← this is about phosphatidylserine, also called “PS”
Telomeres become shorter
These protective caps on our DNA suffer the wear-and-tear so that our DNA doesn’t have to. However, as they get shorter, the DNA can start suffering damage. For this reason, telomere length is considered one of the most “Gold Standard” markers of cellular aging.
Here’s what can be done for that: The Stress Prescription (Against Aging!)
The body fails to sense nutritional intake properly
This is mostly about insulin signalling (though problems can occur in other systems too, but we only have so much room here), so it’s important to take care of that.
See: Turn Back The Clock On Insulin Resistance
Proteins accumulate errors
This is due to DNA damage, of course, but there are specific things that can reduce protein error accumulation; see for example:
A quick fix – preventing protein errors extends lifespan
See also: Rapamycin Can Slow Aging By 20% (But Watch Out)
The microbiome becomes unbalanced
We at 10almonds often mention that gut health affects pretty much every other kind of health, and it’s true for aging as well. So, take care of that microbiome!
Here’s a primer: Gut Health 101
Want to know more about delaying aging beyond the cellular level?
Check out: Age & Aging: What Can (And Can’t) We Do About It?
Take care!
Share This Post
-
Drug companies pay doctors over A$11 million a year for travel and education. Here’s which specialties received the most
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Drug companies are paying Australian doctors millions of dollars a year to fly to overseas conferences and meetings, give talks to other doctors, and to serve on advisory boards, our research shows.
Our team analysed reports from major drug companies, in the first comprehensive analysis of its kind. We found drug companies paid more than A$33 million to doctors in the three years from late 2019 to late 2022 for these consultancies and expenses.
We know this underestimates how much drug companies pay doctors as it leaves out the most common gift – food and drink – which drug companies in Australia do not declare.
Due to COVID restrictions, the timescale we looked at included periods where doctors were likely to be travelling less and attending fewer in-person medical conferences. So we suspect current levels of drug company funding to be even higher, especially for travel.
Monster Ztudio/Shutterstock What we did and what we found
Since 2019, Medicines Australia, the trade association of the brand-name pharmaceutical industry, has published a centralised database of payments made to individual health professionals. This is the first comprehensive analysis of this database.
We downloaded the data and matched doctors’ names with listings with the Australian Health Practitioner Regulation Agency (Ahpra). We then looked at how many doctors per medical specialty received industry payments and how much companies paid to each specialty.
We found more than two-thirds of rheumatologists received industry payments. Rheumatologists often prescribe expensive new biologic drugs that suppress the immune system. These drugs are responsible for a substantial proportion of drug costs on the Pharmaceutical Benefits Scheme (PBS).
The specialists who received the most funding as a group were cancer doctors (oncology/haematology specialists). They received over $6 million in payments.
This is unsurprising given recently approved, expensive new cancer drugs. Some of these drugs are wonderful treatment advances; others offer minimal improvement in survival or quality of life.
A 2023 study found doctors receiving industry payments were more likely to prescribe cancer treatments of low clinical value.
Our analysis found some doctors with many small payments of a few hundred dollars. There were also instances of large individual payments.
Why does all this matter?
Doctors usually believe drug company promotion does not affect them. But research tells a different story. Industry payments can affect both doctors’ own prescribing decisions and those of their colleagues.
A US study of meals provided to doctors – on average costing less than US$20 – found the more meals a doctor received, the more of the promoted drug they prescribed.
Pizza anyone? Even providing a cheap meal can influence prescribing. El Nariz/Shutterstock Another study found the more meals a doctor received from manufacturers of opioids (a class of strong painkillers), the more opioids they prescribed. Overprescribing played a key role in the opioid crisis in North America.
Overall, a substantial body of research shows industry funding affects prescribing, including for drugs that are not a first choice because of poor effectiveness, safety or cost-effectiveness.
Then there are doctors who act as “key opinion leaders” for companies. These include paid consultants who give talks to other doctors. An ex-industry employee who recruited doctors for such roles said:
Key opinion leaders were salespeople for us, and we would routinely measure the return on our investment, by tracking prescriptions before and after their presentations […] If that speaker didn’t make the impact the company was looking for, then you wouldn’t invite them back.
We know about payments to US doctors
The best available evidence on the effects of pharmaceutical industry funding on prescribing comes from the US government-run program called Open Payments.
Since 2013, all drug and device companies must report all payments over US$10 in value in any single year. Payment reports are linked to the promoted products, which allows researchers to compare doctors’ payments with their prescribing patterns.
Analysis of this data, which involves hundreds of thousands of doctors, has indisputably shown promotional payments affect prescribing.
Medical students need to know about this. LightField Studios/Shutterstock US research also shows that doctors who had studied at medical schools that banned students receiving payments and gifts from drug companies were less likely to prescribe newer and more expensive drugs with limited evidence of benefit over existing drugs.
In general, Australian medical faculties have weak or no restrictions on medical students seeing pharmaceutical sales representatives, receiving gifts, or attending industry-sponsored events during their clinical training. They also have no restrictions on academic staff holding consultancies with manufacturers whose products they feature in their teaching.
So a first step to prevent undue pharmaceutical industry influence on prescribing decisions is to shelter medical students from this influence by having stronger conflict-of-interest policies, such as those mentioned above.
A second is better guidance for individual doctors from professional organisations and regulators on the types of funding that is and is not acceptable. We believe no doctor actively involved in patient care should accept payments from a drug company for talks, international travel or consultancies.
Third, if Medicines Australia is serious about transparency, it should require companies to list all payments – including those for food and drink – and to link health professionals’ names to their Ahpra registration numbers. This is similar to the reporting standard pharmaceutical companies follow in the US and would allow a more complete and clearer picture of what’s happening in Australia.
Patients trust doctors to choose the best available treatments to meet their health needs, based on scientific evidence of safety and effectiveness. They don’t expect marketing to influence that choice.
Barbara Mintzes, Professor, School of Pharmacy and Charles Perkins Centre, University of Sydney and Malcolm Forbes, Consultant psychiatrist and PhD candidate, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
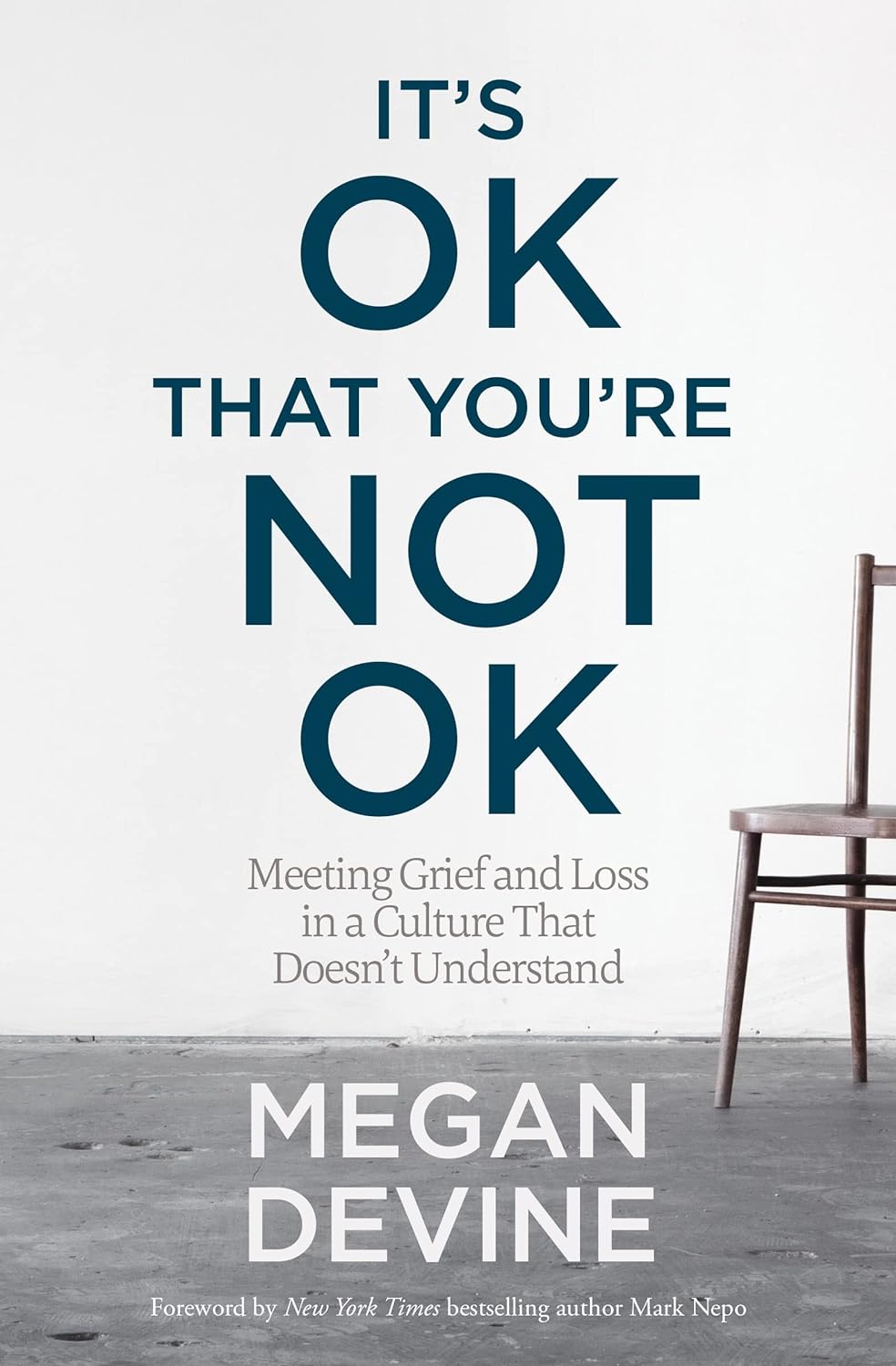
It’s OK That You’re Not OK – by Megan Devine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Firstly, be aware: this is not a cheerful book. If you’re looking for something to life your mood after a loss, it will not be this.
What, then, will you find? A reminder that grief is also the final translation of love, and not necessarily something to be put aside as quickly as possible—or even ever, if we don’t want to.
Too often, society (and even therapists) will correctly note that no two instances of grief are the same (after all, no two people are, so definitely no two relationships are, so how could two instances of grief be?), but will still expect that if most people can move on quickly from most losses, that you should too, and that if you don’t then there is something pathological at hand that needs fixing.
Part one of the book covers this (and more) in a lot of detail; critics have called it a diatribe against the current status quo in the field of grief.
Part two of the book is about “what to do with your grief”, and addresses the reality of grief, how (and why) to stay alive when not doing so feels like a compelling option, dealing with grief’s physical side effects, and calming your mind in ways that actually work (without trying to sweep your grief under a rug).
Parts three and four are more about community—how to navigate the likely unhelpful efforts a lot of people may make in the early days, and when it comes to those people who can and will actually be a support, how to help them to help you.
In the category of criticism, she also plugs her own (paid, subscription-based) online community, which feels a little mercenary, especially as while community definitely can indeed help, the prospect of being promptly exiled from it if you stop paying, doesn’t.
Bottom line: if you have experienced grief and felt like moving on was the right thing to do, then this book isn’t the one for you. If, on the other hand, your grief feels more like something you will carry just as you carry the love you feel for them, then you’ll find a lot about that here.
Share This Post
Related Posts
-
Inheritance – by Dr. Sharon Moalem
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We know genes make a big difference to a lot about us, but how much? And, the genes we have, we’re stuck with, right?
Dr. Sharon Moalem shines a bright light into some of the often-shadowier nooks and crannies of our genetics, covering such topics as:
- How much can (and can’t) be predicted from our parents’ genes—even when it comes to genetic traits that both parents have, and Gregor Mendel himself would (incorrectly) think obvious
- How even something so seemingly simple and clear as genetic sex, very definitely isn’t
- How traumatic life events can cause epigenetic changes that will scar us for generations to come
- How we can use our genetic information to look after our health much better
- How our life choices can work with, or overcome, the hand we got dealt in terms of genes
The style of the book is conversational, down to how there’s a lot of “I” and “you” in here, and the casual style belies the heavy, sharp, up-to-date science contained within.
Bottom line: if you’d like insight into the weird and wonderful nuances of genetics as found in this real, messy, perfectly chaotic world, this book is an excellent choice.
Click here to check out Inheritance, and learn more about yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Top Foods Against Neuroinflammation
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Chronic inflammation is something you might feel in your joints, but it will usually be in the brain too. There, neuroinflammation can disrupt brain function, affecting stress responses, mood, cognition, and even alter brain structure. It’s also heavily implicated in the pathogenesis of various forms of dementia.
What to do about it
Dr. Tracey Marks, psychiatrist, bids us eat:
- Fatty fish: omega-3-rich fish like salmon reduce neuroinflammation.
- Leafy greens: spinach, kale, and collards protect brain cells and support neurotransmitter production.
- Berries: blueberries and strawberries improve memory and protect neurons.
- Nuts and seeds: walnuts, almonds, and flaxseeds support brain health and reduce inflammation.
- Turmeric: curcumin combats inflammation and supports neuron growth (best with supplements).
- Fermented foods: yogurt and sauerkraut improve gut health, benefiting the brain via the gut-brain axis; not just the vagus nerve, but also, remember that various neurotransmitters (including serotonin) are made in the gut.
Of course, you should also avoid alcohol, nicotine, red meat, processed meat, and ideally also white flour products, and sugary foods (unless they are also rich in fiber, like whole fruit).
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How to Prevent (or Reduce) Inflammation
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Aging For Beginners – by Ezra Bayda & Elizabeth Hamilton
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This one’s not about how to avoid aging, but rather, how to be at peace with whatever aging may be happening, perhaps despite our best efforts.
The book is dedicated:
❝To all the starving and suffering children throughout the world, with the wish that they may someday have the opportunity to experience the life of a contented geriatric❞
It’s a stark reminder that old age is a privilege that many do not get to enjoy, thanks to poverty, disease, wars, and accidents and incidents along the way.
So, how to go about making the very most of what we have, for those of us who are perhaps going gray in a comfortable, safe environment?
The answer may surprise you: the authors tackle things head-on without dressing old age up in euphemisms or platitudes—they cover not just the physical decline that typically occurs eventually, but also the impact of the physical pain that this may bring, the way this may play into loneliness and helplessness, and perhaps anxiety and/or depression. And, of course, the topic of grief and loss, that for most of us becomes all the more part of our lives as we get older. For that matter, our own mortality is also something the authors come back to from start to finish.
Thus, this is not necessarily a cheerful book—but it gives the tools such that we can be cheerful about life in general, in the face of all the aforementioned things, without pretending that things that are not good are good, just, making our peace with what is, and making the most out of what we have.
The authors are Zen teachers with decades of experience, and this book is heavily influenced by Zen principles. And yes, it does teach meditation too, but that’s just one tool in the toolbox.
The style is deep and yet very readable, heavy of tone and at the same time inspiring of lightness of heart.
Bottom line: if you’d like to worry less about aging (while still doing all you want to stay young), this book can certainly help with that.
Click here to check out Aging For Beginners, and be at peace with yourself.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: