Powered by Plants – by Ocean Robbins & Nichole Dandrea-Russert
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Of the two authors, the former is a professional public speaker, and the latter is a professional dietician. As a result, we get a book that is polished and well-presented, while actually having a core of good solid science (backed up with plenty of references).
There’s an introductory section that’s all about the “notable nutrients”, that will be focused on in the ingredients choices for the recipes in the rest of the book.
The recipes themselves are simple enough to do quickly, yet interesting enough that you’ll want to do them, and certainly they contain all the plant-based nutrient-density you might expect.
Bottom line: if you’d like to expand your plant-based cooking with a focus on nutrition and ease without sacrificing fun, then this is a great cookbook for that.
Click here to check out Powered by Plants, and get powered by plants!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
For tennis star Destanee Aiava, borderline personality disorder felt like ‘a death sentence’ – and a relief. What is it?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Last week, Australian Open player Destanee Aiava revealed she had struggled with borderline personality disorder.
The tennis player said a formal diagnosis, after suicidal behaviour and severe panic attacks, “was a relief”. But “it also felt like a death sentence because it’s something that I have to live with my whole life”.
A diagnosis is often associated with therapeutic nihilism. This means it’s viewed as impossible to treat, and can leave clinicians and people with the condition in despair.
In fact, people with this disorder can and do recover with adequate support. Understanding it is caused by trauma is fundamental to effectively treat this complex and poorly understood mental illness.
A stigmatising diagnosis
The name “borderline personality disorder” is confusing and adds greatly to the stigma around it.
Doctors first used “borderline” to describe a condition they believed was in-between two others: neurosis and psychosis.
But this implies the condition is not real in itself, and can invalidate the suffering and distress the person and their loved ones experience.
“Personality disorder” is a judgemental term that describes the very essence of a person – their personality – as flawed.
What is borderline personality disorder?
People with the disorder can express a range of symptoms, but high levels of anxiety – including panic attacks – are usually constant.
Symptoms cluster around four main areas:
- high impulsivity (leading to suicidal thoughts and behaviour, self-harm and other risky behaviours)
- unstable or poor sense of self (including low self-esteem)
- mood disturbances (including intense, inappropriate anger, episodic depression or mania)
- problems in relationships.
People with the disorder greatly fear being abandoned and as a result, commonly have distressing difficulties in interpersonal relationships.
This creates a “push-pull” dynamic with loved ones, as people with borderline personality disorder seek closeness, but push away those they love to test the strength of the relationship.
For example, they may escalate a small issue into a major disagreement to see if the loved one will “stick with them” and reinforce their love.
Conversely, if a loved one appears distant or fed up – for example, is thinking about ending the relationship – the person with borderline personality disorder will make major efforts to “pull” them back. This might look like a flurry of messages, expressions of despair, or even suicidal behaviours.
People with borderline personality disorder greatly fear being abandoned, making relationship issues common. Drazen Zigic/Shutterstock Who does it affect?
The disorder affects one in 100 Australians, although this is likely a conservative estimate, as diagnosis is based on the most severe symptoms.
Women are much more likely to be diagnosed with it than men – but why this is so remains a major debate, with political and sociological factors playing a role in making psychiatric diagnoses. Symptoms usually begin in the mid to late teens.
While an initial response to receiving a diagnosis can be comforting for some, it is commonly seen as a chronic, relapsing condition, meaning symptoms can return after a period of improvement.
Borderline personality disorder can fluctuate in intensity and mimic other conditions such as major depression, bipolar disorder, anxiety disorders and psychosis.
Estimates suggest 26% of presentations at emergency departments for mental health issues are by people diagnosed with personality disorders, particularly borderline personality disorder.
What causes it?
The main cause for borderline personality disorder appears to be trauma in early life, compounded by repeated traumas later.
Early life trauma can lead to biological changes in the brain that cause behavioural, emotional or cognitive shifts, leading to social and relationship issues. This is known as complex post-traumatic stress disorder.
Aiava has acknowledged the disorder is “mainly from childhood trauma”, although she has not given details about her specific experiences.
People with borderline personality disorder usually have complex post-traumatic stress disorder. But complex post-traumatic stress disorder doesn’t always result in a borderline personality disorder diagnosis.
Although the two disorders are not identical, they share many similarities, in particular that they are both caused by complex and repeated trauma.
However those with borderline personality disorder tend to experience more rage, emotional disturbances and have a greater fear of abandonment.
They also face greater stigma, whereas the term “complex post-traumatic stress disorder” doesn’t carry the same negative connotations and focuses on the cause of the condition – trauma – rather than “personality”, leading to better treatment options.
The recognition of the major role of trauma in borderline personality disorder is an important step forward in treating the disorder. But because of the stigma associated with it, using the diagnosis of complex post-traumatic stress disorder maybe a better step forward in the future.
Can it be treated?
There are many effective psychological therapies and other treatments for people with borderline personality disorder or complex post-traumatic stress disorder.
For example, dialectical behavioural therapy is a type of cognitive therapy that helps people learn skills such as tolerating distress, managing relationships, regulating emotions and practising mindfulness.
The treatment of people with post-traumatic stress disorder, including victims of war and rape, has taught us a lot about how to treat complex, underlying trauma. For example, with trauma-focused psychological therapies.
Other new treatments, such as eye movement desensitisation and reprogramming, have also shown to be effective.
Many people with borderline personality disorder who receive treatment and have supportive relationships are able to “outgrow” the condition. Others may need to continue to manage symptoms while pursuing a good quality of life.
Treating trauma, not personality
Rethinking borderline personality disorder as a trauma disorder enables a more effective and understanding approach for those with it.
Understanding what trauma does to the brain means newer, targeted medications can also be used.
For example, our research has shown how the brain’s glutamate system – the chemicals responsible for learning and making sense of one’s environment – is overactive in people with complex post-traumtic stress disorder. Medications that work on the glutumate system may therefore help alleviate borderline personality disorder symptoms.
Educating partners and families about borderline personality disorder, providing them support and co-designing crisis strategies are also important parts of total care. Preventing early life trauma is also critical.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
Jayashri Kulkarni, Professor of Psychiatry, Monash University and Eveline Mu, Research Fellow in Women’s Mental Health, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
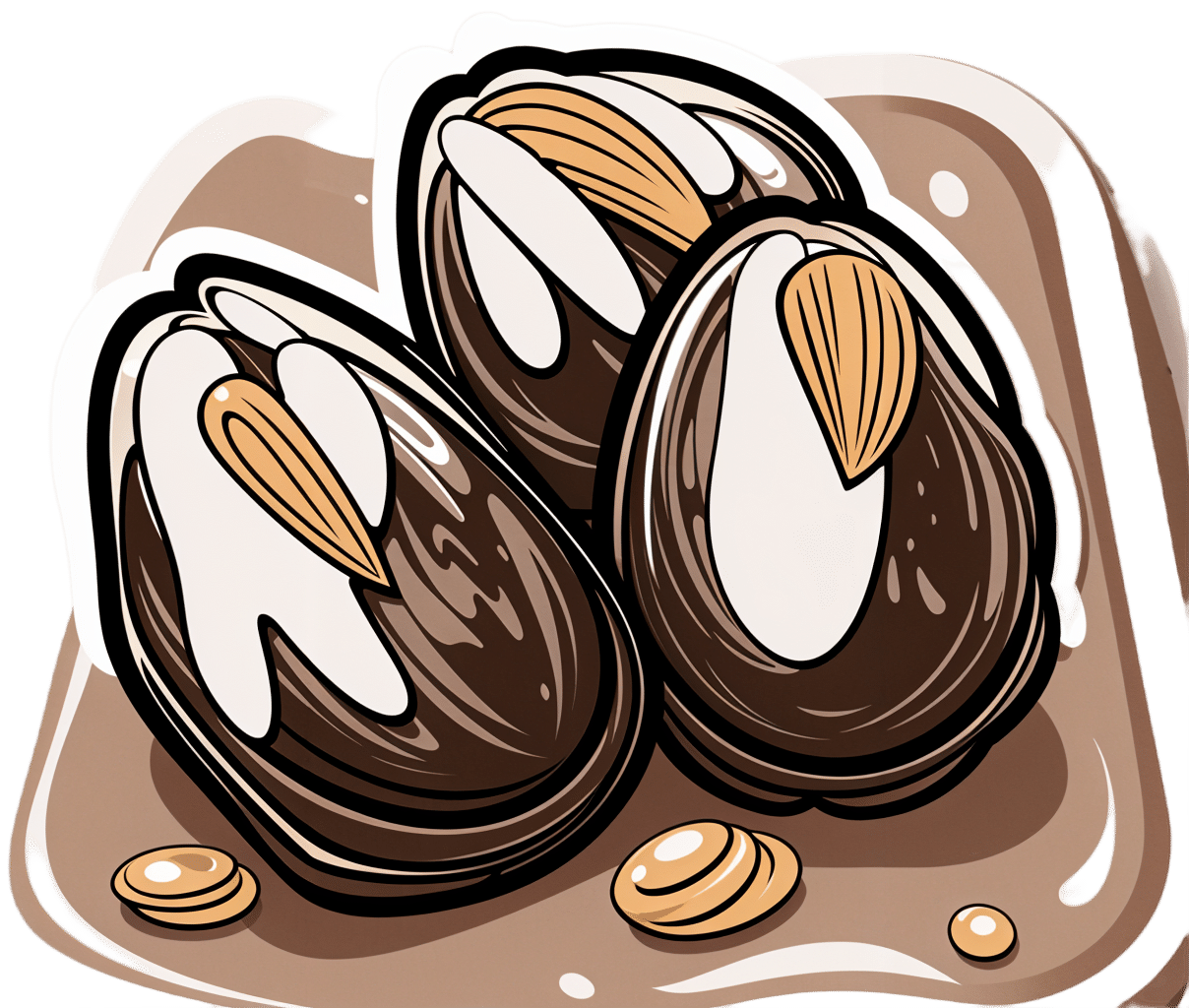
Tiramisu Crunch Bites
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s coffee, it’s creamy, it’s nutty, it’s chocolatey, what’s not to love? It has all the well-loved flavors of tiramisu, but this recipe is a simple one, and it’s essentially stuffed dates in a way you’ve never had them before. They’re delectable, decadent, and decidedly good for your health. These things are little nutrient-bombs that’ll keep you reaching for more.
You will need
- Coffee (we will discuss this)
- 150g (5.5oz) mascarpone (if vegan or lactose-intolerant, can be substituted with vegan varieties, or at a pinch, pressed silken tofu)
- 500g (1lb) dates (Medjool are ideal)
- Twice as many almonds as you have dates
- 50g (2oz) dark chocolate (the darkest, bitterest, you can find)
- Edible flower petals if you can source them (some shops sell dried rose petals for this purpose)
Method
(we suggest you read everything at least once before doing anything)
1) Take the mascarpone and whisk (or blend) it with the coffee. What kind of coffee, you ask? Many will use instant coffee (1tbsp granules mixed with enough boiling water to dissolve it), and that is actually healthiest (counterintuitive but true) but if you care for flavor over health, and have the means to make espresso, make it ristretto (so, stop it halfway through filling up an espresso cup), let it cool, and use that. Absolute bonus for flavor (not for health): if you have the means to make Turkish coffee, use an equivalent amount of that (again, cooled).
You will now have coffee-flavoured mascarpone. It’s great for your gut and full of antioxidant polyphenols. Set it aside for the moment.
2) Take the dark chocolate and melt it. Please don’t microwave it or try to do it in a pan directly over the hob; instead, you will need to use a Bain-Marie. If you don’t have one made-for-purpose, you can place a metal or heatproof glass bowl in a saucepan, with something to stop it from touching the floor of the pan. Then boil water in the pan (without letting the water get into the bowl), and melt the chocolate in the bowl—this will allow you to melt it evenly without burning the chocolate.
You will now have melted dark chocolate. It has its own set of polyphenols, and is great for everything from the brain to the gut microbiome.
3) Cut the dates lengthways on one side and remove the stone. Stuff them carefully with the coffee-flavored mascarpone (you can use a teaspoon, or use a piping kit if you have one). Add a couple of almonds to each one. Place them all on a big plate, and drizzle the melted chocolate over them. Add the petals if you have them.
The dates and almonds deliver extra vitamins and minerals in abundance (not to mention, lots of fiber), and also are an amazing combination even just by themselves. With the mascarpone and chocolate added, this winning on new levels. We’re not done yet, though…
4) Chill them in the fridge for about 30 minutes.
Serve!
Learn more
For those interested in some of the science of what we have going on today:
- Make The Heart-Healthiest Coffee ← this is about cafestol content and why instant is heart-healthiest (alas)
- The Bitter Truth About Coffee (Or Is It) ← this is about the health benefits (and some risks, but mostly benefits) of coffee
- Why You Should Diversify Your Nuts ← almonds are a top-tier choice, but other nuts are good too! This recipe could work well with hazelnuts, for example (we wouldn’t call it “tiramisu crunch bites” in that case, though, since the flavor profile would change)
- Which Sugars Are Healthier, And Which Are Just The Same? ← for any worrying “aren’t dates sugary, though?”
Enjoy!
Share This Post
-
154 million lives saved in 50 years: 5 charts on the global success of vaccines
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We know vaccines have been a miracle for public health. Now, new research led by the World Health Organization has found vaccines have saved an estimated 154 million lives in the past 50 years from 14 different diseases. Most of these have been children under five, and around two-thirds children under one year old.
In 1974 the World Health Assembly launched the Expanded Programme on Immunization with the goal to vaccinate all children against diphtheria, tetanus, pertussis (whooping cough), measles, polio, tuberculosis and smallpox by 1990. The program was subsequently expanded to include several other diseases.
The modelling, marking 50 years since this program was established, shows a child aged under ten has about a 40% greater chance of living until their next birthday, compared to if we didn’t have vaccines. And these positive effects can be seen well into adult life. A 50-year-old has a 16% greater chance of celebrating their next birthday thanks to vaccines.
What the study did
The researchers developed mathematical and statistical models which took in vaccine coverage data and population numbers from 194 countries for the years 1974–2024. Not all diseases were included (for example smallpox, which was eradicated in 1980, was left out).
The analysis includes vaccines for 14 diseases, with 11 of these included in the Expanded Programme on Immunization. For some countries, additional vaccines such as Japanese encephalitis, meningitis A and yellow fever were included, as these diseases contribute to major disease burden in certain settings.
The models were used to simulate how diseases would have spread from 1974 to now, as vaccines were introduced, for each country and age group, incorporating data on increasing vaccine coverage over time.
Children are the greatest beneficiaries of vaccines
Since 1974, the rates of deaths in children before their first birthday has more than halved. The researchers calculated almost 40% of this reduction is due to vaccines.
The effects have been greatest for children born in the 1980s because of the intensive efforts made globally to reduce the burden of diseases like measles, polio and whooping cough.
Some 60% of the 154 million lives saved would have been lives lost to measles. This is likely due to its ability to spread rapidly. One person with measles can spread the infection to 12–18 people.
The study also found some variation across different parts of the world. For example, vaccination programs have had a much greater impact on the probability of children living longer across low- and middle-income countries and settings with weaker health systems such as the eastern Mediterranean and African regions. These results highlight the important role vaccines play in promoting health equity.
Vaccine success is not assured
Low or declining vaccine coverage can lead to epidemics which can devastate communities and overwhelm health systems.
Notably, the COVID pandemic saw an overall decline in measles vaccine coverage, with 86% of children having received their first dose in 2019 to 83% in 2022. This is concerning because very high levels of vaccination coverage (more than 95%) are required to achieve herd immunity against measles.
In Australia, the coverage for childhood vaccines, including measles, mumps and rubella, has declined compared to before the pandemic.
This study is a reminder of why we need to continue to vaccinate – not just against measles, but against all diseases we have safe and effective vaccines for.
The results of this research don’t tell us the full story about the impact of vaccines. For example, the authors didn’t include data for some vaccines such as COVID and HPV (human papillomavirus). Also, like with all modelling studies, there are some uncertainties, as data was not available for all time periods and countries.
Nonetheless, the results show the success of global vaccination programs over time. If we want to continue to see lives saved, we need to keep investing in vaccination locally, regionally and globally.
Meru Sheel, Associate Professor and Epidemiologist, Infectious Diseases, Immunisation and Emergencies Group, Sydney School of Public Health, University of Sydney and Alexandra Hogan, Mathematical epidemiologist, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
The Plant-Based Athlete – by Matt Frazier and Robert Cheeke
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you’re already a seasoned plant-based athlete yourself, you can probably skip this book; the 60 recipes at the end would still provide value, but there is the “No Meat Athlete Cookbook” that you could hop straight to, in any case.
For most readers, there will be plenty of value from start to finish. We get a quick ground-up tour of nutrition basics, before getting into restructuring diet to optimize it for performance.
There is less in the way of “Vegans struggle with…” and more in the way of “People think vegans struggle with…” and explanations of what vegan athletes actually eat. The book does include science, but isn’t too science-heavy, and relies more on modelling what plant-based superathletes enjoy on a daily basis.
To that end,if the book has a weak point, it’s perhaps that it could have stood to include more science. The book comes recommended by Dr. Michael Greger, whose nutritional approach is incredibly science-heavy and well-referenced, and this book is obviously compatible with that (so they could have!), but in this case Frazier and Cheeke leave us to take their word for it.
Nevertheless, the science is good whether they cite it or not, and this book is quite a comprehensive primer of plant-based athleticism.
Bottom line: if you’re wondering how to optimize the two goals of “eating plants” and “being a powerful athlete”, then this one’s the book for you.
Click here to check out The Plant-Based Athlete and upgrade your health and athletic performance!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
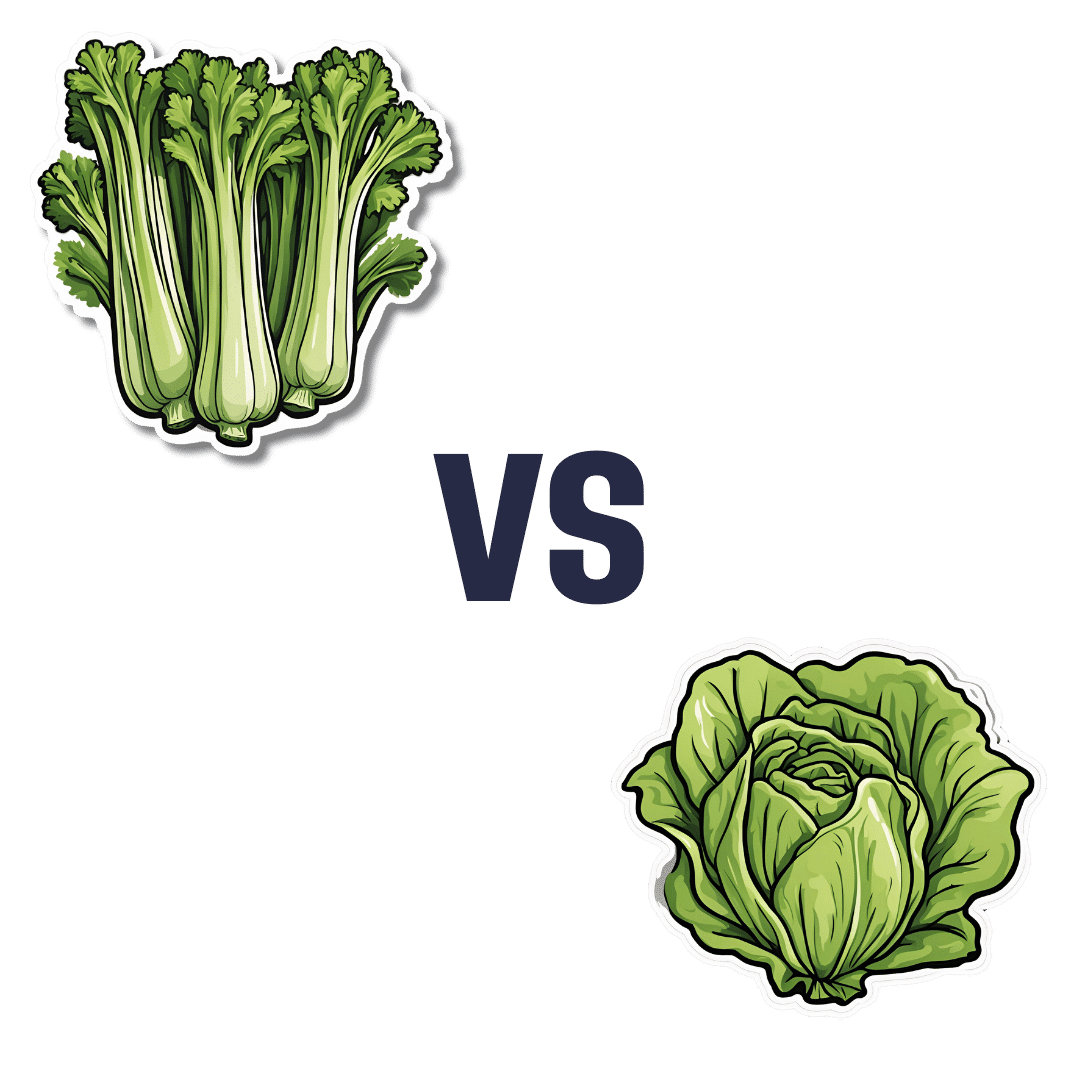
Celery vs Lettuce – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing celery to lettuce, we picked the lettuce.
Why?
Let us consider the macros first: lettuce has 2x the protein, but of course the numbers are tiny and probably nobody is eating this for the protein. Both of these salad items are roughly comparable in terms of carbs and fiber, being both mostly water with just enough other stuff to hold their shape. Nominally this section is a slight win for lettuce on account of the protein, but in realistic practical terms, it’s a tie.
In terms of vitamins, celery has more of vitamins B5 and E, while lettuce has more of vitamins A, B1, B2, B3, B6, B7, B9, C, K, and choline. An easy win for lettuce here.
In the category of minerals, celery has more calcium, copper, and potassium, while lettuce has more iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. So, a fair win for lettuce.
Adding up the sections makes for an overall win for lettuce; of course, enjoy both, though!
Want to learn more?
You might like to read:
Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
12 Questions For Better Brain Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We usually preface our “Expert Insights” pieces with a nice banner that has a stylish tall cutout that allows us to put a photo of the expert in. Today we’re not doing that, because for today’s camera-shy expert, we could only find one photo, and it’s a small, grainy, square headshot that looks like it was taken some decades ago, and would not fit our template at all. You can see it here, though!
In any case, Dr. Linda Selwa is a neurologist and neurophysiologist with nearly 40 years of professional experience.
The right questions to ask
As a neurologist, she found that one of the problems that results in delayed interventions (and thus, lower efficacy of those interventions) is that people don’t know there’s anything to worry about until a degenerative brain condition has degenerated past a certain point. With that in mind, she bids us ask ourselves the following questions, and discuss them with our primary healthcare providers as appropriate:
- Sleep: Are you able to get sufficient sleep to feel rested?
- Affect, mood and mental health: Do you have concerns about your mood, anxiety, or stress?
- Food, diet and supplements: Do you have concerns about getting enough or healthy enough food, or have any questions about supplements or vitamins?
- Exercise: Do you find ways to fit physical exercise into your life?
- Supportive social interactions: Do you have regular contact with close friends or family, and do you have enough support from people?
- Trauma avoidance: Do you wear seatbelts and helmets, and use car seats for children?
- Blood pressure: Have you had problems with high blood pressure at home or at doctor visits, or do you have any concerns about blood pressure treatment or getting a blood pressure cuff at home?
- Risks, genetic and metabolic factors: Do you have trouble controlling blood sugar or cholesterol? Is there a neurological disease that runs in your family?
- Affordability and adherence: Do you have any trouble with the cost of your medicines?
- Infection: Are you up to date on vaccines, and do you have enough information about those vaccines?
- Negative exposures: Do you smoke, drink more than one to two drinks per day, or use non-prescription drugs? Do you drink well water, or live in an area with known air or water pollution?
- Social and structural determinants of health: Do you have concerns about keeping housing, having transportation, having access to care and medical insurance, or being physically or emotionally safe from harm?
You will note that some of these are well-known (to 10almonds readers, at least!) risk factors for cognitive decline, but others are more about systemic and/or environmental considerations, things that don’t directly pertain to brain health, but can have a big impact on it anyway.
About “concerns”: in the case of those questions that ask “do you have concerns about…?”, and you’re not sure, then yes, you do indeed have concerns.
About “trouble”: as for these kinds of health-related questionnaires in general, if a question asks you “do you have trouble with…?” and your answer is something like “no, because I have a special way of dealing with that problem” then the answer for the purposes of the questionnaire is yes, you do indeed have trouble.
Note that you can “have trouble with” something that you simultaneously “have under control”—just as a person can have no trouble at all with something that they leave very much out of control.
Further explanation on each of the questions
If you’re wondering what is meant by any of these, or what counts, or why the question is even being asked, then we recommend you check out Dr. Selwa et al’s recently-published paper, then all is explained in there, in surprisingly easy-to-read fashion:
Emerging Issues In Neurology: The Neurologist’s Role in Promoting Brain Health
If you scroll past the abstract, introduction, and disclaimers, then you’ll be straight into the tables of information about the above 12 factors.
Want to be even more proactive?
Check out:
How To Reduce Your Alzheimer’s Risk
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: