Sometimes, Perfect Isn’t Practical!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝10 AM breakfast is not realistic for most. What’s wrong with 8 AM and Evening me at 6. Don’t quite understand the differentiation.❞
(for reference, this is about our “Breakfasting For Health?” main feature)
It’s not terrible to do it the way you suggest It’s just not optimal, either, that’s all!
Breakfasting at 08:00 and then dining at 18:00 is ten hours apart, so no fasting benefits between those. Let’s say you take half an hour to eat dinner, then eat nothing again until breakfast, that’s 18:30 to 08:00, so that’s 13½ hours fasting. You’ll recall that fasting benefits start at 12 hours into the fast, so that means you’d only get 1½ hours of fasting benefits.
As for breakfasting at 08:00 regardless of intermittent fasting considerations, the reason for the conclusion of around 10:00 being optimal, is based on when our body is geared up to eat breakfast and get the most out of that, which the body can’t do immediately upon waking. So if you wake and get sunlight at 08:30, get a little moderate exercise, then by 10:00 your digestive system will be perfectly primed to get the most out of breakfast.
However! This is entirely based on you waking and getting sunlight at 08:30.
So, iff you wake and get sunlight at 06:30, then in that case, breakfasting at 08:00 would give the same benefits as described above. What’s important is the 1½ hour priming-time.
Writer’s note: our hope here is always to be informational, not prescriptive. Take what works for you; ignore what doesn’t fit your lifestyle.
I personally practice intermittent fasting for about 21hrs/day. I breakfast (often on nuts and perhaps a little salad) around 16:00, and dine at around 18:00ish, giving myself a little wiggleroom. I’m not religious about it and will slide it if necessary.
As you can see: that makes what is nominally my breakfast practically a pre-dinner snack, and I clearly ignore the “best to eat in the morning” rule because that’s not consistent with my desire to have a family dinner together in the evening while still practicing the level of fasting that I prefer.
Science is science, and that’s what we report here. How we apply it, however, is up to us all as individuals!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
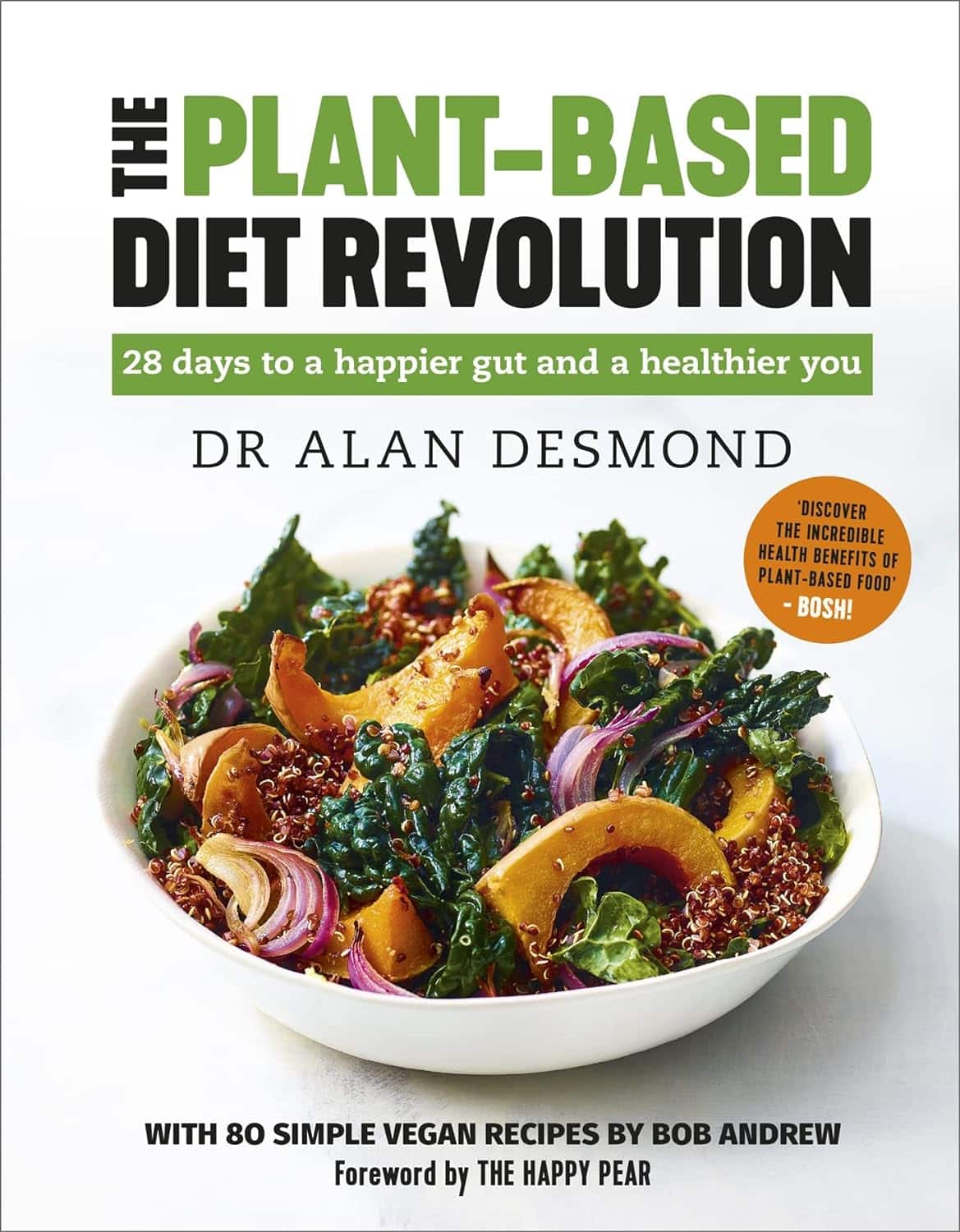
The Plant-Based Diet Revolution – by Dr. Alan Desomond
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is this just another gut-healthy cooking guide? Not entirely…
For a start, it’s not just about giving you a healthy gut; it also covers a healthy heart and a healthy brain. There’s lots of science in here!
It’s also aimed as a transitional guide to eating more plants and fewer animal products, if you so choose. And if you don’t so choose, at least having the flexibility to cook both ways.
The recipes themselves (organized into basics, breakfasts, lunches, mains, desserts) are clear and easy while also being calculated to please readers (and their families) who are used to eating more meat. There are, for instance, plenty of healthy proteins, healthy fats, and comfort foods.
The “28 days” of the title refers to a meal plan using the recipes from the book; it’s not a big feature of the book though, so use it or don’t, but the cooking advice itself is more than worth the price of the book and the recipes are certainly great.
Bottom line: if you’re thinking of taking a “Meatless Mondays” approach to making your diet healthier, this book can help you do that in style!
Click here to check out The Plant-Based Diet Revolution, and upgrade your culinary repertoire!
Share This Post
-
What Weston Price Got Right (And Wrong)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Weston Price: What Stood The Test of Time?
This is Dr. Weston Price, a dentist. You may guess from the photo, or perhaps already knew, his work is not new in 2023. We usually feature current health experts here, but we’re taking a day to do a blast from the past, because his ideas endure today, and inform a lot of people’s health views. So, he’s a good one to at least know about.
What was his deal?
Dr. Price (1870–1948) wanted to study focal infection theory—the idea that repairing root canals allowed bacterial infections that caused everything from heart disease to arthritis. His solution was that the teeth should be extracted instead.
This theory was popular in the 1920s, was challenged in the 1930s, ignored in the 1940s (the world was a bit busy), and by broad medical consensus anyway, rejected in the 1950s. But, while it was being challenged in the 1930s, Dr. Price decided to find more evidence for its support.
The result was his famous world tour of peoples living traditional lifestyles without the influence of “modern” diet. His findings, and the conclusions he drew from them, extended to far more than just dental health.
What did he find?
Dr. Price found that people living traditional lifestyles, with their traditional diets based on locally-sourced foods, had much better overall health. Of course, he was a dentist and not a general practitioner, so aside from examining their teeth, he largely relied on self-reported diagnoses of illness, or lack thereof.
In short: he found that people in places without modern medical institutions had fewer diagnoses of disease. From this, he concluded that incidence of disease was much lower.
There was also an unexamined element of survivorship bias—an undiagnosed disease is more likely to be fatal, and he questioned only living people, which skewed the stats rather. Nor did he examine infant mortality rate nor adult life expectancy, both of which were not great.
Was it all useless, then?
Actually no! He did hit upon some observations that have stood the test of time:
- He correctly concluded that modern diets with sugar and white flour were ruinous to the health.
- He correctly concluded that locally-sourced food, and grass-fed in the case of pastoral farming, tended to have much more nutritional value than the mass-produced results of intensive farming.
- He correctly concluded that many modern preservation methods robbed foods of their nutrients.
- He correctly concluded that many grains and seeds are more nutritions when fermented/soaked/sprouted.
About that “locally-sourced food”: the reason locally-sourced food tends to be more nutritious is that it has required less in the way of preservation for a long trip around the world, and will also tend to be fresher.
On the other hand, this does mean a lot of the foods that Dr. Price recommends are very much subject to availability. It may well be true that the Inuit people do not eat a lot of fruit and veg (which mostly do not grow there), but if you live in Nevada, maybe locally-sourced whale fat is just as difficult to find.
One person’s “this fatty organ meat contains the vitamin C we need” may be another person’s “that’s great; I have an apple tree in my garden though”.
Want to learn more?
Dr. Price’s most influential work is his magnum opus, “Nutrition and Physical Degeneration”. It’s a fascinating book in its historical context, but do be warned, it was written by a rich white man in 1939 and the writing is as racist as you might expect. Even when making favourable comparisons, the tone is very much “and here is what these savages are doing well”.
If you don’t fancy reading all that, here are two other sources about Weston Price’s work and conclusions, presented for balance:
- The Weston A. Price Foundation (Official Website)
- Weston Price’s Appalling Legacy (Science-Based Medicine.org)
Enjoy!
Share This Post
-
Bird Flu Is Bad for Poultry and Dairy Cows. It’s Not a Dire Threat for Most of Us — Yet.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Headlines are flying after the Department of Agriculture confirmed that the H5N1 bird flu virus has infected dairy cows around the country. Tests have detected the virus among cattle in nine states, mainly in Texas and New Mexico, and most recently in Colorado, said Nirav Shah, principal deputy director at the Centers for Disease Control and Prevention, at a May 1 event held by the Council on Foreign Relations.
A menagerie of other animals have been infected by H5N1, and at least one person in Texas. But what scientists fear most is if the virus were to spread efficiently from person to person. That hasn’t happened and might not. Shah said the CDC considers the H5N1 outbreak “a low risk to the general public at this time.”
Viruses evolve and outbreaks can shift quickly. “As with any major outbreak, this is moving at the speed of a bullet train,” Shah said. “What we’ll be talking about is a snapshot of that fast-moving train.” What he means is that what’s known about the H5N1 bird flu today will undoubtedly change.
With that in mind, KFF Health News explains what you need to know now.
Q: Who gets the bird flu?
Mainly birds. Over the past few years, however, the H5N1 bird flu virus has increasingly jumped from birds into mammals around the world. The growing list of more than 50 species includes seals, goats, skunks, cats, and wild bush dogs at a zoo in the United Kingdom. At least 24,000 sea lions died in outbreaks of H5N1 bird flu in South America last year.
What makes the current outbreak in cattle unusual is that it’s spreading rapidly from cow to cow, whereas the other cases — except for the sea lion infections — appear limited. Researchers know this because genetic sequences of the H5N1 viruses drawn from cattle this year were nearly identical to one another.
The cattle outbreak is also concerning because the country has been caught off guard. Researchers examining the virus’s genomes suggest it originally spilled over from birds into cows late last year in Texas, and has since spread among many more cows than have been tested. “Our analyses show this has been circulating in cows for four months or so, under our noses,” said Michael Worobey, an evolutionary biologist at the University of Arizona in Tucson.
Q: Is this the start of the next pandemic?
Not yet. But it’s a thought worth considering because a bird flu pandemic would be a nightmare. More than half of people infected by older strains of H5N1 bird flu viruses from 2003 to 2016 died. Even if death rates turn out to be less severe for the H5N1 strain currently circulating in cattle, repercussions could involve loads of sick people and hospitals too overwhelmed to handle other medical emergencies.
Although at least one person has been infected with H5N1 this year, the virus can’t lead to a pandemic in its current state. To achieve that horrible status, a pathogen needs to sicken many people on multiple continents. And to do that, the H5N1 virus would need to infect a ton of people. That won’t happen through occasional spillovers of the virus from farm animals into people. Rather, the virus must acquire mutations for it to spread from person to person, like the seasonal flu, as a respiratory infection transmitted largely through the air as people cough, sneeze, and breathe. As we learned in the depths of covid-19, airborne viruses are hard to stop.
That hasn’t happened yet. However, H5N1 viruses now have plenty of chances to evolve as they replicate within thousands of cows. Like all viruses, they mutate as they replicate, and mutations that improve the virus’s survival are passed to the next generation. And because cows are mammals, the viruses could be getting better at thriving within cells that are closer to ours than birds’.
The evolution of a pandemic-ready bird flu virus could be aided by a sort of superpower possessed by many viruses. Namely, they sometimes swap their genes with other strains in a process called reassortment. In a study published in 2009, Worobey and other researchers traced the origin of the H1N1 “swine flu” pandemic to events in which different viruses causing the swine flu, bird flu, and human flu mixed and matched their genes within pigs that they were simultaneously infecting. Pigs need not be involved this time around, Worobey warned.
Q: Will a pandemic start if a person drinks virus-contaminated milk?
Not yet. Cow’s milk, as well as powdered milk and infant formula, sold in stores is considered safe because the law requires all milk sold commercially to be pasteurized. That process of heating milk at high temperatures kills bacteria, viruses, and other teeny organisms. Tests have identified fragments of H5N1 viruses in milk from grocery stores but confirm that the virus bits are dead and, therefore, harmless.
Unpasteurized “raw” milk, however, has been shown to contain living H5N1 viruses, which is why the FDA and other health authorities strongly advise people not to drink it. Doing so could cause a person to become seriously ill or worse. But even then, a pandemic is unlikely to be sparked because the virus — in its current form — does not spread efficiently from person to person, as the seasonal flu does.
Q: What should be done?
A lot! Because of a lack of surveillance, the U.S. Department of Agriculture and other agencies have allowed the H5N1 bird flu to spread under the radar in cattle. To get a handle on the situation, the USDA recently ordered all lactating dairy cattle to be tested before farmers move them to other states, and the outcomes of the tests to be reported.
But just as restricting covid tests to international travelers in early 2020 allowed the coronavirus to spread undetected, testing only cows that move across state lines would miss plenty of cases.
Such limited testing won’t reveal how the virus is spreading among cattle — information desperately needed so farmers can stop it. A leading hypothesis is that viruses are being transferred from one cow to the next through the machines used to milk them.
To boost testing, Fred Gingrich, executive director of a nonprofit organization for farm veterinarians, the American Association of Bovine Practitioners, said the government should offer funds to cattle farmers who report cases so that they have an incentive to test. Barring that, he said, reporting just adds reputational damage atop financial loss.
“These outbreaks have a significant economic impact,” Gingrich said. “Farmers lose about 20% of their milk production in an outbreak because animals quit eating, produce less milk, and some of that milk is abnormal and then can’t be sold.”
The government has made the H5N1 tests free for farmers, Gingrich added, but they haven’t budgeted money for veterinarians who must sample the cows, transport samples, and file paperwork. “Tests are the least expensive part,” he said.
If testing on farms remains elusive, evolutionary virologists can still learn a lot by analyzing genomic sequences from H5N1 viruses sampled from cattle. The differences between sequences tell a story about where and when the current outbreak began, the path it travels, and whether the viruses are acquiring mutations that pose a threat to people. Yet this vital research has been hampered by the USDA’s slow and incomplete posting of genetic data, Worobey said.
The government should also help poultry farmers prevent H5N1 outbreaks since those kill many birds and pose a constant threat of spillover, said Maurice Pitesky, an avian disease specialist at the University of California-Davis.
Waterfowl like ducks and geese are the usual sources of outbreaks on poultry farms, and researchers can detect their proximity using remote sensing and other technologies. By zeroing in on zones of potential spillover, farmers can target their attention. That can mean routine surveillance to detect early signs of infections in poultry, using water cannons to shoo away migrating flocks, relocating farm animals, or temporarily ushering them into barns. “We should be spending on prevention,” Pitesky said.
Q: OK it’s not a pandemic, but what could happen to people who get this year’s H5N1 bird flu?
No one really knows. Only one person in Texas has been diagnosed with the disease this year, in April. This person worked closely with dairy cows, and had a mild case with an eye infection. The CDC found out about them because of its surveillance process. Clinics are supposed to alert state health departments when they diagnose farmworkers with the flu, using tests that detect influenza viruses, broadly. State health departments then confirm the test, and if it’s positive, they send a person’s sample to a CDC laboratory, where it is checked for the H5N1 virus, specifically. “Thus far we have received 23,” Shah said. “All but one of those was negative.”
State health department officials are also monitoring around 150 people, he said, who have spent time around cattle. They’re checking in with these farmworkers via phone calls, text messages, or in-person visits to see if they develop symptoms. And if that happens, they’ll be tested.
Another way to assess farmworkers would be to check their blood for antibodies against the H5N1 bird flu virus; a positive result would indicate they might have been unknowingly infected. But Shah said health officials are not yet doing this work.
“The fact that we’re four months in and haven’t done this isn’t a good sign,” Worobey said. “I’m not super worried about a pandemic at the moment, but we should start acting like we don’t want it to happen.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
Related Posts
-
What is childhood dementia? And how could new research help?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Childhood” and “dementia” are two words we wish we didn’t have to use together. But sadly, around 1,400 Australian children and young people live with currently untreatable childhood dementia.
Broadly speaking, childhood dementia is caused by any one of more than 100 rare genetic disorders. Although the causes differ from dementia acquired later in life, the progressive nature of the illness is the same.
Half of infants and children diagnosed with childhood dementia will not reach their tenth birthday, and most will die before turning 18.
Yet this devastating condition has lacked awareness, and importantly, the research attention needed to work towards treatments and a cure.
More about the causes
Most types of childhood dementia are caused by mutations (or mistakes) in our DNA. These mistakes lead to a range of rare genetic disorders, which in turn cause childhood dementia.
Two-thirds of childhood dementia disorders are caused by “inborn errors of metabolism”. This means the metabolic pathways involved in the breakdown of carbohydrates, lipids, fatty acids and proteins in the body fail.
As a result, nerve pathways fail to function, neurons (nerve cells that send messages around the body) die, and progressive cognitive decline occurs.
Childhood dementia is linked to rare genetic disorders. maxim ibragimov/Shutterstock What happens to children with childhood dementia?
Most children initially appear unaffected. But after a period of apparently normal development, children with childhood dementia progressively lose all previously acquired skills and abilities, such as talking, walking, learning, remembering and reasoning.
Childhood dementia also leads to significant changes in behaviour, such as aggression and hyperactivity. Severe sleep disturbance is common and vision and hearing can also be affected. Many children have seizures.
The age when symptoms start can vary, depending partly on the particular genetic disorder causing the dementia, but the average is around two years old. The symptoms are caused by significant, progressive brain damage.
Are there any treatments available?
Childhood dementia treatments currently under evaluation or approved are for a very limited number of disorders, and are only available in some parts of the world. These include gene replacement, gene-modified cell therapy and protein or enzyme replacement therapy. Enzyme replacement therapy is available in Australia for one form of childhood dementia. These therapies attempt to “fix” the problems causing the disease, and have shown promising results.
Other experimental therapies include ones that target faulty protein production or reduce inflammation in the brain.
Research attention is lacking
Death rates for Australian children with cancer nearly halved between 1997 and 2017 thanks to research that has enabled the development of multiple treatments. But over recent decades, nothing has changed for children with dementia.
In 2017–2023, research for childhood cancer received over four times more funding per patient compared to funding for childhood dementia. This is despite childhood dementia causing a similar number of deaths each year as childhood cancer.
The success for childhood cancer sufferers in recent decades demonstrates how adequately funding medical research can lead to improvements in patient outcomes.
Dementia is not just a disease of older people. Miljan Zivkovic/Shutterstock Another bottleneck for childhood dementia patients in Australia is the lack of access to clinical trials. An analysis published in March this year showed that in December 2023, only two clinical trials were recruiting patients with childhood dementia in Australia.
Worldwide however, 54 trials were recruiting, meaning Australian patients and their families are left watching patients in other parts of the world receive potentially lifesaving treatments, with no recourse themselves.
That said, we’ve seen a slowing in the establishment of clinical trials for childhood dementia across the world in recent years.
In addition, we know from consultation with families that current care and support systems are not meeting the needs of children with dementia and their families.
New research
Recently, we were awarded new funding for our research on childhood dementia. This will help us continue and expand studies that seek to develop lifesaving treatments.
More broadly, we need to see increased funding in Australia and around the world for research to develop and translate treatments for the broad spectrum of childhood dementia conditions.
Dr Kristina Elvidge, head of research at the Childhood Dementia Initiative, and Megan Maack, director and CEO, contributed to this article.
Kim Hemsley, Head, Childhood Dementia Research Group, Flinders Health and Medical Research Institute, College of Medicine and Public Health, Flinders University; Nicholas Smith, Head, Paediatric Neurodegenerative Diseases Research Group, University of Adelaide, and Siti Mubarokah, Research Associate, Childhood Dementia Research Group, Flinders Health and Medical Research Institute, College of Medicine and Public Health, Flinders University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Anti-Viral Gut – by Dr. Robynne Chutkan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Some people get a virus and feel terrible for a few days; other people get the same virus and die. Then there are some who never even get it at all despite being in close proximity with the other two. So, what’s the difference?
Dr. Robynne Chutkan outlines the case for the difference not being in the virus, but in the people. And nor is it a matter of mysterious fate, but rather, a matter of the different levels of defenses (or lack thereof) that we each have.
The key, she explains, is in our microbiome, and the specific steps to make sure that ours is optimized and ready to protect us. The book goes beyond “eat prebiotics and probiotics”, though, and goes through other modifiable factors, based on data from this pandemic and the last one a hundred years ago. We also learn about the many different kinds of bacteria that live in our various body parts (internal and external), because as it turns out, our gut microbiome (however important; hence the title) isn’t the only relevant microbiome when it comes to whether or not a given disease will take hold or be eaten alive on the way in.
The style is very polished—Dr. Chutkan is an excellent educator who makes her points clearly and comprehensibly without skimping on scientific detail.
Bottom line: if you’d like your chances of surviving any given virus season to not be left to chance, then this is a must-read book.
Click here to check out The Anti-Viral Gut, and make your body a fortress!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
STI rates are increasing among midlife and older adults. We need to talk about it
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Globally, the rates of common sexually transmissible infections (STIs) are increasing among people aged over 50. In some cases, rates are rising faster than among younger people.
Recent data from the United States Centers for Disease Control and Prevention shows that, among people aged 55 and older, rates of gonorrhoea and chlamydia, two of the most common STIs, more than doubled between 2012 and 2022.
Australian STI surveillance data has reflected similar trends. Between 2013 and 2022, there was a steady increase in diagnoses of chlamydia, gonorrhoea and syphilis among people aged 40 and older. For example, there were 5,883 notifications of chlamydia in Australians 40 plus in 2013, compared with 10,263 in 2022.
A 2020 study of Australian women also showed that, between 2000 and 2018, there was a sharper increase in STI diagnoses among women aged 55–74 than among younger women.
While the overall rate of common STIs is highest among young adults, the significant increase in STI diagnoses among midlife and older adults suggests we need to pay more attention to sexual health across the life course.
Fit Ztudio/Shutterstock Why are STI rates rising among older adults?
STI rates are increasing globally for all age groups, and an increase among midlife and older people is in line with this trend.
However, increases of STIs among older people are likely due to a combination of changing sex and relationship practices and hidden sexual health needs among this group.
The “boomer” generation came of age in the 60s and 70s. They are the generation of free love and their attitude to sex, even as they age, is quite different to that of generations before them.
Given the median age of divorce in Australia is now over 43, and the internet has ushered in new opportunities for post-separation dating, it’s not surprising that midlife and older adults are exploring new sexual practices or finding multiple sexual partners.
People may start new relationships later in life. Tint Media/Shutterstock It’s also possible midlife and older people have not had exposure to sexual health education in school or do not relate to current safe sex messages, which tend to be directed toward young people. Condoms may therefore seem unnecessary for people who aren’t trying to avoid pregnancy. Older people may also lack confidence negotiating safe sex or accessing STI screening.
Hidden sexual health needs
In contemporary life, the sex lives of older adults are largely invisible. Ageing and older bodies are often associated with loss of power and desirability, reflected in the stereotype of older people as asexual and in derogatory jokes about older people having sex.
With some exceptions, we see few positive representations of older sexual bodies in film or television.
Older people’s sexuality is also largely invisible in public policy. In a review of Australian policy relating to sexual and reproductive health, researchers found midlife and older adults were rarely mentioned.
Sexual health policy generally targets groups with the highest STI rates, which excludes most older people. As midlife and older adults are beyond childbearing years, they also do not feature in reproductive health policy. This means there is a general absence of any policy related to sex or sexual health among midlife or older adults.
Added to this, sexual health policy tends to be focused on risk rather than sexual wellbeing. Sexual wellbeing, including freedom and capacity to pursue pleasurable sexual experiences, is strongly associated with overall health and quality of life for adults of all ages. Including sexual wellbeing as a policy priority would enable a focus on safe and respectful sex and relationships across the adult life course.
Without this priority, we have limited knowledge about what supports sexual wellbeing as people age and limited funding for initiatives to engage with midlife or older adults on these issues.
Midlife and older adults may have limited knowledge about STIs. Southworks/Shutterstock How can we support sexual health and wellbeing for older adults?
Most STIs are easily treatable. Serious complications can occur, however, when STIs are undiagnosed and untreated over a long period. Untreated STIs can also be passed on to others.
Late diagnosis is not uncommon as some STIs can have no symptoms and many people don’t routinely screen for STIs. Older, heterosexual adults are, in general, less likely than other groups to seek regular STI screening.
For midlife or older adults, STIs may also be diagnosed late because some doctors do not initiate testing due to concerns they will cause offence or because they assume STI risk among older people is negligible.
Many doctors are reluctant to discuss sexual health with their older patients unless the patient explicitly raises the topic. However, older people can be embarrassed or feel awkward raising matters of sex.
Resources for health-care providers and patients to facilitate conversations about sexual health and STI screening with older patients would be a good first step.
To address rising rates of STIs among midlife and older adults, we also need to ensure sexual health promotion is targeted toward these age groups and improve accessibility of clinical services.
More broadly, it’s important to consider ways to ensure sexual wellbeing is prioritised in policy and practice related to midlife and older adulthood.
A comprehensive approach to older people’s sexual health, that explicitly places value on the significance of sex and intimacy in people’s lives, will enhance our ability to more effectively respond to sexual health and STI prevention across the life course.
Jennifer Power, Associate Professor and Principal Research Fellow, Australian Research Centre in Sex, Health and Society, La Trobe University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: