Speedy Easy Ratatouille
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One of the biggest contributing factors to unhealthy eating? The convenience factor. To eat well, it seems, one must have at least two of the following: money, time, and skill. So today we have a health dish that’s cheap, quick, and easy!
(You won’t need a rat in a hat to help you with this one)
You will need
- 3 ripe tomatoes, roughly chopped
- 2 zucchini, halved and chopped into thick batons
- 2 portobello mushrooms, sliced into ½” slices
- 1 large red pepper, cut into thick chunks
- 3 tbsp extra virgin olive oil
- 2 tbsp finely chopped parsley
- 2 tsp garlic paste
- 2 tsp thyme leaves, destalked
- 1 tsp rosemary leaves, destalked
- 1 tsp red chili flakes
- 1 tsp black pepper
- Optional: 1 tsp MSG, or 1 tsp low sodium salt (the MSG is the healthier option as it contains less sodium than even low sodium salt)
- Optional: other vegetables, chopped. Use what’s in your fridge! This is a great way to use up leftovers. Particularly good options include chopped eggplant, chopped red onion, and/or chopped carrot.
Method
(we suggest you read everything at least once before doing anything)
1) Put the olive oil into a sauté pan and set the heat on medium. When hot but smoking, add the mushrooms and any optional vegetables (but not the others from the list yet), and fry for 5 minutes.
Note: if you aren’t pressed for time, then you can diverge from the “speedy” part of this by cooking each of the vegetables separately before combining, which allows each to keep its flavor more distinct.
2) Add the garlic, followed by the zucchini, red pepper, chili flakes, and thyme; stir periodically (you shouldn’t have to stir constantly) for 10 minutes.
3) Add the tomatoes and a cup of water to the pan, along with any MSG/salt. Cover with the lid and allow to simmer for a further 10 minutes.
4) Serve, adding the garnish.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- The Magic Of Mushrooms: “The Longevity Vitamin” (That’s Not A Vitamin)
- Our Top 5 Spices: How Much Is Enough For Benefits? ← we had 3/5 today!
- Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk?
- MSG vs Salt: Sodium Comparison
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
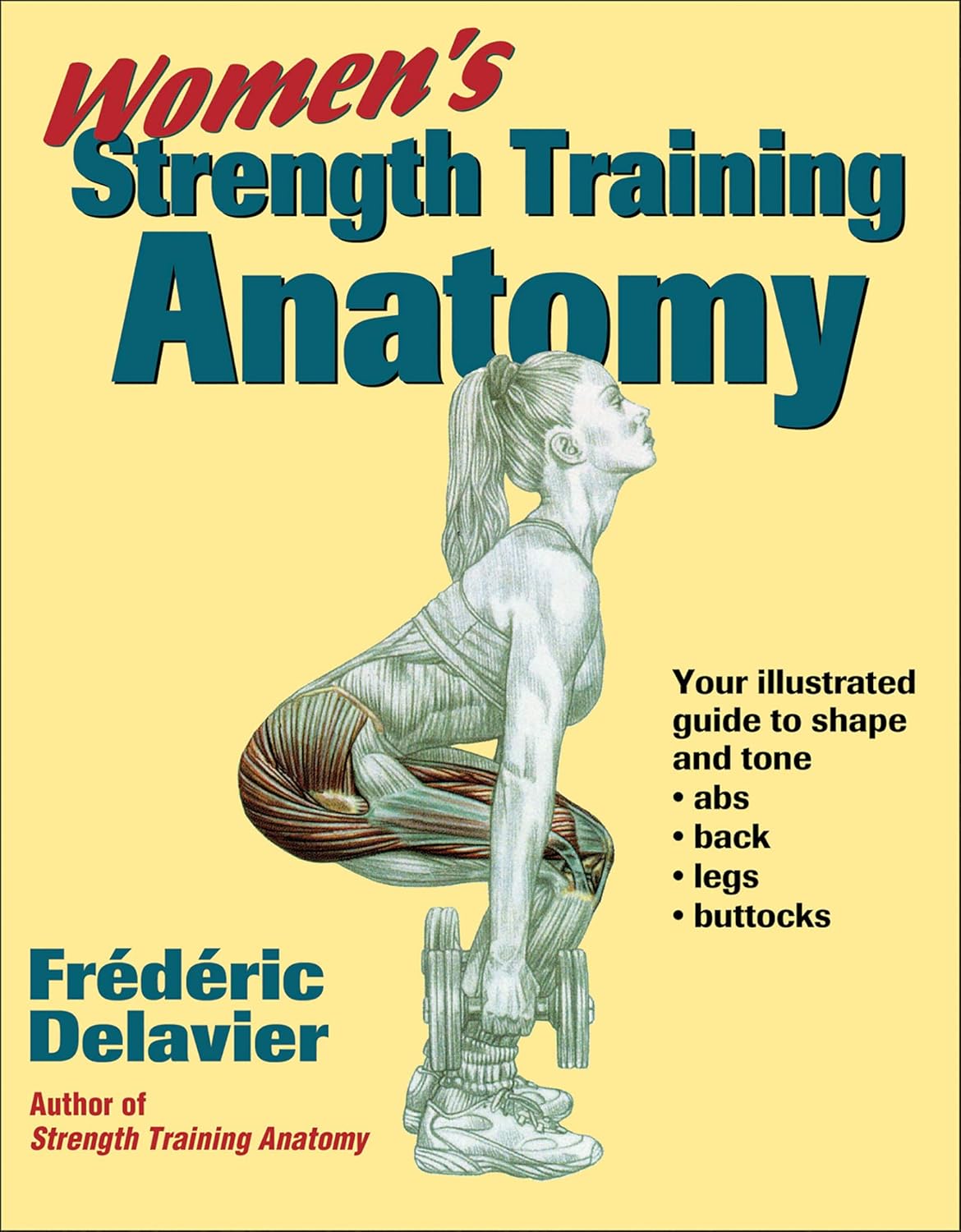
Women’s Strength Training Anatomy – by Frédéric Delavier
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fitness guides for women tend to differ from fitness guides for men, in the wrong ways:
“Do some squats and jumping jacks, and here’s a exercise for your abs; you too can look like our model here”
In those other books we are left wonder: where’s the underlying information? Where are the explanations that aren’t condescending? Where, dare we ask, is the understanding that a woman might ever lift something heavier than a baby?
Delavier, in contrast, delivers. With 130 pages of detailed anatomical diagrams for all kinds of exercises to genuinely craft your body the way you want it for you. Bigger here, smaller there, functional strength, you decide.
And rest assured: no, you won’t end up looking like Arnold Schwarzenegger unless you not only eat like him, but also have his genes (and possibly his, uh, “supplement” regime).
What you will get though, is a deep understanding of how to tailor your exercise routine to actually deliver the personalized and specific results that you want.
Pick Up Today’s Book on Amazon!
Not looking for a feminine figure? You may like the same author’s book for men:
Share This Post
-
6 Signs Of A Heart Attack… A Month In Advance
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many people know the signs of a heart attack when it’s happening, but how about before it’s too late to avoid it?
The signs
- Unusual fatigue: persistent tiredness that doesn’t improve with rest
- Shortness of breath: unexplained breathlessness during light activities or rest, which can be caused by fluid buildup in the lungs (because the heart isn’t circulating blood as well as it should)
- Chest discomfort: pain, pressure, tightness, or aching in the chest due to reduced blood flow to the heart muscle—often occurring during physical exertion or emotional stress
- Frequent indigestion: means that heartburn could be heart-related! This is about persistently reoccurring discomfort or pain in the upper abdomen
- Sleep disturbances: difficulties falling asleep, staying asleep, or waking up abruptly
- Excessive sweating: unexplained cold sweats or sudden sweating without physical exertion or excessive heat, can be a response to the decreased oxygen levels caused by less efficient blood flow
Note: this is a list of warning signs, not a diagnostic tool. Any or even all of these could be caused by something else. Just, don’t ignore the signs and do get yourself checked out.
For more details on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
-
The Epigenetics Revolution – by Dr. Nessa Carey
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you enjoyed the book “Inheritance” that we reviewed a couple of days ago, you might love this as a “next read” book. But you can also just dive straight in here, if you like!
This one, as the title suggests, focuses entirely on epigenetics—how our life events can shape our genetic expression, and that of our descendants. Or to look at it in the other direction, how our genetic expression can be shaped by the life experiences of, for example, our grandparents.
The style of this book is very much pop-science, but contains a lot of information from hard science throughout. We learn not just about longitudinal population studies as one might expect, but also about the intricacies of DNA methylation and histone modifications, for example.
Depending on your outlook, you may find some of this very bleak (“great, I am shackled by what my grandparents did”) or very optimism-inducing (“oh wow, I’m not nearly so constrained by genetics as I thought; this stuff is so malleable!”). This is also the same author who wrote “Hacking The Code of Life“, by the way, but we’ll review that another day.
Bottom line: this book is the best one-shot primer on epigenetics that this reviewer has read (you may be wondering how many that is, and the answer is… about seven or so? I’m not good at counting).
Click here to check out The Epigenetics Revolution, and learn how dynamic you really are!
Share This Post
Related Posts
-
Fix Your Upper Back With These Three Steps
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to back pain, the lower back gets a lot of attention, but what about when it’s nearer the neck and shoulders?
Reaching for better health
In this short video, Liv describes and shows three exercises:
Exercise 1: Thoracic Pullover (Dumbbell Pullover)
Purpose: Improves overhead reach and shoulder mobility.
Equipment: light weight, yoga block, or foam roller.
Steps:- Lie on the floor with the foam roller/block beneath the upper back.
- Hold the weight in both hands, arms extended upward.
- Inhale deeply and reach the weight toward the ceiling.
- Exhale and arc your spine over the block, moving the weight backward.
- Keep core tension to maintain a neutral lower back position.
- Perform 10 repetitions.
Exercise 2: Rotational Mobility Stretch
Purpose: enhances torso rotation, core strength, and hip mobility.
Equipment: none (or a mat)
Steps:- Lie on your side with knees stacked at 90° and arms extended in front.
- Hold a weight in the top hand.
- Inhale and lift the top arm toward the ceiling, extending the shoulder blade.
- Exhale and twist your torso, allowing the arm to move toward the floor.
- Modify by extending the bottom leg for a deeper twist if needed.
- Perform 6 reps per side, switching legs and repeating on the other side.
Exercise 3: Doorway/Pole Side Stretch
Purpose: targets multiple areas for a deep, satisfying stretch.
Equipment: door frame, pole, or wall.
Steps:- Stand at arm’s length from the wall or frame.
- Cross the outer leg (furthest from the wall) behind the inner leg.
- Place the closest hand on the wall and reach the other arm overhead.
- Grip the wall or frame with the top hand, pressing away with the bottom hand.
- Lean into a banana-shaped curve and rotate your chest upward for a deeper stretch.
- Hold for 20–30 seconds per side and repeat 2–3 times.
For more on all of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Minimum Method – by Joey Thurman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Trying to squeeze out an extra 0.5% from every effort in life can be exhausting, especially with diminishing marginal returns when it comes to linear increases in effort.
Surely there must be a sweet spot of getting the best returns on the least effort and call it a day?
That’s what this book is about. Thurman examines and explains how to get “the most for least” in various important areas of health, including diet, exercise, sleep, breathwork, recovery, and a chapter specifically on brain health, though of course all the aforementioned things do affect brain health too.
An interesting feature of the book is that at the end of each chapter, he’ll give different advice for different levels of experience/commitment, so that essentially there’s an easy/medium/hard way to proceed each time.
The style is light and personal, without much hard science. The advice given is nonetheless consistent with prevailing scientific consensus, and there are still occasional scientific references throughout, with links to appropriate studies. Mostly though, the focus is on being practical.
Bottom line: if you’ve been looking for a “most for least” way of going about health, this is a fine option.
Click here to check out The Minimum Method, and enjoy benefits disproportionate to your effort!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Web That Has No Weaver – by Ted Kaptchuk
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At 10almonds we have a strong “stick with the science” policy, and that means peer-reviewed studies and (where such exists) scientific consensus.
However, in the spirit of open-minded skepticism (i.e., acknowledging what we don’t necessarily know), it can be worth looking at alternatives to popular Western medicine. Indeed, many things have made their way from Traditional Chinese Medicine (or Ayurveda, or other systems) into Western medicine in any case.
“The Web That Has No Weaver” sounds like quite a mystical title, but the content is presented in the cold light of day, with constant “in Western terms, this works by…” notes.
The author walks a fine line of on the one hand, looking at where TCM and Western medicine may start and end up at the same place, by a different route; and on the other hand, noting that (in a very Daoist fashion), the route is where TCM places more of the focus, in contrast to Western medicine’s focus on the start and end.
He makes the case for TCM being more holistic, and it is, though Western medicine has been catching up in this regard since this book’s publication more than 20 years ago.
The style of the writing is very easy to follow, and is not esoteric in either mysticism or scientific jargon. There are diagrams and other illustrations, for ease of comprehension, and chapter endnotes make sure we didn’t miss important things.
Bottom line: if you’re curious about Traditional Chinese Medicine, this book is the US’s most popular introduction to such, and as such, is quite a seminal text.
Click here to check out The Web That Has No Weaver, and enjoy learning about something new!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: