Samosa Spiced Surprise
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You know what’s best about samosas? It’s not actually the fried pastry; that’s just what holds it together. If you were to try eating sheets of pastry alone, it would not be much fun. But, the spiced vegetable filling? Now we’re talking! So, this recipe takes what’s best about samosas, and makes them into healthy snack-sized patties.
You will need
- Extra virgin olive oil, or coconut oil (per your preference) for cooking
- 4 medium potatoes, boiled, peeled, and mashed
- 1 medium onion, diced
- 1 cup peas
- 1 carrot, finely chopped
- ½ cup garbanzo bean flour (chickpea flour, gram flour, whatever your supermarket calls it)
- ¼ cup fresh cilantro, chopped (substitute parsley if you have the soap gene)
- ¼ bulb garlic, minced
- 1 jalapeño pepper, chopped
- 1 tbsp ground cumin
- 2 tsp garam masala
- 1 tsp ground coriander
- 1 tsp ground turmeric
- 1 tsp ground black pepper
Method
(we suggest you read everything at least once before doing anything)
1) Fry the onion until it is becoming soft and translucent (3–5 minutes).
2) Add the spices (the garlic, both kinds of pepper, cumin, coriander, turmeric, and the garam masala), stirring in well
3) Add the carrot and peas, stirring and cooking until just becoming soft (probably another 3–5 minutes, depending on the heat, how small you chopped the carrot, and whether the peas were frozen or fresh). Take it off the heat.
4) Mix the potato, chickpea flour, and cilantro in a bowl, and carefully add everything from the pan, mixing that in thoroughly too.
5) Shape into patties, and fry them on each side until browned and crispy.
6) Serve as part of a buffet, or perhaps as an appetizer—raita is a fine accompaniment option.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Figs vs Plums – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing figs to plums, we picked the figs.
Why?
In terms of macros, figs have more protein, carbs, and fiber; the glycemic index is about equal so we’ll call this category either a tie, or a nominal win for figs (as the “more food per food” option).
In the category of vitamins, figs have more of vitamins B1, B2, B3, B5, B6, B7, B9, and choline, while plums have more of vitamins A, C, E, and K. We may subjectively prefer one set of vitamins or the other (depending on the rest of our diet, for example), but by the numbers, this is a 7:4 victory for figs.
When it comes to minerals, figs have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while plums are not higher in any minerals. An easy win for figs here.
Of course, enjoy either or both, but if you’re going to pick one for nutritional density, we say it’s figs, as illustrated scientifically below:
Want to learn more?
You might like to read:
Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Share This Post
-
Try This At Home: ABI Test For Clogged Arteries
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Arterial plaque is a big deal, and statistically it’s more of a risk as we get older, often coming to a head around age 72 for women and 65 for men—these are the median ages at which people who are going to get heart attacks, get them. Or get it, because sometimes one is all it takes.
The Ankle-Brachial Index Test
Dr. Brewer recommends a home test for detecting arterial plaque called the Ankle-Brachial Index (ABI), which uses a blood pressure monitor. The test involves measuring blood pressure in both the arms and ankles, then calculating the ratio of these measurements:
- A healthy ABI score is between 1.0 and 1.4; anything outside this range may indicate arterial problems.
- Low ABI scores (below 0.8) suggest plaque is likely obstructing blood flow
- High ABI scores (above 1.4) may indicate artery hardening
Peripheral Artery Disease (PAD), associated with poor ABI results (be they high or low), can cause a whole lot of problems that are definitely better tackled sooner rather than later—remember that atherosclerosis is a self-worsening thing once it gets going, because narrower walls means it’s even easier for more stuff to get stuck in there (and thus, the new stuff that got stuck also becomes part of the walls, and the problem gets worse).
If you need a blood pressure monitor, by the way, here’s an example product on Amazon.
Do note also that yes, if you have plaque obstructing blood flow and hardened arteries, your scores may cancel out and give you a “healthy” score, despite your arteries being very much not healthy. For this reason, this test can be used to raise the alarm, but not to give the “all clear”.
For more on all of the above, plus a demonstration and more in-depth explanation of the test, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
-
The DASH Diet Mediterranean Solution – by Dr. Marla Heller
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sometimes, an author releases a series of books that could have just been one book, with various padding and rehashes. In some cases, naming no names
Dr. Mark Hyman, it means we have to carefully pick out the honestly very good and highly recommendable ones from the “you just republished for the extra income, didn’t you?” ones.In this case, today’s book is part of a series of books with very similar titles, and this one seems the most useful as a standalone book
The Mediterranean Diet is still the scientific world’s current “gold standard” in terms of most evidence-based diet for general health, and as we’ve written about, it can be tweaked to focus on being best for [your particular concern here]. In this case, it’s the DASH variant of the Mediterranean Diet, considered best for heart health specifically.
The style is repetitive, and possibly indicative of the author getting into a habit of having to pad books. Nevertheless, saying things too often is better than forgetting to say them, so hey. On which note, it is more of an educational book than a cookbook—it does have recipes, but not many.
Bottom line: if you’d like an introduction to the DASH variant of the Mediterranean Diet, this book will get you well-acquainted.
Click here to check out The DASH Diet Mediterranean Solution, and learn all about it!
Share This Post
Related Posts
-
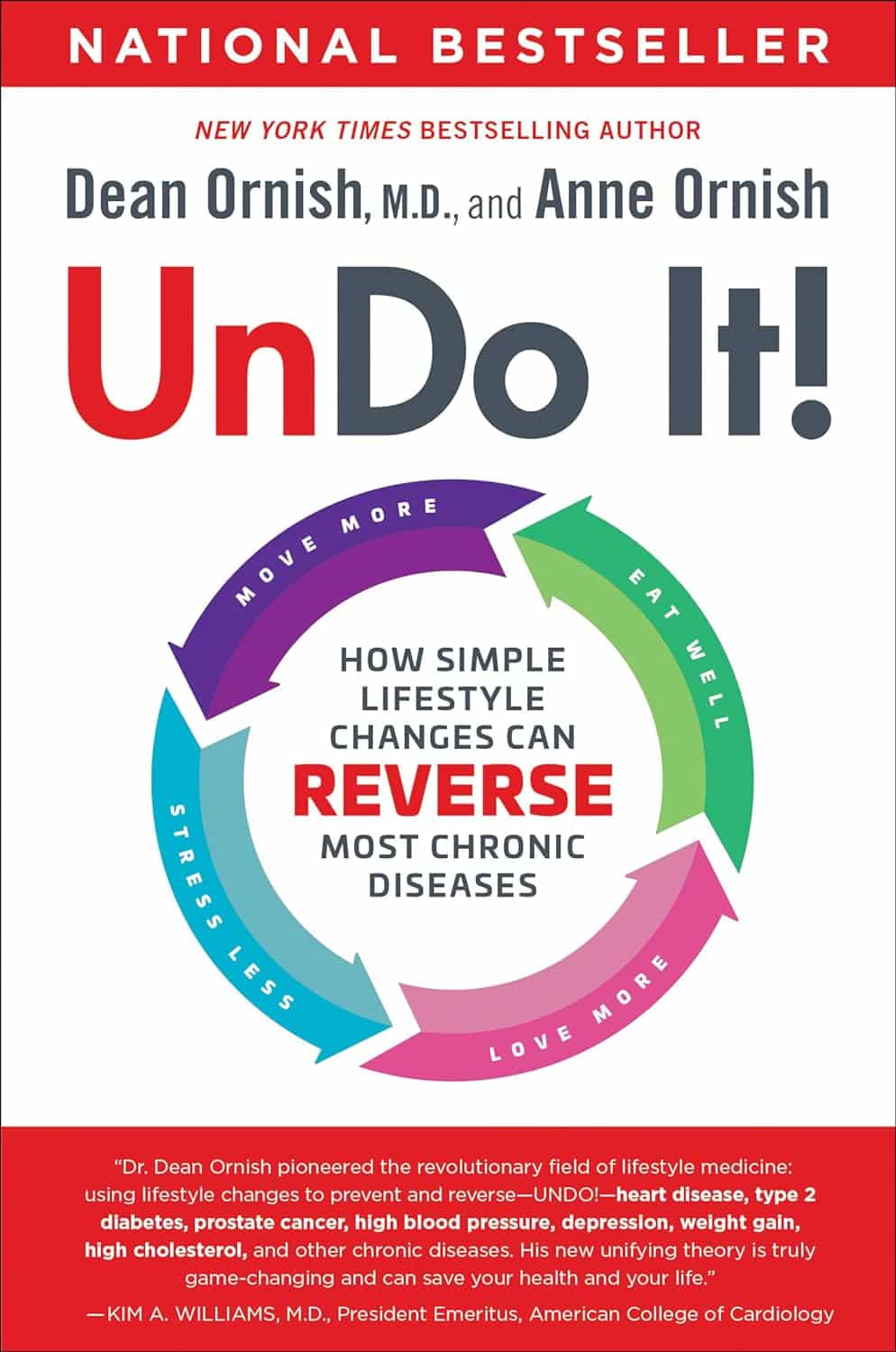
Undo It! – by Dr. Dean Ornish & Anne Ornish
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Of course, no lifestyle changes will magically undo Type 1 Diabetes or Cerebral Palsy. But for many chronic diseases, a lot can be done. The question is,how does one book cover them all?
As authors Dr. Dean Ornish and Anne Ornish explain, very many chronic diseases are exacerbated, or outright caused, by the same factors:
- Gene expression
- Inflammation
- Oxidative stress
This goes for chronic disease from heart disease to type 2 diabetes to cancer and many autoimmune diseases.
We cannot change our genes, but we can change our gene expression (the authors explain how). And certainly, we can control inflammation and oxidative stress.
Then first part of the book is given over to dietary considerations. If you’re a regular 10almonds reader, you won’t be too surprised at their recommendations, but you may enjoy the 70 recipes offered.
Attention is also given to exercising in ways optimized to beat chronic disease, and to other lifestyle factors.
Limiting stress is important, but the authors go further when it comes to psychological and sociological factors. Specifically, what matters most to health, when it comes to intimacy and community.
Bottom line: this is a very good guide to a comprehensive lifestyle overhaul, especially if something recently has given you cause to think “oh wow, I should really do more to avoid xyz disease”.
Click here to check out Undo It, and better yet, prevent it in advance!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Measles cases are rising—here’s how to protect your family
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The U.S. is currently experiencing a spike in measles cases across several states. Measles a highly contagious and potentially life-threatening disease caused by a virus. The measles-mumps-rubella (MMR) vaccine prevents measles; unvaccinated people put themselves and everyone around them at risk, including babies who are too young to receive the vaccine.
Read on to learn more about measles: what it is, how to stay protected, and what to do if a measles outbreak happens near you.
What are the symptoms of measles?
Measles symptoms typically begin 10 to 14 days after exposure. The disease starts with a fever followed by a cough, runny nose, and red eyes and then produces a rash of tiny red spots on the face and body. Measles can affect anyone, but is most serious for children under 5, immunocompromised people, and pregnant people, who may give birth prematurely or whose babies may have low birth weight as a result of a measles infection.
Measles isn’t just a rash—the disease can cause serious health problems and even death. About one in five unvaccinated people in the U.S. who get measles will be hospitalized and could suffer from pneumonia, dehydration, or brain swelling.
If you get measles, it can also damage your immune system, making you more vulnerable to other diseases.
How do you catch measles?
Measles spreads through the air when an infected person coughs or sneezes. It’s so contagious that unvaccinated people have a 90 percent chance of becoming infected if exposed.
An infected person can spread measles to others before they have symptoms.
Why are measles outbreaks happening now?
The pandemic caused many children to miss out on routine vaccinations, including the MMR vaccine. Delayed vaccination schedules coincided with declining confidence in vaccine safety and growing resistance to vaccine requirements.
Skepticism about the safety and effectiveness of COVID-19 vaccines has resulted in some people questioning or opposing the MMR vaccine and other routine immunizations.
How do I protect myself and my family from measles?
Getting an MMR vaccine is the best way to prevent getting sick with measles or spreading it to others. The CDC recommends that children receive the MMR vaccine at 12 to 15 months and again at 4 to 6 years, before starting kindergarten.
One dose of the MMR vaccine provides 93 percent protection and two doses provide 97 percent protection against all strains of measles. Because some children are too young to be immunized, it’s important that those around them are vaccinated to protect them.
Is the MMR vaccine safe?
The MMR vaccine has been rigorously tested and monitored over 50 years and determined to be safe. Adverse reactions to the vaccine are extremely rare.
Receiving the MMR vaccine is much safer than contracting measles.
What do I do if there’s a measles outbreak in my community?
Anyone who is not fully vaccinated for measles should be immunized with a measles vaccine as soon as possible. Measles vaccines given within 72 hours after exposure may prevent or reduce the severity of disease.
Children as young as 6 months old can receive the MMR vaccine if they are at risk during an outbreak. If your child isn’t fully vaccinated with two doses of the MMR vaccine—or three doses, if your child received the first dose before their first birthday—talk to your pediatrician.
Unvaccinated people who have been exposed to the virus should stay home from work, school, day care, and other activities for 21 days to avoid spreading the disease.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Marathons in Mid- and Later-Life
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
We had several requests pertaining to veganism, meatless mondays, and substitutions in recipes—so we’re going to cover those on a different day!
As for questions we’re answering today…
Q: Is there any data on immediate and long term effects of running marathons in one’s forties?
An interesting and very specific question! We didn’t find an overabundance of studies specifically for the short- and long-term effects of marathon-running in one’s 40s, but we did find a couple of relevant ones:
The first looked at marathon-runners of various ages, and found that…
- there are virtually no relevant running time differences (p<0.01) per age in marathon finishers from 20 to 55 years
- the majority of middle-aged and elderly athletes have training histories of less than seven years of running
From which they concluded:
❝The present findings strengthen the concept that considers aging as a biological process that can be considerably speeded up or slowed down by multiple lifestyle related factors.❞
See the study: Performance, training and lifestyle parameters of marathon runners aged 20–80 years: results of the PACE-study
The other looked specifically at the impact of running on cartilage, controlled for age (45 and under vs 46 and older) and activity level (marathon-runners vs sedentary people).
The study had the people, of various ages and habitual activity levels, run for 30 minutes, and measured their knee cartilage thickness (using MRI) before and after running.
They found that regardless of age or habitual activity level, running compressed the cartilage tissue to a similar extent. From this, it can be concluded that neither age nor marathon-running result in long-term changes to cartilage response to running.
Or in lay terms: there’s no reason that marathon-running at 40 should ruin your knees (unless you are doing something wrong).
That may or may not have been a concern you have, but it’s what the study looked at, so hey, it’s information.
Here’s the study: Functional cartilage MRI T2 mapping: evaluating the effect of age and training on knee cartilage response to running
Q: Information on [e-word] dysfunction for those who have negative reactions to [the most common medications]?
When it comes to that particular issue, one or more of these three factors are often involved:
- Hormones
- Circulation
- Psychology
The most common drugs (that we can’t name here) work on the circulation side of things—specifically, by increasing the localized blood pressure. The exact mechanism of this drug action is interesting, albeit beyond the scope of a quick answer here today. On the other hand, the way that they work can cause adverse blood-pressure-related side effects for some people; perhaps you’re one of them.
To take matters into your own hands, so to speak, you can address each of those three things we just mentioned:
Hormones
Ask your doctor (or a reputable phlebotomy service) for a hormone test. If your free/serum testosterone levels are low (which becomes increasingly common in men over the age of 45), they may prescribe something—such as testosterone shots—specifically for that.
This way, it treats the underlying cause, rather than offering a workaround like those common pills whose names we can’t mention here.
Circulation
Look after your heart health; eat for your heart health, and exercise regularly!
Cold showers/baths also work wonders for vascular tone—which is precisely what you need in this matter. By rapidly changing temperatures (such as by turning off the hot water for the last couple of minutes of your shower, or by plunging into a cold bath), your blood vessels will get practice at constricting and maintaining that constriction as necessary.
Psychology
[E-word] dysfunction can also have a psychological basis. Unfortunately, this can also then be self-reinforcing, if recalling previous difficulties causes you to get distracted/insecure and lose the moment. One of the best things you can do to get out of this catch-22 situation is to not worry about it in the moment. Depending on what you and your partner(s) like to do in bed, there are plenty of other equally respectable options, so just switch track!
Having a conversation about this in advance will probably be helpful, so that everyone’s on the same page of the script in that eventuality, and it becomes “no big deal”. Without that conversation, misunderstandings and insecurities could arise for your partner(s) as well as yourself (“aren’t I desirable enough?” etc).
So, to recap, we recommend:
- Have your hormones checked
- Look after your circulation
- Make the decision to have fun!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: