Pelvic Floor Exercises (Not Kegels!) To Prevent Urinary Incontinence
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s a common threat, and if you think it couldn’t happen to you, then well, just wait. Happily, Dr. Christine Pieton, PT, DPT, a sport & women’s health physical therapist, has advice:
On the ball!
Or rather, we’re going to be doing ball-squeezing here, if you’ll pardon the expression. You will need a soccer-ball sized ball to squeeze.
Ball-squeeze breathing: lie on your back, ball between your knees, and inhale deeply, expanding your torso. Exhale, pressing your knees into the ball, engaging your abdominal muscles from lower to upper. Try to keep your spine long and avoid your pelvis tucking under during the exhalation.
Ball-squeeze bridge: lie on your back, ball between your knees, inhale to prepare, and then exhale, pressing up into a bridge, maintaining a firm pressure on the ball. Inhale as you lower yourself back down.
Ball-squeeze side plank: lie on your side this time, ball between your knees, supporting forearm under your shoulder, as in the video thumbnail. Inhale to prepare, and then exhale, lifting your hip a few inches off the mat. Inhale as you lower yourself back down.
Ball-squeeze bear plank: get on your hands and knees, ball between your thighs. Lengthen your spine, inhale to prepare, and exhale as you bring your knees just a little off the floor. Inhale as you lower yourself back down.
For more details and tips on each of these, plus a visual demonstration, plus an optional part 2 video with more exercises that aren’t ball-squeezes this time, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Psst… A Word To The Wise About UTIs
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why 7 Hours Sleep Is Not Enough
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How Sleep-Deprived Are You, Really?
This is Dr. Matthew Walker. He’s a neuroscientist and sleep specialist, and is the Director of the Center for Human Sleep Science at UC Berkeley’s Department of Psychology. He’s also the author of the international bestseller “Why We Sleep”.
What does he want us to know?
Sleep deprivation is more serious than many people think it is. After about 16 hours without sleep, the brain begins to fail, and needs more than 7 hours of sleep to “reset” cognitive performance.
Note: note “seven or more”, but “more than seven”.
After ten days with only 7 hours sleep (per day), Dr. Walker points out, the brain is as dysfunctional as it would be after going without sleep for 24 hours.
Here’s the study that sparked a lot of Dr. Walker’s work:
Importantly, in Dr. Walker’s own words:
❝Three full nights of recovery sleep (i.e., more nights than a weekend) are insufficient to restore performance back to normal levels after a week of short sleeping❞
~ Dr. Matthew Walker
See also: Why You Probably Need More Sleep
Furthermore: the sleep-deprived mind is unaware of how sleep-deprived it is.
You know how a drunk person thinks they can drive safely? It’s like that.
You do not know how sleep-deprived you are, when you are sleep-deprived!
For example:
❝(60.7%) did not signal sleepiness before a sleep fragment occurred in at least one of the four MWT trials❞
Source: Sleepiness is not always perceived before falling asleep in healthy, sleep-deprived subjects
Sleep efficiency matters
With regard to the 7–9 hours band for optimal health, Dr. Walker points out that the sleep we’re getting is not always the sleep we think we’re getting:
❝Assuming you have a healthy sleep efficiency (85%), to sleep 9 hours in terms of duration (i.e. to be a long-sleeper), you would need to be consistently in bed for 10 hours and 36 minutes a night. ❞
~ Dr. Matthew Walker
At the bottom end of that, by the way, doing the same math: to get only the insufficient 7 hours sleep discussed earlier, a with a healthy 85% sleep efficiency, you’d need to be in bed for 8 hours and 14 minutes per night.
The unfortunate implication of this: if you are consistently in bed for 8 hours and 14 minutes (or under) per night, you are not getting enough sleep.
“But what if my sleep efficiency is higher than 85%?”
It shouldn’t be.If your sleep efficiency is higher than 85%, you are sleep-deprived and your body is having to enforce things.
Want to know what your sleep efficiency is?
We recommend knowing this, by the way, so you might want to check out:
Head-To-Head Comparison of Google and Apple’s Top Sleep-Monitoring Apps
(they will monitor your sleep and tell you your sleep efficiency, amongst other things)
Want to know more?
You might like his book:
Why We Sleep: Unlocking the Power of Sleep and Dreams
…and/or his podcast:
…and for those who like videos, here’s his (very informative) TED talk:
Prefer text? Click here to read the transcript
Want to watch it, but not right now? Bookmark it for later
Enjoy!
Share This Post
-
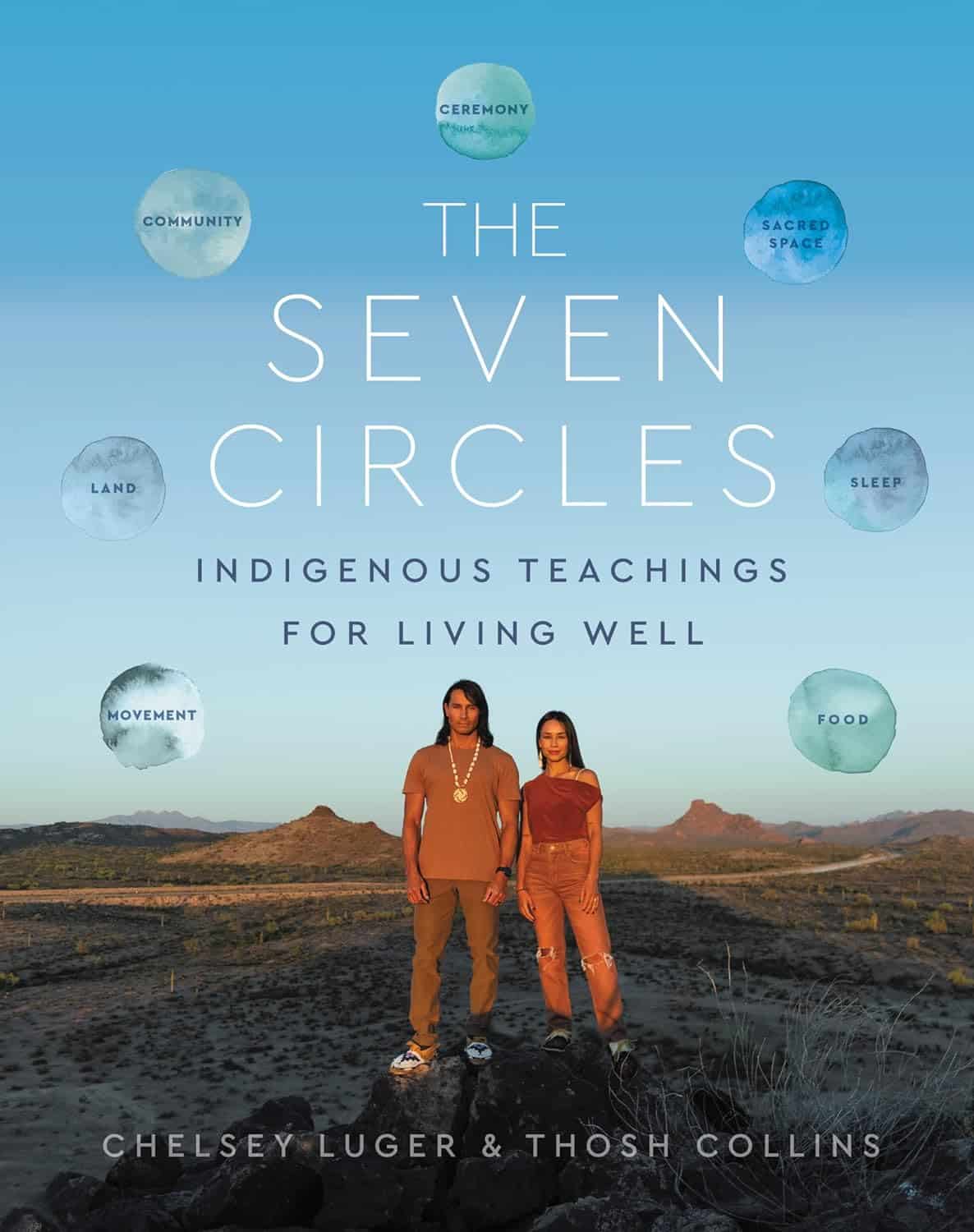
The Seven Circles – by Chelsey Luger & Thosh Collins
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At first glance, this can seem like an unscientific book—you won’t find links to studies in this one, for sure! However, if we take a look at the seven circles in question, they are:
- Food
- Movement
- Sleep
- Ceremony
- Sacred Space
- Land
- Community
Regular 10almonds readers may notice that these seven items contain five of the things strongly associated with the “supercentenarian Blue Zones”. (If you are wondering why Native American reservations are not Blue Zones, the answer there lies less in health science and more in history and sociology, and what things have been done to a given people).
The authors—who are Native American, yes—present in one place a wealth of knowledge and know-how. Not even just from their own knowledge and their own respective tribes, but gathered from other tribes too.
Perhaps the strongest value of this book to the reader is in the explanation of noting the size of each of those circles, how they connect with each other, and providing a whole well-explained system for how we can grow each of them in harmony with each other.
Or to say the same thing in sciencey terms: how to mindfully improve integrated lifestyle factors synergistically for greater efficacy and improved health-adjusted quality-of-life years.
Bottom line: if you’re not averse to something that mostly doesn’t use sciencey terms of have citations to peer-reviewed studies peppered through the text, then this book has wisdom that’s a) older than the pyramids of Giza, yet also b) highly consistent with our current best science of Blue Zone healthy longevity.
Share This Post
-
Tempeh vs Tofu – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing tempeh to tofu, we picked the tempeh.
Why?
Per 100g, tempeh has about 1.5x as many calories, about 2x as much protein, about 3x as much fiber, and about 4x the carbohydrates.
Which latter sounds like a lot, but really, the amounts here are small—tempeh is under 12% carbohydrates, and most of that is treated by the body as fiber (e.g. it’s a resistant starch).
Both have no sugar, and both have more or less the same (tiny) amount of fat.
Micronutrients, you ask? As they’re both made from soybeans, the micronutrient profiles are similar, but exact amounts will depend on the method used, so by all means check labels if comparing products in store. By and large, there’s usually not much difference, though.
You can see sample stats here:
In summary
Both are great, and/but tempeh is the more nutrient-dense of the two.
Therefore, tempeh is the healthier option, unless you are on a very strictly calorie-controlled diet, in which case, tofu will give you more quantity per calorie.
Enjoy!
Share This Post
Related Posts
-
Sun-Dried Tomatoes vs Carrots – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing sun-dried tomatoes to carrots, we picked the sun-dried tomatoes.
Why?
After tomatoes lost to carrots yesterday, it turns out that sun-drying them is enough to turn the nutritional tables!
This time, it’s the sun-dried tomatoes that have more carbs and fiber, as well as the nominally lower glycemic index (although obviously, carrots are also just fine in this regard; nobody is getting metabolic disease from eating carrots). Still, by the numbers, a win for sun-dried tomatoes.
In terms of vitamins, the fact that they have less water-weight means that proportionally, gram for gram, sun-dried tomatoes have more of vitamins B1, B2, B3, B5, B6, B9, C, E, K, and choline, while carrots still have more vitamin A. An easy win for sun-dried tomatoes on the whole, though.
When it comes to minerals, sun-dried tomatoes have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while carrots are not higher in any mineral.
Looking at polyphenols, sun-dried tomatoes have more, including a good healthy dose of quercetin; they also have more lycopene, not technically a polyphenol by virtue of its chemical structure (it’s a carotenoid), but a powerful phytochemical nonetheless. And, the lycopene content is higher in sun-dried tomatoes (compared to raw tomatoes) not just because of the loss of water-weight making a proportional difference, but also because the process itself improves the lycopene content, much like cooking does.
All in all, a clear and overwhelming win for sun-dried tomatoes.
Just watch out, as this is about the sun-dried tomatoes themselves; if you get them packed in vegetable oil, as is common, it’ll be a very different nutritional profile!
Want to learn more?
You might like to read:
Tomatoes vs Carrots – Which is Healthier? ← see the difference!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Superfood Energy Balls
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
They are healthy, they are tasty, they are convenient! Make some of these and when you need an energizing treat at silly o’clock when you don’t have time to prepare something, here they are, full of antioxidants, vitamins and minerals, good for blood sugars too, and ready to go:
You will need
- 1 cup pitted dates
- 1 cup raw mixed nuts
- ¼ cup goji berries
- 1 tbsp cocoa powder
- 1 tsp chili flakes
Naturally, you can adjust the spice level if you like! But this is a good starter recipe.
Method
(we suggest you read everything at least once before doing anything)
1) Blend all the ingredients in a good processor to make a dough
2) Roll the dough into 1″ balls; you should have enough dough for about 16 balls. If you want them to be pretty, you can roll them in some spare dry ingredients (e.g. chopped nuts, goji berries, chili flakes, seeds of some kind, whatever you have in your kitchen that fits the bill).
3) Refrigerate for at least 1–2 hours, and serve! They can also be kept in the fridge for at least a good while—couldn’t tell you how long for sure though, because honestly, they’ve never stayed that long in the fridge without being eaten.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Dates vs Figs – Which is Healthier?
- Why You Should Diversify Your Nuts!
- Goji Berries: Which Benefits Do They Really Have?
- The Sugary Food That Lowers Blood Sugars
- Enjoy Bitter Foods For Your Heart & Brain
- Capsaicin’s Hot Benefits
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Path To Revenue – by Theresa Marcroft
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
So many books about start-ups skip right over the elephant in the room: survivorship bias. Not so for Marcroft! This book contains the most comprehensive and unapologetic treatment of it we’ve seen.
Less “here’s what Steve Jobs did right and here’s what Chocolate-Teapots-For-Dogs-R-Us did wrong; don’t mess up that badly and you’ll be fine”… and more realism. Marcroft gives us a many-angled critical analytic approach. In it, she examines why many things can seem similar in both content and presentation… but can cause growth or failure (and how and why), based on more than anecdotes and luck.
The book is information-dense (taking a marketing-centric approach) and/but well-presented in a very readable format.
If we can find any criticism of the book, it’s less about what’s in it and more about what’s not in it. This can never be a “your start-up bible!” book because it’s not comprehensive. It doesn’t cover assembling your team, for example. Nor does it give a lot of attention to management, preferring to focus on strategy.
But no single book can be all things, and we highly recommend this one—the marketing advice alone is more than worth the cost of the book!
Take Your First Step Along The Path To Revenue By Checking It Out On Amazon!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: