The Most Anti Aging Exercise
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve referenced this (excellent) video before, but never actually put it under the spotlight in one of these features, so here we go!
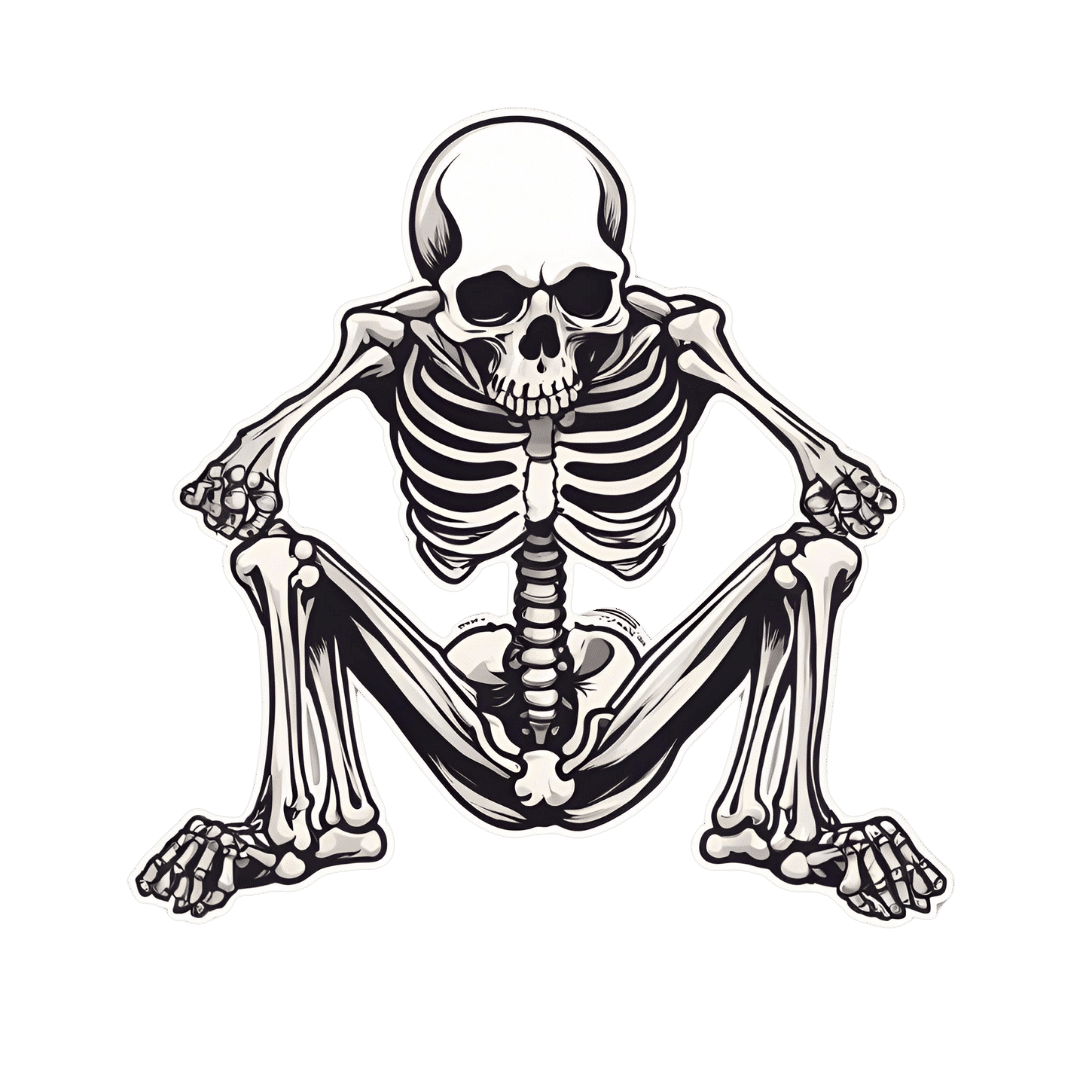
Deep squats
It’s about deep squats, also called Slav squats, Asian squats, sitting squats, resting squats, or various other names. However, fear not; you don’t need to be Slavic or Asian to do it; you just need to practice.
As for why this is called “anti-aging”, by the way, it’s because being able to get up off the ground is one of the main tests of age-related mobility decline, and if you can deep-squat comfortably, then you can do that easily. And so long as you continue being able to deep-squat comfortably, you’ll continue to be able to get up off the ground easily too, because you have the strength in the right muscles, as well as the suppleness, comfort with range of motion, and balance (those stabilizing muscles are used constantly in a deep squat, whereas Western lifestyle sitting leaves those muscles very neglected and thus atrophied).
Epidemiological note: chairs, couches, and assorted modern conveniences reduce the need for squatting in daily life, leading to stiffness in joints, muscles, tendons, and ligaments. Many adults in developed countries struggle with deep squats due to lack of use, not aging. Which is a problem, because a lack of full range of motion in joints causes wear and tear, leading to chronic pain and degenerative joint diseases. People in countries where squatting is a common resting position have lower incidences of osteoarthritis, for example—contrary to what some might expect, squatting does not harm joints but rather protects them from arthritis and knee pain. Strengthening leg muscles through squatting can alleviate knee pain, whereas knee pain is often worsened by inactivity.
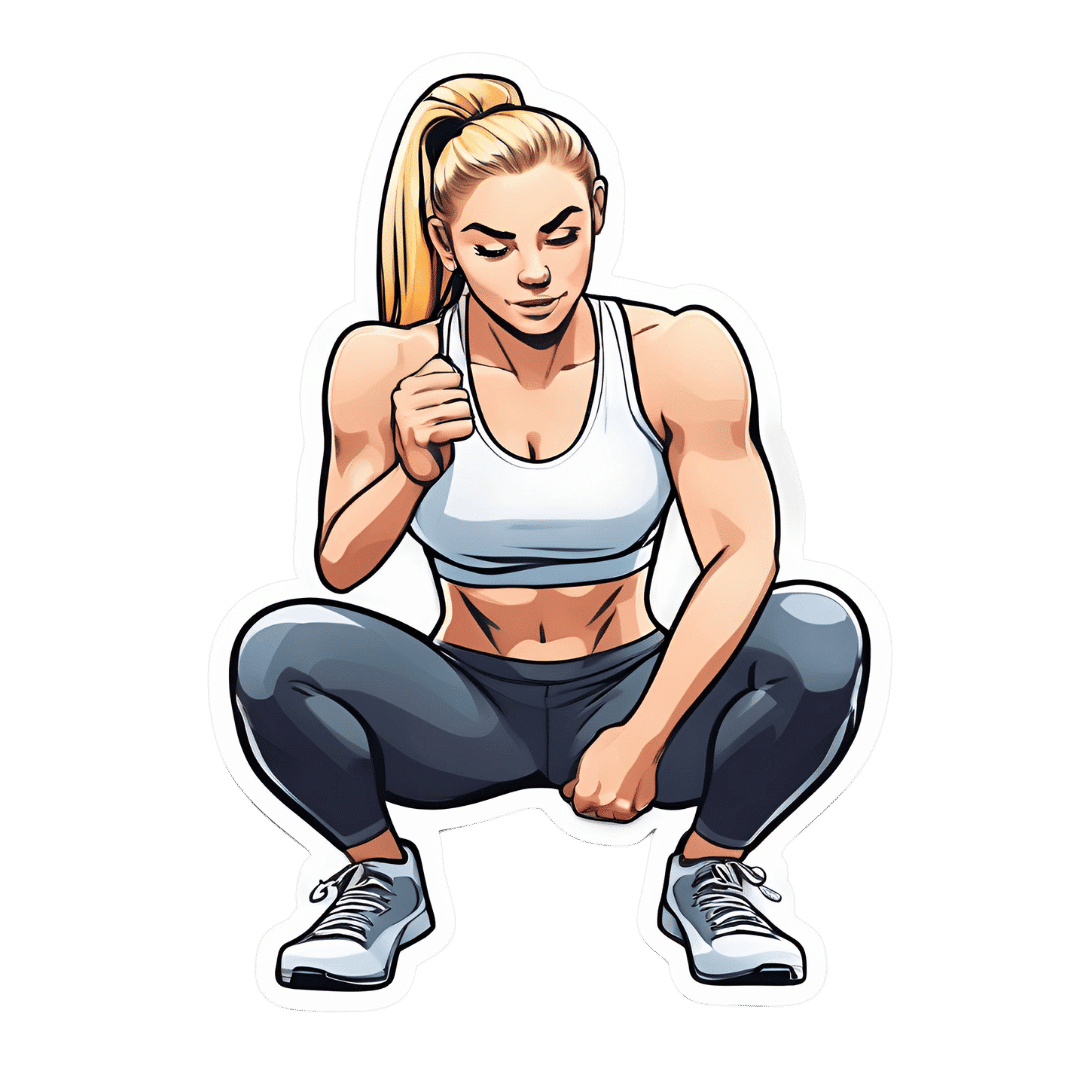
Notwithstanding the thumbnail, which is showing an interim position, one’s feet should be flat on the ground, by the way, and one’s butt should be nearby, just a few inches off the ground (in other words, the position that we see her in for most of this video).
Troubleshooting: if you’re accustomed to sitting in chairs a lot, then this may be uncomfortable at first. Zuzka advises us to go gently, and/but gradually increase our range of motion and (equally importantly) duration in the resting position.
You can use a wall or doorway to partially support you, at first, if you struggle with mobility or balance. Just try to gradually use it less, until you’re comfortable deep-squatting with no support.
Since this is not an intrinsically very exciting exercise, once you build up the duration for which you’re comfortable deep-squatting, it can be good to get in the habit of “sitting” this way (i.e. deep squatting, still butt-off-the-floor, but doing the job of sitting) while doing other things such as working (if you have an appropriate work set-up for that*), reading, or watching TV.
*this is probably easiest with a laptop placed on an object/surface of appropriate height, such as a coffee table or such. As a bonus, having your hands in front of you while working will also bring your center of gravity forwards a bit, making the position easier and more comfortable to maintain. This writer (hi, it’s me) prefers her standing desk for work in general, with a nice ergonomic keyboard and all that, but if using a laptop from time to time, then squatting is a very good option.
In terms of working up duration, if you can only manage seconds to start with, that’s fine. Just do a few more seconds each time, until it’s 30, 60, 120, and so on until it’s 5 minutes, 10, 15, and so on.
You can even start that habit-forming while you’re still in the “seconds at a time” stage! You can deep-squat just for some seconds while you:
- pick up something from the floor
- check on something in the oven
- get something out of the bottom of the fridge
…etc!
For more on all this, plus many visual demonstrations including interim exercises to get you there if it’s difficult for you at first, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Mobility For Now & For Later: Train For The Marathon That Is Your Life!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Overcome Front-Of-Hip Pain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Alyssa Kuhn, physiotherapist, demonstrates how:
One, two, three…
One kind of pain affects a lot of related things: hip pain has an impact on everything that’s connected to the pelvis, which is basically the rest of the body, but especially the spine itself. For this reason, it’s critical to keep it in as good condition as possible.
Two primary causes of hip stiffness and pain:
- Anterior pelvic tilt due to posture, weight distribution, or pain. This tightens the front muscles and weakens the back muscles.
- Prolonged sitting, which tightens the hip muscles due to inactivity.
Three exercises are recommended by Dr. Kuhn to relieve pain and stiffness:
- Bridge exercise:
- Lie on a firm surface with your knees bent.
- Push through your feet, engage your hamstrings, and flatten your lower back.
- Hold for 3–5 seconds, relax, and repeat (10–20 reps).
- Wall exercise with arms:
- Stand with your lower back against the wall, feet a step away.
- Tilt your hips backwards, keeping your lower back in contact with the wall.
- Alternate lifting one arm at a time while maintaining back contact with the wall (10–20 reps).
- Wall exercise with legs:
- Same stance as the previous exercise but wider now.
- Lift one heel at a time while keeping your hips stable and your back against the wall.
- Practice for 30–60 seconds, maintaining good form.
As ever, consistency is key for long-term relief. Dr. Kuhn recommends doing these regularly, especially before any expected periods of prolonged sitting (e.g. at desk, or driving, etc). And of course, do try to reduce, or at least break up, those sitting marathons if you can.
For more on all of this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
-
The New Menopause – by Dr. Mary Claire Haver
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author is most famous for “The Galveston Diet”, which book is astonishingly similar in its content, chapters, format, etc to Nikki Williams’ “It’s Not You, It’s Your Hormones” which came out a few years previously but didn’t get the same marketing.
Nonetheless, this time Dr. Haver has something new to add, and we think it’s worth a read.
The general theme of this book is a comprehensive overview of the menopause, experientially (subjective to the person going through it) and empirically (by science), from start to finish and beyond. This book’s more about human physiology, and less about diet than the previous.
Dr. Haver also discusses in-depth how estrogen is thought of as a sex hormone (and it is), to the point that people consider it perhaps expendable, and forget (or are simply unaware) that we have estrogen receptors throughout our bodies and estrogen is vital for maintaining many other bodily functions, including your heart, cognitive function, bone integrity, blood sugar balance, and more.
(in case you’re wondering “why don’t men fall to bits, then?”, don’t worry, their testosterone does these things for them. Testosterone is orders of magnitude less potent than estrogen, mg for mg, so they need a lot more of it, but under good conditions they produce plenty so it’s fine)
But, the amount of testosterone available to peri/postmenopausal women is simply not enough to do that job (and it’d also result in a transition of secondary sex characteristics, which for most people would be very unwanted), so, something else needs to be done.
Dr. Haver also discusses in detail the benefits and risks of HRT and how to get/manage them, respectively, with the latest up-to-date research (at time of going to print; the book was published in April 2024).
Bottom line: if you want to know what’s going on with your peri- or post-menopausal body and how it could be better (or if you want to know what’s going on with someone else approaching/experiencing menopause), then this is a top-tier book.
Click here to check out The New Menopause, and know what’s going on and what to do about it!
Share This Post
-
Olive Oil vs Coconut Oil – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing extra virgin olive oil to cold-pressed coconut oil, we picked the olive oil.
Why?
While the cold-pressed coconut oil may offer some health benefits due to its lauric acid content, its 80–90% saturated fat content isn’t great for most people. It’s a great oil when applied topically for healthy skin and hair, though!
The extra virgin olive oil has a much more uncontroversially healthy blend of triglycerides, and (in moderation) is universally recognized as very heart-healthy.
Your local supermarket, most likely, has a good extra virgin olive oil, but if you’d like to get some online, here’s an example product on Amazon for your convenience.
Share This Post
Related Posts
-
Get Better Sleep: Beyond “Sleep Hygiene”
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Better Sleep, Better Life!
This is Arianna Huffington. Yes, that Huffington, of the Huffington Post. But! She’s also the CEO of Thrive Global, a behavior change tech company with the mission of changing the way we work and live—in particular, by challenging the idea that burnout is the required price of success.
The power of better sleep
Sleep is a very important, but most often neglected, part of good health. Here are some of Huffington’s top insights from her tech company Thrive, and as per her “Sleep Revolution” initiative.
Follow your circadian rhythm
Are you a night owl or a morning lark? Whichever it is, roll with it, and plan around that if your lifestyle allows for such. While it is possible to change from one to the other, we do have a predisposition towards one or the other, and will generally function best when not fighting it.
This came about, by the way, because we evolved to have half of us awake in the mornings and half in the evenings, to keep us all safe. Socially we’ve marched onwards from that point in evolutionary history, but our bodies are about a hundred generations behind the times, and that’s just what we have to work with!
Don’t be afraid (or ashamed!) to take naps
Naps, done right, can be very good for the health—especially if we had a bad night’s sleep the previous night.
Thrive found that workers are more productive when they have nap rooms, and (following on a little from the previous point) are allowed to sleep in or work from home.
See also: How To Nap Like A Pro (No More “Sleep Hangovers”!)
Make sure you have personal space available in bed
The correlation between relationship satisfaction and sleeping close to one’s partner has been found to be so high that it’s even proportional: the further away a couple sleeps from each other, the less happy they are. But…
Partners who got good sleep the previous night, will be more likely to want intimacy on any given night—at a rate of an extra 14% per extra hour of sleep the previous night. So, there’s a trade-off, as having more room in bed tends to result in better sleep. Time to get a bigger bed?
What gets measured, gets done
This goes for sleep, too! Not only does dream-journaling in the morning cue your subconscious to prepare to dream well the following night, but also, sleep trackers and sleep monitoring apps go a very long way to improving sleep quality, even if no extra steps are consciously taken to “score better”.
We’ve previously reviewed some of the most popular sleep apps; you can check out for yourself how they measured up:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Head Over Hips
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about managing osteoarthritis (or ideally: avoiding it, but that’s not always an option on the table, of course), so here’s a primer/refresher before we get into the meat of today’s article:
Avoiding/Managing Osteoarthritis
When the head gets in the way
Research shows that the problem with recovery in cases of osteoarthritis of the hip is in fact often not the hip itself, but rather, the head:
❝In fact, the stronger your muscles are, the more protected your joint is, and the less pain you will experience.
Our research has shown that people with hip osteoarthritis were unable to activate their muscles as efficiently, irrespective of strength.
Basically, people with hip arthritis are unable to activate their muscles properly because the brain is actively putting on the brake to stop them from using the muscle.❞
This is a case of a short-term protective response being unhelpful in the long-term. If you injure yourself, your brain will try to inhibit you from exacerbating that injury, such as by (for example) disobliging you from putting weight on an injured joint.
This is great if you merely twisted an ankle and just need to sit back and relax while your body works its healing magic, but it’s counterproductive if it’s a chronic issue like osteoarthritis. In such (i.e. chronic) cases, avoidance of use of the joint will simply cause atrophy of the surrounding muscle and other tissues, leading to more of the very wear-and-tear that led to the osteoarthritis in the first place.
So… How to deal with that?
You probably can exercise
It’s easy to get caught between the dichotomy of “exercise and inflame your joints” vs “rest and your joints seize up”, which is not pleasant.
However, the trick lies in how you exercise, per joint type:
When Bad Joints Stop You From Exercising (5 Things To Change)
…which to be clear, isn’t a case of “avoid using the joint that’s bad”, but is rather “use it in this specific way, so that it gets stronger without doing it more damage in the process”.
Which is exactly what is needed!
Further resources
For those who like learning from short videos, here’s a trio of helpers (along with our own text-based overview for each):
- The Most Underrated Hip Mobility Exercise (Not Stretching)
- Overcome Front-Of-Hip Pain
- 10 Tips To Reduce Morning Pain & Stiffness With Arthritis
And for those who prefer just reading, here’s a book we reviewed on the topic:
11 Minutes to Pain-Free Hips – by Melinda Wright
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Princess of Wales wants to stay cancer-free. What does this mean?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Catherine, Princess of Wales, has announced she has now completed a course of preventive chemotherapy.
The news comes nine months after the princess first revealed she was being treated for an unspecified form of cancer.
In the new video message released by Kensington Palace, Princess Catherine says she’s focused on doing what she can to stay “cancer-free”. She acknowledges her cancer journey is not over and the “path to recovery and healing is long”.
While we don’t know the details of the princess’s cancer or treatment, it raises some questions about how we declare someone fully clear of the disease. So what does being – and staying – “cancer-free” mean?
Pete Hancock/Shutterstock What’s the difference between being cancer-free and in remission?
Medically, “cancer-free” means two things. First, it means no cancer cells are able to be detected in a patient’s body using the available testing methods. Second, there is no cancer left in the patient.
These might sound basically the same. But this second aspect of “cancer-free” can be complicated, as it’s essentially impossible to be sure no cancer cells have survived a treatment.
Testing can’t completely rule out the chance some cancer cells have survived treatment. Andrewshots/Shutterstock It only takes a few surviving cells for the cancer to grow back. But these cells may not be detectable via testing, and can lie dormant for some time. The possibility of some cells still surviving means it is more accurate to say a patient is “in remission”, rather than “cancer-free”.
Remission means there is no detectable cancer left. Once a patient has been in remission for a certain period of time, they are often considered to be fully “cancer-free”.
Princess Catherine was not necessarily speaking in the strict medical sense. Nonetheless, she is clearly signalling a promising step in her recovery.
What happens during remission?
During remission, patients will usually undergo surveillance testing to make sure their cancer hasn’t returned. Detection tests can vary greatly depending on both the patient and their cancer type.
Many tests involve simply looking at different organs to see if there are cancer cells present, but at varying levels of complexity.
Some cancers can be detected with the naked eye, such as skin cancers. In other cases, technology is needed: colonoscopies for colorectal cancers, X-ray mammograms for breast cancers, or CT scans for lung cancers. There are also molecular tests, which test for the presence of cancer cells using protein or DNA from blood or tissue samples.
For most patients, testing will continue for years at regular intervals. Surveillance testing ensures any returning cancer is caught early, giving patients the best chance of successful treatment.
Remaining in remission for five years can be a huge milestone in a patient’s cancer journey. For most types of cancer, the chances of cancer returning drop significantly after five years of remission. After this point, surveillance testing may be performed less frequently, as the patients might be deemed to be at a lower risk of their cancer returning.
Skin cancer may be detected by the naked eye, but many other cancers require technology for detection and monitoring. wavebreakmedia/Shutterstock Measuring survival rates
Because it is very difficult to tell when a cancer is “cured”, clinicians may instead refer to a “five-year survival rate”. This measures how likely a cancer patient is to be alive five years after their diagnosis.
For example, data shows the five-year survival rate for bowel cancer among Australian women (of all ages) is around 70%. That means if you had 100 patients with bowel cancer, after five years you would expect 70 to still be alive and 30 to have succumbed to the disease.
These statistics can’t tell us much about individual cases. But comparing five-year survival rates between large groups of patients after different cancer treatments can help clinicians make the often complex decisions about how best to treat their patients.
The likelihood of cancer coming back, or recurring, is influenced by many factors which can vary over time. For instance, approximately 30% of people with lung cancer develop a recurrent disease, even after treatment. On the other hand, breast cancer recurrence within two years of the initial diagnosis is approximately 15%. Within five years it drops to 10%. After ten, it falls below 2%.
These are generalisations though – recurrence rates can vary greatly depending on things such as what kind of cancer the patient has, how advanced it is, and whether it has spread.
Staying cancer-free
Princess Catherine says her focus now is to “stay cancer-free”. What might this involve?
How a cancer develops and whether it recurs can be influenced by things we can’t control, such as age, ethnicity, gender, genetics and hormones.
However, there are sometimes environmental factors we can control. That includes things like exposure to UV radiation from the sun, or inhaling carcinogens like tobacco.
Lifestyle factors also play a role. Poor diet and nutrition, a lack of exercise and excessive alcohol consumption can all contribute to cancer development.
Research estimates more than half of all cancers could potentially be prevented through regular screening and maintaining a healthy lifestyle (not to mention preventing other chronic conditions such as heart disease and diabetes).
Recommendations to reduce cancer risk are the same for everyone, not just those who’ve had treatment like Princess Catherine. They include not smoking, eating a nutritious and balanced diet, exercising regularly, cutting down on alcohol and staying sun smart.
Amali Cooray, PhD Candidate in Genetic Engineering and Cancer, WEHI (Walter and Eliza Hall Institute of Medical Research) ; John (Eddie) La Marca, Senior Research Officer, Blood Cells and Blood Cancer, WEHI (Walter and Eliza Hall Institute of Medical Research) , and Sarah Diepstraten, Senior Research Officer, Blood Cells and Blood Cancer Division, WEHI (Walter and Eliza Hall Institute of Medical Research)
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: