Pasteurization: What It Does And Doesn’t Do
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Pasteurization’s Effect On Risks & Nutrients
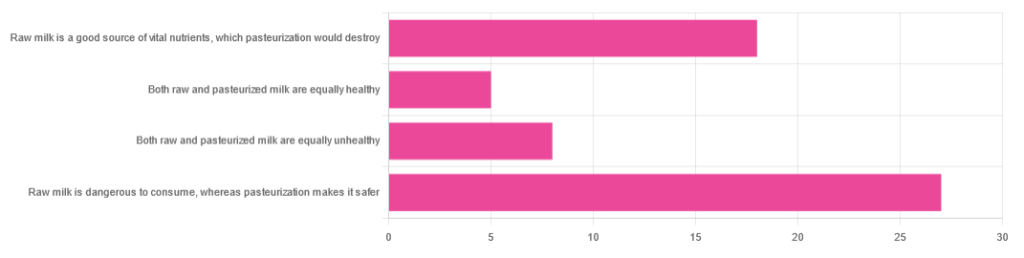
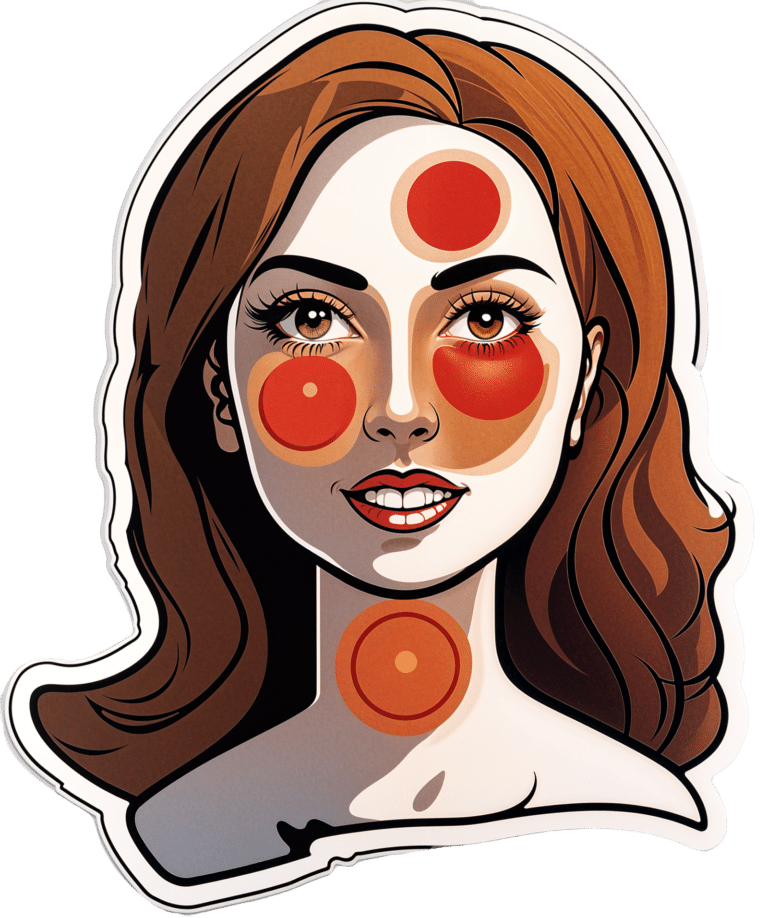
In Wednesday’s newsletter, we asked you for your health-related opinions of raw (cow’s) milk, and got the above-depicted, below-described, set of responses:
- About 47% said “raw milk is dangerous to consume, whereas pasteurization makes it safer”
- About 31% said “raw milk is a good source of vital nutrients which pasteurization would destroy”
- About 14% said “both raw milk and pasteurized milk are equally unhealthy”
- About 9% said “both raw milk and pasteurized milk are equally healthy”
Quite polarizing! So, what does the science say?
“Raw milk is dangerous to consume, whereas pasteurization makes it safer: True or False?”
True! Coincidentally, the 47% who voted for this are mirrored by the 47% of the general US population in a similar poll, deciding between the options of whether raw milk is less safe to drink (47%), just as safe to drink (15%), safer to drink (9%), or not sure (30%):
Public Fails to Appreciate Risk of Consuming Raw Milk, Survey Finds
As for what those risks are, by the way, unpasteurized dairy products are estimated to cause 840x more illness and 45x more hospitalizations than pasteurized products.
This is because unpasteurized milk can (and often does) contain E. coli, Listeria, Salmonella, Cryptosporidium, and other such unpleasantries, which pasteurization kills.
Source for both of the above claims:
(we know the title sounds vague, but all this information is easily visible in the abstract, specifically, the first two paragraphs)
Raw milk is a good source of vital nutrients which pasteurization would destroy: True or False?
False! Whether it’s a “good” source can be debated depending on other factors (e.g., if we considered milk’s inflammatory qualities against its positive nutritional content), but it’s undeniably a rich source. However, pasteurization doesn’t destroy or damage those nutrients.
Incidentally, in the same survey we linked up top, 16% of the general US public believed that pasteurization destroys nutrients, while 41% were not sure (and 43% knew that it doesn’t).
Note: for our confidence here, we are skipping over studies published by, for example, dairy farming lobbies and so forth. Those do agree, by the way, but nevertheless we like sources to be as unbiased as possible. The FDA, which is not completely unbiased, has produced a good list of references for this, about half of which we would consider biased, and half unbiased; the clue is generally in the journal names. For example, Food Chemistry and the Journal of Food Science and Journal of Nutrition are probably less biased than the International Dairy Association and the Journal of Dairy Science:
FDA | Raw Milk Misconceptions and the Danger of Raw Milk Consumption
this page covers a lot of other myths too, more than we have room to “bust” here, but it’s very interesting reading and we recommend to check it out!
Notably, we also weren’t able to find any refutation by counterexample on PubMed, with the very slight exception that some studies sometimes found that in the case of milks that were of low quality, pasteurization can reduce the vitamin E content while increasing the vitamin A content. For most milks however, no significant change was found, and in all cases we looked at, B-vitamins were comparable and vitamin D, popularly touted as a benefit of cow’s milk, is actually added later in any case. And, importantly, because this is a common argument, no change in lipid profiles appears to be findable either.
In science, when something has been well-studied and there aren’t clear refutations by counterexample, and the weight of evidence is clearly very much tipped into one camp, that usually means that camp has it right.
Milk generally is good/bad for the health: True or False?
True or False, depending on what we want to look at. It’s definitely not good for inflammation, but the whole it seems to be cancer-neutral and only increases heart disease risk very slightly:
- Keep Inflammation At Bay ← short version is milk is bad, fermented milk products are fine in moderation
- Is Dairy Scary? ← short version is that milk is neither good nor terrible; fermented dairy products however are health-positive in numerous ways when consumed in moderation
You may be wondering…
…how this goes for the safety of dairy products when it comes to the bird flu currently affecting dairy cows, so:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Herbal Supplement That Rivals Prozac
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Flower Power: St. John’s Wort’s Drug-Level Effectiveness
St. John’s wort is a small yellow flower, extract of which can be bought inexpensively off-the-shelf in pretty much any pharmacy in most places.
It’s sold and used as a herbal mood-brightener.
Does it work?
Yes! It’s actually very effective. This is really uncontroversial, so we’ll keep it brief.
The main findings of studies are that St. John’s wort not only gives significant benefits over placebo, but also works about as well as prescription anti-depressants:
A systematic review of St. John’s wort for major depressive disorder
They also found that fewer people stop taking it, compared to how many stop taking antidepressants. It’s not known how much of this is because of its inexpensive, freely-accessible nature, and how much might be because it gave them fewer adverse side effects:
Clinical use of Hypericum perforatum (St John’s wort) in depression: A meta-analysis
How does it work?
First and foremost, it’s an SSRI—a selective serotonin reuptake inhibitor. Basically, it doesn’t add serotonin, but it makes whatever serotonin you have, last longer. Same as most prescription antidepressants. It also affects adenosine and GABA pathways, which in lay terms, means it promotes feelings of relaxation, in a similar way to many prescription antianxiety medications.
Mechanism of action of St John’s wort in depression: what is known?
Any problems we should know about?
Yes, definitely. To quote directly from the National Center for Complementary and Integrative Health:
St. John’s wort can weaken the effects of many medicines, including crucially important medicines such as:
- Antidepressants
- Birth control pills
- Cyclosporine, which prevents the body from rejecting transplanted organs
- Some heart medications, including digoxin and ivabradine
- Some HIV drugs, including indinavir and nevirapine
- Some cancer medications, including irinotecan and imatinib
- Warfarin, an anticoagulant (blood thinner)
- Certain statins, including simvastatin
I’ve read all that, and want to try it!
As ever, we don’t sell it (or anything else), but here’s an example product on Amazon.
Please be safe and do check with your doctor and/or pharmacist, though!
Share This Post
-
Kiwi vs Grapefruit – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kiwi to grapefruit, we picked the kiwi.
Why?
In terms of macros, kiwi has nearly 2x the protein, slightly more carbs, and 2x the fiber; both fruits are low glycemic index foods, however.
When it comes to vitamins, kiwi has more of vitamins B3, B6, B7, B9, C, E, K, and choline, while grapefruit has more of vitamins A, B1, B2, and B5. An easy win for kiwi.
In the category of minerals, kiwi is higher in calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while grapefruit is not higher in any minerals. So, no surprises for guessing which wins this category.
One thing that grapefruit is a rich source of: furanocoumarin, which can inhibit cytochrome P-450 3A4 isoenzyme and P-glycoptrotein transporters in the intestine and liver—slowing down their drug metabolism capabilities, thus effectively increasing the bioavailability of many drugs manifold.
This may sound superficially like a good thing (improving bioavailability of things we want), but in practice it means that in the case of many drugs, if you take them with (or near in time to) grapefruit or grapefruit juice, then congratulations, you just took an overdose. This happens with a lot of meds for blood pressure, cholesterol (including statins), calcium channel-blockers, anti-depressants, benzo-family drugs, beta-blockers, and more. Oh, and Viagra, too. Which latter might sound funny, but remember, Viagra’s mechanism of action is blood pressure modulation, and that is not something you want to mess around with unduly. So, do check with your pharmacist to know if you’re on any meds that would be affected by grapefruit or grapefruit juice!
All in all, adding up the categories makes for an overwhelming total win for kiwis.
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← kiwi is top of the list!
Take care!
Share This Post
-
Fennel vs Onion – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing fennel to onion, we picked the fennel.
Why?
First note, in case you didn’t see the picture: we are talking about white onions here (also called brown onions, by virtue of their attire).
Looking at the macros, fennel has nearly 2x the fiber and a little more protein, while onion has more carbs. An easy win in this category for the fennel.
In the category of vitamins, fennel has more of vitamins A, B2, B3, B5, B9, C, E, K, and choline (most of them by generous margins and some by especially large margins, we are talking, for example, 480x the vitamin A, 29x the vitamin E, and 157x the vitamin K), while onions have more of vitmains B1 and B6. Another clear win for fennel.
When it comes to minerals, fennel has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while onion is not higher in any minerals. No prizes for guessing: fennel wins this category too.
You may be curious as to how they add up on the polyphenol front, and the answer is, they don’t, much. Wonderful as these two vegetables are, an abundance of polyphenols is not amongst their strengths; fennel has some lignans and onion has some flavonols, but we’re talking tiny numbers here (in contrast, red onion would have aced it with 120mg/100g quercetin, amongst others, but red onion wasn’t on trial today).
Adding up the sections makes a clear win for fennel today.
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Share This Post
Related Posts
-
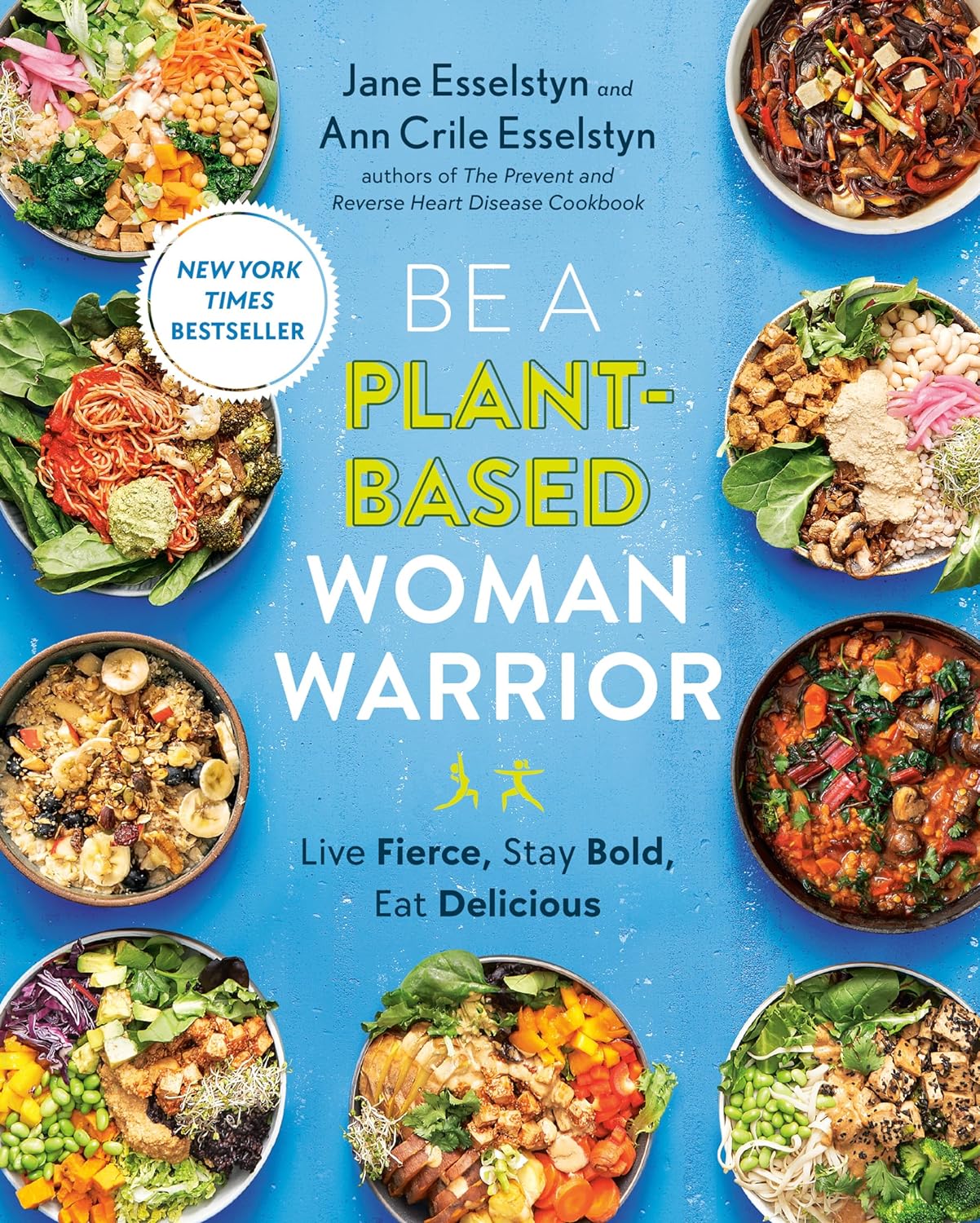
Be A Plant-Based Woman Warrior – by Jane Esselstyn & Ann Esselstyn
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Notwithstanding the title, this book is not about being a woman or a warrior, but let us share what one reviewer on Amazon wrote:
❝I don’t want to become a plant based woman warrior. The sex change would be traumatic for me. However, as a man who proudly takes ballet classes and Pilates, I am old enough not to worry about stereotypes. When I see a good thing, I am going to use it❞
The authors, a mother-and-daughter team in their 80s and 50s respectively, do give a focus on things that disproportionally affect women, and rectifying those things with diet, especially in one of the opening chapters.
Most the book, however, is about preventing/reversing things that can affect everyone, such as heart disease, diabetes, inflammation and the autoimmune diseases associated with such, and cancer in general, hence the dietary advice being good for most people (unless you have an unusually restrictive diet).
We get an overview of the pantry we should cultivate and curate, as well as some basic kitchen skills that will see us well for the rest of the book, such as how to make oat flour and other similar mini-recipes, before getting into the main recipes themselves.
About the recipes: they are mostly quite simple, though often rely on having pre-prepared items from the mini-recipes we mentioned earlier. They’re all vegan, mostly but not all gluten-free, whole foods, no added sugar, and as for oil… Well, it seems to be not necessarily oil-free, but rather oil-taboo. You see, they just don’t mention it. For example, when they say to caramelize onions, they say to heat a skillet, and when it is hot, add the onions, and stir until browned. They don’t mention any oil in the ingredients or in the steps. It is a mystery. 10almonds note: we recommend olive oil, or avocado oil if you prefer a milder taste and/or need a higher smoke point.
Bottom line: the odd oil taboo aside, this is a good book of simple recipes that teaches some good plant-based kitchen skills while working with a healthy, whole food pantry.
Click here to check out Be A Plant-Based Woman Warrior, and be a plant-based woman warrior!
Or at the very least: be a plant-based cook regardless of gender, hopefully without war, and enjoy the additions to your culinary repertoire
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Which Plant Milk?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Plant-based milks—what’s best?
You asked us to look at some popular plant milks and their health properties, and we said we’d do a main feature, so here it is!
We’ll also give a quick nod to environmental considerations at the end too (they might not be quite what you expect!). That said, as a health and productivity newsletter, we’ll be focusing on the health benefits.
While we can give a broad overview, please note that individual brands may vary, especially in two important ways:
- Pro: many (most?) brands of plant milks fortify their products with extra vitamins and minerals, especially vitamin D and calcium.
- Con: some brands also add sugar.
So, by all means use this guide to learn about the different plants’ properties, and/but still do check labels later.
Alternatively, consider making your own!
- Pros: no added sugar + cheaper
- Cons: no added vitamins and minerals + some equipment required
Almond milk
Almond milk is low in carbs and thus good for a carb-controlled diet. It’s also high in vitamin E and a collection of minerals.
Oat milk
Oats are one of the healthiest “staple foods” around, and while drinking oat milk doesn’t convey all the benefits, it does a lot. It also has one of the highest soluble fiber contents of any milk, which is good for reducing LDL (bad) cholesterol levels.
See for example: Consumption of oat milk for 5 weeks lowers serum cholesterol and LDL cholesterol in free-living men with moderate hypercholesterolemia
Coconut milk
Coconut has a higher fat content than most plant milks, but also contains medium-chain triglycerides (MCTs). These raise HDL (good) cholesterol levels.
Read the study: How well do plant based alternatives fare nutritionally compared to cow’s milk?
Hemp milk
Being made from hemp seeds that contain a lot of protein and healthy fats (including omega-3 and omega-6), hemp milk packs a nutritious punch. It’s carb-free. It’s also THC-free, in case you were wondering, which means no, it does not have psychoactive effects.
Pea milk
It’s very high in protein, and contains an array of vitamins and minerals. It’s not very popular yet, so there isn’t as much research about it. This 2021 study found that it had the nutritional profile the closest to cow’s milk (beating soy by a narrow margin) and praised it as a good alternative for those with a soy allergy.
This is Research Review Monday so we try to stick to pure science, but for your interest… here’s an interesting pop-science article (ostensibly in affiliation with the pea milk brand, Ripple) about the nutritional qualities of their pea milk specifically, which uses particularly nutrient-dense yellow peas, plus some extra vitamin and mineral fortifications:
Read: Ripple Milk: 6 Reasons Why You Should Try Pea Milk
Soy milk
Perhaps the most popular plant milk, and certainly usually the cheapest in stores. It’s high in protein, similar to cow’s milk. In fact, nutritionally, it’s one of the closest to cow’s milk without involving cows as a middleman. (Did you know three quarters of all soy in the world is grown to feed to livestock, not humans? Now you do).
And no, gentlemen-readers, it won’t have any feminizing effects. The human body can’t use the plant estrogens in soy for that. It does give some isoflavone benefits though, which are broadly good for everyone’s health. See for example this research review with 439 sources of its own:
Read: Soy and Health Update: Evaluation of the Clinical and Epidemiologic Literature
Quick note on flavor: nut milks have the flavor of the nut they were made from. Coconut milk tastes of coconut. The other milks listed above don’t have much of a flavor—which in many cases may be what you want.
Note on environmental considerations:
A lot of us try to be as socially responsible as reasonably possible in our choices, so this may be an influencing factor. In a nutshell:
- Oats and Soy are generally grown as vast monocrops, and these are bad for the environment
- They are still better for the environment than cow’s milk though, as for example most soy is grown to feed to cows, not humans. So including cows in the process means four times as much monocrop farming, plus adds several other environmental issues that are beyond the scope of this newsletter.
- Almonds are particularly resource-intensive when it comes to water use.
- Still nowhere near as much as cows, though.
- Peas are grown in places that naturally have very high rainfall, so are a good option here. Same generally goes for rice, which didn’t make the cut today. (Nor did hazelnuts, sorry—we can only include so much!)
- Hemp is by far and away the most environmentally friendly, assuming it is grown in a climate naturally conducive to such.
- Making plant milk at home is usually most environmentally friendly, depending on where your ingredients came from.
- Literally any plant milk is much more environmentally friendly than cow’s milk.
See the science for yourself: Reducing food’s environmental impacts through producers and consumers
See also (if you like graphs and charts): Environmental footprints of dairy and plant-based milks
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
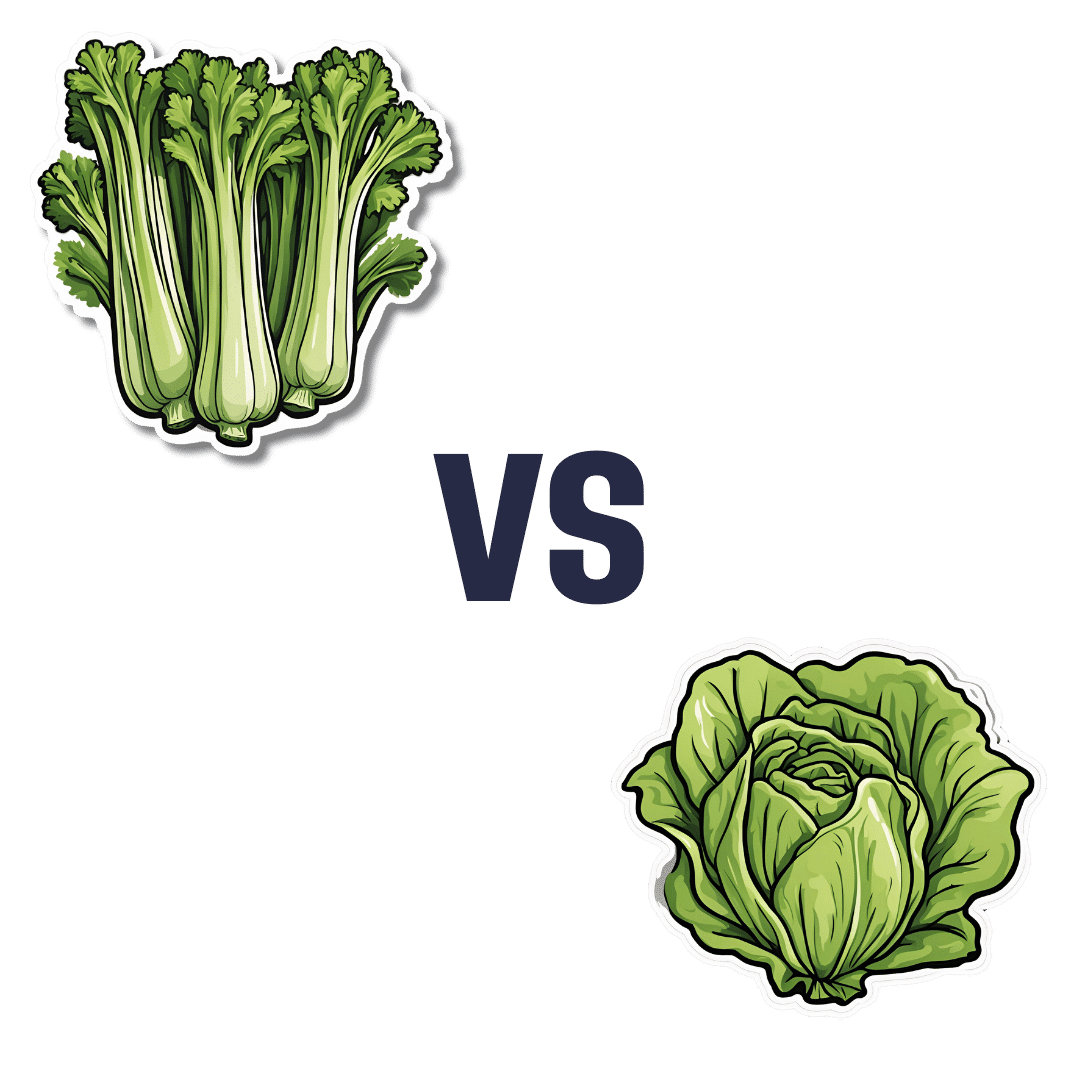
Celery vs Lettuce – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing celery to lettuce, we picked the lettuce.
Why?
Let us consider the macros first: lettuce has 2x the protein, but of course the numbers are tiny and probably nobody is eating this for the protein. Both of these salad items are roughly comparable in terms of carbs and fiber, being both mostly water with just enough other stuff to hold their shape. Nominally this section is a slight win for lettuce on account of the protein, but in realistic practical terms, it’s a tie.
In terms of vitamins, celery has more of vitamins B5 and E, while lettuce has more of vitamins A, B1, B2, B3, B6, B7, B9, C, K, and choline. An easy win for lettuce here.
In the category of minerals, celery has more calcium, copper, and potassium, while lettuce has more iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. So, a fair win for lettuce.
Adding up the sections makes for an overall win for lettuce; of course, enjoy both, though!
Want to learn more?
You might like to read:
Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: