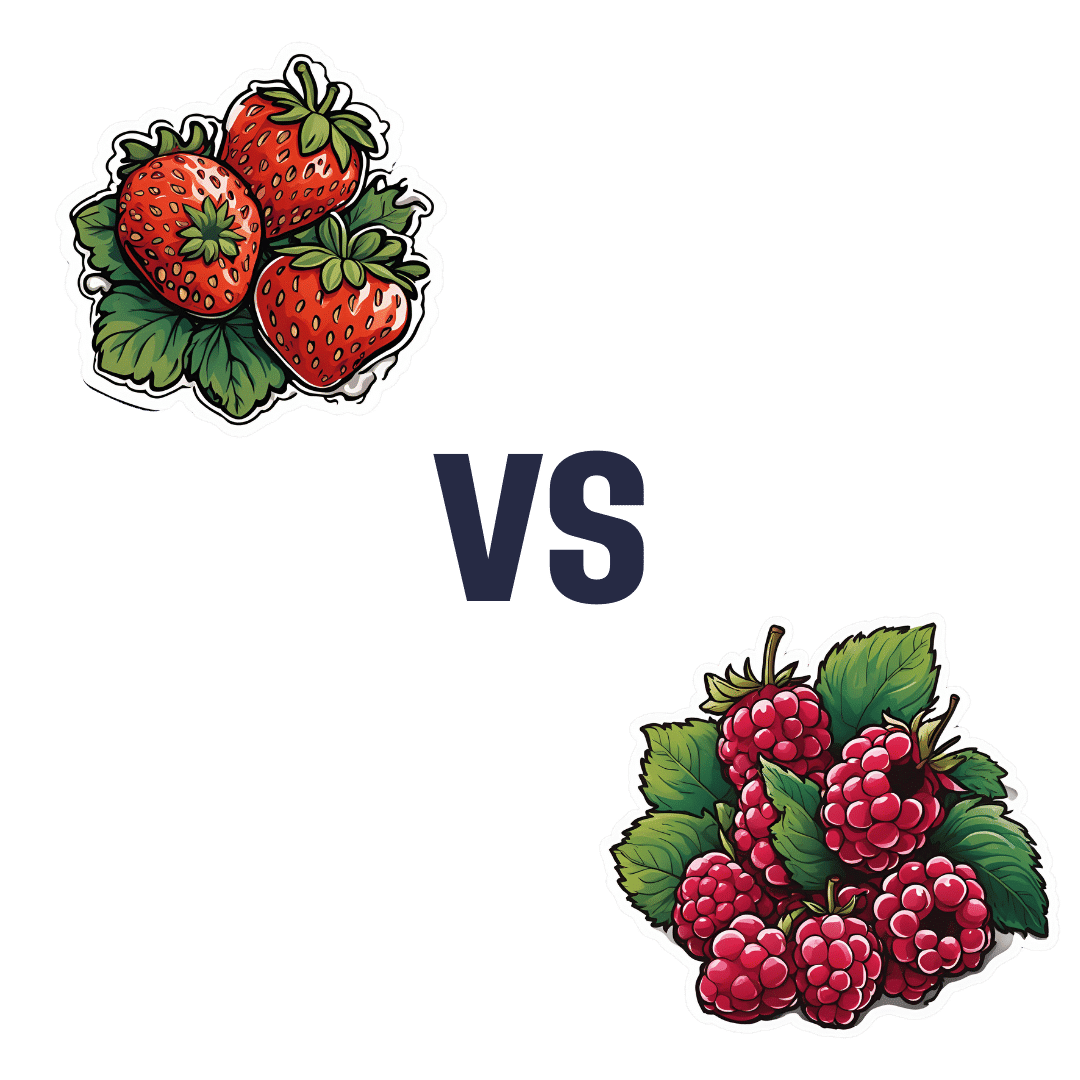
Strawberries vs Raspberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing strawberries to raspberries, we picked the raspberries.
Why?
They’re both very respectable fruits, of course! But it’s not even close, and there is a clear winner here…
In terms of macros, the biggest difference is that raspberries have moderately more carbs, and more than 3x the fiber. Technically they also have 2x the protein, but that’s a case of “two times almost nothing is still almost nothing”. All in all, and especially for the “more than 3x the fiber” (6.5g/100g to strawberries’ 2g/100g), this one’s an easy win for raspberries.
When it comes to vitamins, strawberries have more vitamin C, while raspberries have more of vitamins A, B1, B2, B3, B5, B6, E, K, and choline. Another clear and easy win for raspberries.
In the category of minerals, guess what, raspberries win this hands-down, too: strawberries are higher in selenium, while raspberries have more calcium, copper, iron, magnesium, manganese, phosphorus, and zinc.
Adding up all the individual wins (all for raspberries), it’s not hard to say that raspberries win the day. Still, of course, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
From Apples to Bees, and High-Fructose Cs: Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
11 Minutes to Pain-Free Hips – by Melinda Wright
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If hips don’t lie, what are yours saying to you? If what they’re saying to you sounds like a cry for help sometimes, this is the book to get you onto a better track.
The hip is the largest joint in your body, and it bears a lot of weight. So it’s little wonder if sometimes they’d like a word with the boss. The question is: what will you do about it? Melinda Wright has suggestions to keep your hips—and you—happy.
She spends the first couple of chapters introducing key concepts, and some anatomy and physiology that’ll be good to know.
Then we’re into resistance stretching, basic hip exercises, all the way through to more advanced stuff. There are very clear photos for each. One thing that stands out about this book is each exercise is not just explained simply and clearly, but also offers “easing oneself in” exercises. After all, we’re not all at the same starting point.
The book finishes off with some more holistic advice about chronic pain management, based on her personal experience with scoliosis, and some dietary tips to reduce joint pain and inflammation too.
All in all, a very helpful book!
Pick up 11 “Minutes to Pain-Free Hips” at Amazon today!
^You will also see options for pain-free back, and pain-free neck, by the same author
Share This Post
-
How To Kill Laziness
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Laziness Is A Scooby-Doo Villain.
Which means: to tackle it requires doing a Scooby-Doo unmasking.
You know, when the mystery-solving gang has the “ghost” or “monster” tied to a chair, and they pull the mask off, to reveal that there was no ghost etc, and in fact it was a real estate scammer or somesuch.
Social psychologist Dr. Devon Price wrote about this (not with that metaphor though) in a book we haven’t reviewed yet, but will one of these days:
Laziness Does Not Exist – by Dr. Devon Price (book)
In the meantime, and perhaps more accessibly, he gave a very abridged summary for Medium:
Medium | Laziness Does Not Exist… But unseen barriers do (11mins read)
Speaking of barriers, Medium added a paywall to that (the author did not, in fact, arrange the paywall as Medium claim), so in case you don’t have an account, he kindly made the article free on its own website, here:
Devon Price | Laziness Does Not Exist… But unseen barriers do (same article; no paywall)
He details problems that people get into (ranging from missed deadlines to homelessness), that are easily chalked up to laziness, but in fact, these people are not lazily choosing to suffer, and are usually instead suffering from all manner of unchosen things, ranging from…
- imposter syndrome / performance anxiety,
- perfectionism (which can overlap a lot with the above),
- social anxiety and/or depression (these also can overlap for some people),
- executive dysfunction in the brain, and/or
- just plain weathering “the slings and arrows of outrageous fortune [and] the heartache and the thousand natural shocks that flesh is heir to”, to borrow from Shakespeare, in ways that aren’t always obviously connected—these things can be great or small, it could be a terminal diagnosis of some terrible disease, or it could be a car breakdown, but the ripples spread.
And nor are you, dear reader, choosing to suffer (even if sometimes it appears otherwise)
Unless you’re actually a masochist, at least, in which case, you do you. But for most of us, what can look like laziness or “doing it to oneself” is usually a case of just having one or more of the above-mentioned conditions in place.
Which means…
That grace we just remembered above to give to other people?
Yep, we should give that to ourselves too.
Not as a free pass, but in the same way we (hopefully) would with someone else, and ask: is there some problem I haven’t considered, and is there something that would make this easier?
Here are some tools to get you started:
- Imposter Syndrome (And Why Almost Everyone Has It)
- Perfectionism, And How To Make Yours Work For You
- How To Set Anxiety Aside
- Mental Health First-Aid (To Get Yourself Or A Loved One Through Depression)
- Procrastination, And How To Pay Off The To-Do List Debt
- Take This Two-Minute Executive Dysfunction Test
Take care!
Share This Post
-
Strong Curves – by Bret Contreras & Kellie Davis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The title (and subtitle) is, of course, an appeal to vanity. However, the first-listed author is well-known as “The Glute Guy”, and he takes this very seriously, not just for aesthetic reasons but also for practical reasons.
After all, when it comes to posture and stability, a lot rests on our hips, and hips, well, they rest on our butt and thighs. What’s more, the gluteus maximus is the largest muscle in the human body, so really, is it a good one to neglect? Probably not, and your lower back will definitely thank you for keeping your glutes in good order, too.
That said, while it’s a focal point, it’s not the be-all-and-end-all, and this book does cover the whole body.
The book takes the reader from “absolute beginner” to “could compete professionally”, with clearly-illustrated and well-described exercises. We also get a strong “crash course” in the relevant anatomy and physiology, and even a chapter on nutrition, which is a lot better than a lot of exercise books’ efforts in that regard.
For those who like short courses, this book has several progressive 12-week workout plans that take the reader from a very clear starting point to a very clear goal point.
Another strength of the book is that while a lot of exercises expect (and require) access to a gym, there are also whole sections of “at home / bodyweight” exercises, including 12-week workout plans for such, as described above.
Bottom line: there’s really nothing bad that this reviewer can find to say about this one—highly recommendable to any woman who wants to get strong while keeping a feminine look.
Click here to check out Strong Curves, and rebuild your body, your way!
PS: at first glance, the cover art looks like an AI model; it’s not; that’s the co-author Kellie Davis, who also serves as the model through the book’s many photographic illustrations.
Share This Post
Related Posts
-
The Connection Cure – by Julia Hotz
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may recognize some of the things in the subtitle as being notable elements of the Blue Zones supercentenarians’ lifestyles, but this book looks at numerous quite diverse countries, and people from many walks of life.
What they have in common—and this is mostly a very person-centered book, relying a lot on case studies, with additional references coming from wider sociological data—is social prescribing.
What is social prescribing? That’s what the author (a journalist by general profession) answers comprehensively here, and it’s about looking at the ways medical problems can often have nonmedical solutions. It doesn’t necessarily mean that walking will cure your cancer or art will cure your diabetes, but it does mean that very often a key part of an unhealthy lifestyle is fundamentally something that can be fixed by one or more of: movement, nature, art, service, and belonging.
She looks at social prescribing in its birthplace (the UK, where cheap solutions that are nevertheless evidence-based are very much prioritized), in big countries like Canada and Australia, in aging countries like Singapore and South Korea, and yes, also in the #1 country of pill prescribing, the US.
The structure of the book is interesting, we first have 5 person-centered chapters addressing each of the social prescribing aspects and how they helped in two example case studies for each one, then 5 country-by-country epidemiological chapters looking at the big picture, then 5 person-centered chapters again, this time looking at personalizing social prescribing for oneself (this section of the book being headed “Social Prescribing For You And Me”), looking at what is going on in one’s life and health, which of the 5 elements might be missing, and what tangible goal-oriented benefits can—according to the evidence—be obtained by tending to what one actually needs in terms of social prescribing.
The style is narrative and journalistic, with very little hard science, but very little that’s wishy-washy either. It is, in short, a pleasant and informative read that helps the reader really understand social prescribing, the better to implement it in our own lives.
Bottom line: if you like having extra nonmedical approaches to avoid or alleviate medical problems, then this book will really help you achieve that.
Click here to check out The Connection Cure, and get social prescribing!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Codependency Isn’t What Most People Think It Is
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Codependency isn’t what most people think it is
In popular parlance, people are often described as “codependent” when they rely on each other to function normally. That’s interdependent mutualism, and while it too can become a problem if a person is deprived of their “other half” and has no idea how to do laundry and does not remember to take their meds, it’s not codependency.
Codependency finds its origins in the treatment and management of alcoholism, and has been expanded to encompass other forms of relationships with dependence on substances and/or self-destructive behaviors—which can be many things, including the non-physical, for example a pattern of irresponsible impulse-spending, or sabotaging one’s own relationship(s).
We’ll use the simplest example, though:
- Person A is (for example) an alcoholic. They have a dependency.
- Person B, married to A, is not an alcoholic. However, their spouse’s dependency affects them greatly, and they do what they can to manage that, and experience tension between wanting to “save” their spouse, and wanting their spouse to be ok, which latter, superficially, often means them having their alcohol.
Person B is thus said to be “codependent”.
The problem with codependency
The problems of codependency are mainly twofold:
- The dependent partner’s dependency is enabled and thus perpetuated by the codependent partner—they might actually have to address their dependency, if it weren’t for their partner keeping them from too great a harm (be it financially, socially, psychologically, medically, whatever)
- The codependent partner is not having a good time of it either. They have the stress of two lives with the resources (e.g. time) of one. They are stressing about something they cannot control, understandably worrying about their loved one, and, worse: every action they might take to “save” their loved one by reducing the substance use, is an action that makes their partner unhappy, and causes conflict too.
Note: codependency is often a thing in romantic relationships, but it can appear in other relationships too, e.g. parent-child, or even between friends.
See also: Development and validation of a revised measure of codependency
How to deal with this
If you find yourself in a codependent position, or are advising someone who is, there are some key things that can help:
- Be a nurturer, not a rescuer. It is natural to want to “rescue” someone we care about, but there are some things we cannot do for them. Instead, we must look for ways to build their strength so that they can take the steps that only they can take to fix the problem.
- Establish boundaries. Practise saying “no”, and also be clear over what things you can and cannot control—and let go of the latter. Communicate this, though. An “I’m not the boss of you” angle can prompt a lot of people to take more personal responsibility.
- Schedule time for yourself. You might take some ideas from our previous tangentially-related article:
How To Avoid Carer Burnout (Without Dropping Care)
Want to read more?
That’s all we have space for today, but here’s a very useful page with a lot of great resources (including questionnaires and checklist and things, in case you’re thinking “is it, or…?”)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
When can my baby drink cow’s milk? It’s sooner than you think
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Parents are often faced with well-meaning opinions and conflicting advice about what to feed their babies.
The latest guidance from the World Health Organization (WHO) recommends formula-fed babies can switch to cow’s milk from six months. Australian advice says parents should wait until 12 months. No wonder some parents, and the health professionals who advise them, are confused.
So what do parents need to know about the latest advice? And when is cow’s milk an option?
What’s the updated advice?
Last year, the WHO updated its global feeding guideline for children under two years old. This included recommending babies who are partially or totally formula fed can have whole animal milks (for example, full-fat cow’s milk) from six months.
This recommendation was made after a systematic review of research by WHO comparing the growth, health and development of babies fed infant formula from six months of age with those fed pasteurised or boiled animal milks.
The review found no evidence the growth and development of babies who were fed infant formula was any better than that of babies fed whole, fresh animal milks.
The review did find an increase in iron deficiency anaemia in babies fed fresh animal milk. However, WHO noted this could be prevented by giving babies iron-rich solid foods daily from six months.
On the strength of the available evidence, the WHO recommended babies fed infant formula, alone or in addition to breastmilk, can be fed animal milk or infant formula from six months of age.
The WHO said that animal milks fed to infants could include pasteurised full-fat fresh milk, reconstituted evaporated milk, fermented milk or yoghurt. But this should not include flavoured or sweetened milk, condensed milk or skim milk.
If you’re choosing cow’s milk for your baby, make sure it’s whole milk rather than skim milk. Mr Adi/Shutterstock Why is this controversial?
Australian government guidelines recommend “cow’s milk should not be given as the main drink to infants under 12 months”. This seems to conflict with the updated WHO advice. However, WHO’s advice is targeted at governments and health authorities rather than directly at parents.
The Australian dietary guidelines are under review and the latest WHO advice is expected to inform that process.
OK, so how about iron?
Iron is an essential nutrient for everyone but it is particularly important for babies as it is vital for growth and brain development. Babies’ bodies usually store enough iron during the final few weeks of pregnancy to last until they are at least six months of age. However, if babies are born early (prematurely), if their umbilical cords are clamped too quickly or their mothers are anaemic during pregnancy, their iron stores may be reduced.
Cow’s milk is not a good source of iron. Most infant formula is made from cow’s milk and so has iron added. Breastmilk is also low in iron but much more of the iron in breastmilk is taken up by babies’ bodies than iron in cow’s milk.
Babies should not rely on milk (including infant formula) to supply iron after six months. So the latest WHO advice emphasises the importance of giving babies iron-rich solid foods from this age. These foods include:
- meat
- eggs
- vegetables, including beans and green leafy vegetables
- pulses, including lentils
- ground seeds and nuts (such as peanut or other nut butters, but with no added salt or sugar).
You may have heard that giving babies whole cow’s milk can cause allergies. In fact, whole cow’s milk is no more likely to cause allergies than infant formula based on cow’s milk.
If you’re introducing cow’s milk at six months, offer iron-rich foods too, such as meat or lentils. pamuk/Shutterstock What are my options?
The latest WHO recommendation that formula-fed babies can switch to cow’s milk from six months could save you money. Infant formula can cost more than five times more than fresh milk (A$2.25-$8.30 a litre versus $1.50 a litre).
For families who continue to use infant formula, it may be reassuring to know that if infant formula becomes hard to get due to a natural disaster or some other supply chain disruption fresh cow’s milk is fine to use from six months.
It is also important to know what has not changed in the latest feeding advice. WHO still recommends infants have only breastmilk for their first six months and then continue breastfeeding for up to two years or more. It is also still the case that infants under six months who are not breastfed or who need extra milk should be fed infant formula. Toddler formula for children over 12 months is not recommended.
All infant formula available in Australia must meet the same standard for nutritional composition and food safety. So, the cheapest infant formula is just as good as the most expensive.
What’s the take-home message?
The bottom line is your baby can safely switch from infant formula to fresh, full-fat cow’s milk from six months as part of a healthy diet with iron-rich foods. Likewise, cow’s milk can also be used to supplement or replace breastfeeding from six months, again alongside iron-rich foods.
If you have questions about introducing solids your GP, child health nurse or dietitian can help. If you need support with breastfeeding or starting solids you can call the National Breastfeeding Helpline (1800 686 268) or a lactation consultant.
Karleen Gribble, Adjunct Associate Professor, School of Nursing and Midwifery, Western Sydney University; Naomi Hull, PhD candidate, food security for infants and young children, University of Sydney, and Nina Jane Chad, Research Fellow, University of Sydney School of Public Health, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: