Pain Doesn’t Belong on a Scale of Zero to 10
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Over the past two years, a simple but baffling request has preceded most of my encounters with medical professionals: “Rate your pain on a scale of zero to 10.”
I trained as a physician and have asked patients the very same question thousands of times, so I think hard about how to quantify the sum of the sore hips, the prickly thighs, and the numbing, itchy pain near my left shoulder blade. I pause and then, mostly arbitrarily, choose a number. “Three or four?” I venture, knowing the real answer is long, complicated, and not measurable in this one-dimensional way.
Pain is a squirrely thing. It’s sometimes burning, sometimes drilling, sometimes a deep-in-the-muscles clenching ache. Mine can depend on my mood or how much attention I afford it and can recede nearly entirely if I’m engrossed in a film or a task. Pain can also be disabling enough to cancel vacations, or so overwhelming that it leads people to opioid addiction. Even 10+ pain can be bearable when it’s endured for good reason, like giving birth to a child. But what’s the purpose of the pains I have now, the lingering effects of a head injury?
The concept of reducing these shades of pain to a single number dates to the 1970s. But the zero-to-10 scale is ubiquitous today because of what was called a “pain revolution” in the ’90s, when intense new attention to addressing pain — primarily with opioids — was framed as progress. Doctors today have a fuller understanding of treating pain, as well as the terrible consequences of prescribing opioids so readily. What they are learning only now is how to better measure pain and treat its many forms.
About 30 years ago, physicians who championed the use of opioids gave robust new life to what had been a niche specialty: pain management. They started pushing the idea that pain should be measured at every appointment as a “fifth vital sign.” The American Pain Society went as far as copyrighting the phrase. But unlike the other vital signs — blood pressure, temperature, heart rate, and breathing rate — pain had no objective scale. How to measure the unmeasurable? The society encouraged doctors and nurses to use the zero-to-10 rating system. Around that time, the FDA approved OxyContin, a slow-release opioid painkiller made by Purdue Pharma. The drugmaker itself encouraged doctors to routinely record and treat pain, and aggressively marketed opioids as an obvious solution.
To be fair, in an era when pain was too often ignored or undertreated, the zero-to-10 rating system could be regarded as an advance. Morphine pumps were not available for those cancer patients I saw in the ’80s, even those in agonizing pain from cancer in their bones; doctors regarded pain as an inevitable part of disease. In the emergency room where I practiced in the early ’90s, prescribing even a few opioid pills was a hassle: It required asking the head nurse to unlock a special prescription pad and making a copy for the state agency that tracked prescribing patterns. Regulators (rightly) worried that handing out narcotics would lead to addiction. As a result, some patients in need of relief likely went without.
After pain doctors and opioid manufacturers campaigned for broader use of opioids — claiming that newer forms were not addictive, or much less so than previous incarnations — prescribing the drugs became far easier and were promoted for all kinds of pain, whether from knee arthritis or back problems. As a young doctor joining the “pain revolution,” I probably asked patients thousands of times to rate their pain on a scale of zero to 10 and wrote many scripts each week for pain medication, as monitoring “the fifth vital sign” quickly became routine in the medical system. In time, a zero-to-10 pain measurement became a necessary box to fill in electronic medical records. The Joint Commission on the Accreditation of Healthcare Organizations made regularly assessing pain a prerequisite for medical centers receiving federal health care dollars. Medical groups added treatment of pain to their list of patient rights, and satisfaction with pain treatment became a component of post-visit patient surveys. (A poor showing could mean lower reimbursement from some insurers.)
But this approach to pain management had clear drawbacks. Studies accumulated showing that measuring patients’ pain didn’t result in better pain control. Doctors showed little interest in or didn’t know how to respond to the recorded answer. And patients’ satisfaction with their doctors’ discussion of pain didn’t necessarily mean they got adequate treatment. At the same time, the drugs were fueling the growing opioid epidemic. Research showed that an estimated 3% to 19% of people who received a prescription for pain medication from a doctor developed an addiction.
Doctors who wanted to treat pain had few other options, though. “We had a good sense that these drugs weren’t the only way to manage pain,” Linda Porter, director of the National Institutes of Health’s Office of Pain Policy and Planning, told me. “But we didn’t have a good understanding of the complexity or alternatives.” The enthusiasm for narcotics left many varietals of pain underexplored and undertreated for years. Only in 2018, a year when nearly 50,000 Americans died of an overdose, did Congress start funding a program — the Early Phase Pain Investigation Clinical Network, or EPPIC-Net — designed to explore types of pain and find better solutions. The network connects specialists at 12 academic specialized clinical centers and is meant to jump-start new research in the field and find bespoke solutions for different kinds of pain.
A zero-to-10 scale may make sense in certain situations, such as when a nurse uses it to adjust a medication dose for a patient hospitalized after surgery or an accident. And researchers and pain specialists have tried to create better rating tools — dozens, in fact, none of which was adequate to capture pain’s complexity, a European panel of experts concluded. The Veterans Health Administration, for instance, created one that had supplemental questions and visual prompts: A rating of 5 correlated with a frown and a pain level that “interrupts some activities.” The survey took much longer to administer and produced results that were no better than the zero-to-10 system. By the 2010s, many medical organizations, including the American Medical Association and the American Academy of Family Physicians, were rejecting not just the zero-to-10 scale but the entire notion that pain could be meaningfully self-reported numerically by a patient.
In the years that opioids had dominated pain remedies, a few drugs — such as gabapentin and pregabalin for neuropathy, and lidocaine patches and creams for musculoskeletal aches — had become available. “There was a growing awareness of the incredible complexity of pain — that you would have to find the right drugs for the right patients,” Rebecca Hommer, EPPIC-Net’s interim director, told me. Researchers are now looking for biomarkers associated with different kinds of pain so that drug studies can use more objective measures to assess the medications’ effect. A better understanding of the neural pathways and neurotransmitters that create different types of pain could also help researchers design drugs to interrupt and tame them.
Any treatments that come out of this research are unlikely to be blockbusters like opioids; by design, they will be useful to fewer people. That also makes them less appealing prospects to drug companies. So EPPIC-Net is helping small drug companies, academics, and even individual doctors design and conduct early-stage trials to test the safety and efficacy of promising pain-taming molecules. That information will be handed over to drug manufacturers for late-stage trials, all with the aim of getting new drugs approved by the FDA more quickly.
The first EPPIC-Net trials are just getting underway. Finding better treatments will be no easy task, because the nervous system is a largely unexplored universe of molecules, cells, and electronic connections that interact in countless ways. The 2021 Nobel Prize in Physiology or Medicine went to scientists who discovered the mechanisms that allow us to feel the most basic sensations: cold and hot. In comparison, pain is a hydra. A simple number might feel definitive. But it’s not helping anyone make the pain go away.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Off-Button For Your Brain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Off-Button For Your Brain
We evolved our emotions for our own benefit as a species. Even the “negative” ones:
- Stress keeps us safe by making sure we take important situations seriously
- Anger keeps us safe by protecting us from threats
- Disgust keeps us safe by helping us to avoid things that might cause disease
- Anxiety keeps us safe by ensuring we don’t get complacent
- Guilt keeps us safe by ensuring we can function as a community
- Sadness keeps us safe by ensuring we value things that are important to us, and learn to become averse to losing them
- …and so on
But that’s not always useful. What was once a very good response to a common source of fear (for example, a sabre-toothed tiger) is no longer a helpful response to a modern source of fear (for example, an important interview).
Sometimes it’s good to take the time and energy to process our feelings and the event(s) that prompted those feelings. Sometimes, we don’t have that luxury.
For example, if you are stressed about your workload? Then staying awake half the night thinking about it is only going to make your problems worse the next day.
So, how to switch that off, or at least put a pause on it?
The human mind tends to have a “negative bias”, evolved for our own protection. If something is “good enough”, we don’t need to worry about it, so we move on to the next thing, until we find something that is a problem, then we dwell on that. That’s not always helpful, and the good news is, there’s a way to flip the switch on this process:
Identifying the positive, and releasing the rest
This exercise can be done when you’re trying to sleep, or at any time you need a calmer, quieter mind.
Take a moment to notice whatever you’re experiencing.
If it’s something that feels good, or neutral, identify it with a single word. For example:
- Warmth
- Soft
- Security
- Smile
- Peace
If it’s something that feels bad, then instead of identifying it, simply say (or think) to yourself “release”.
You can’t fight bad feelings with force, and you can’t “just not think about them”, but you can dismiss them as soon as they arrive and move onto the next thing. So where your train of thought may previously have been:
It’s good to be in bed ➔ I have eight hours to sleep before my meeting ➔ Have I done everything I was supposed to? ➔ I hope that what I’ve done is good enough ➔ [Mentally rehearsing how the meeting might go] ➔ [various disaster preparations] ➔ What am I even going to wear? ➔ Ugh I forgot to do the laundry ➔ That reminds the electricity bill is due ➔ Etc
Now your train of thought may be more like:
Relief ➔ Rest ➔ But my meeti—release ➔ If I—release ➔ soft ➔ comfort ➔ release ➔ pillow ➔ smile ➔ release ➔ [and before you know it you’re asleep]
And if you do this in a situation where you’re not going to sleep? Same process, just a more wakeful result, for example, let’s move the scene to an office where your meeting will shortly take place:
Five minutes to go ➔ What a day ➔ Ok, I’d better clear my head a bit ➔ release ➔ release ➔ breath ➔ light ➔ chair ➔ what if—release ➔ prepared ➔ ready ➔ calm ➔ [and before you know it you’re impressing your work associate with your calm preparedness]
In summary:
If you need to stop a train of thought, this method may help. Especially if you’re in a situation where you can’t use some external distraction to keep you from thinking about the bad thing!
You’re probably still going to have to deal with the Bad Thing™ at some point—you’ve just recognized that now isn’t the time for that. Mentally postpone that so that you will be well-rested when you choose to deal with the Bad Thing™ later at your convenience.
So remember: identify the positive (with a single word), and anything else, just release.
Share This Post
-
16 Overlooked Autistic Traits In Women
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We hear a lot about “autism moms”, but Taylor Heaton is an autistic mom, diagnosed as an adult, and she has insights to share about overlooked autistic traits in women.
The Traits
- Difficulty navigating romantic relationships: often due to misreading signs
- Difficulty understanding things: including the above, but mostly: difficulty understanding subtext, when people leave things as “surely obvious”. Autistic women are likely to be aware of the possible meanings, but unsure which it might be, and may well guess wrongly.
- Masking: one of the reasons for the gender disparity in diagnosis is that autistic women are often better at “masking”, that is to say, making a conscious effort to blend in to allistic society—often as a result of being more societally pressured to do so.
- Honesty: often to a fault
- Copy and paste: related to masking, this is about consciously mirroring others in an effort to put them at ease and be accepted
- Being labelled sensitive and/or gifted: usually this comes at a young age, but the resultant different treatment can have a lifetime effect
- Secret stims: again related to masking, and again for the same reasons that displaying autistic symptoms is often treated worse in women, autistic women’s stims tend to be more subtle.
- Written communication: autistic women are often more comfortable with the written word than the spoken
- Leadership: autistic women will often gravitate to leadership roles, partly as a survival mechanism
- Gaslighting: oneself, e.g. “If this person did this without that, then I can to” (without taking into account that maybe the circumstances are different, or maybe they actually did lean on crutches that you didn’t know were there, etc).
- Inner dialogue: rich inner dialogue, but unable to express it outwardly—often because of the sheer volume of thoughts per second.
- Fewer female friends: often few friends overall, for that matter, but there’s often a gender imbalance towards male friends, or where there isn’t, towards more masculine friends at least.
- Feeling different: often a matter of feeling one does not meet standard expectations in some fashion
- School: autistic women are often academically successful
- Special interests: often more “socially accepted” interests than autistic men’s.
- Flirting: autistic women are often unsure how to flirt or what to do about it, which can result in simple directness instead
For more details on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Related reading:
You might like a main feature of ours from not long back:
Miss Diagnosis: Anxiety, ADHD, & Women
Take care!
Share This Post
-
Elderhood – by Dr. Louise Aronson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Where does “middle age” end, and “old age” begin? By the United States’ CDC’s categorization, human life involves:
- 17 stages of childhood, deemed 0–18
- 5 stages of adulthood, deemed 18–60
- 1 stage of elderhood, deemed 60+
Isn’t there something missing here? Do we just fall off some sort of conveyor belt on our sixtieth birthdays, into one big bucket marked “old”?
Yesterday you were 59 and enjoying your middle age; today you have, apparently, the same medical factors and care needs as a 114-year-old.
Dr. Louise Aronson, a geriatrician, notes however that medical science tends to underestimate the differences found in more advanced old age, and underresearch them. That elders consume half of a country’s medicines, but are not required to be included in clinical trials. That side effects not only are often different than for younger adults, but also can cause symptoms that are then dismissed as “Oh she’s just old”.
She explores, mostly through personal career anecdotes, the well-intentioned disregard that is frequently given by the medical profession, and—importantly—how we might overcome that, as individuals and as a society.
Bottom line: if you are over the age of 60, love someone over the age of 60, this is a book for you. Similarly if you and/or they plan to live past the age of 60, this is also a book for you.
Share This Post
Related Posts
-
State of Slim – by Dr. James Hill & Dr. Holly Wyatt
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The premise of this book is “people in Colorado are on average the slimmest in the US”, and sets about establishing why, and then doing what Coloradans are doing. As per the subtitle (drop 20 pounds in 8 weeks), this is a weight loss book and does assume that you want to lose weight—specifically, to lose fat. So if that’s not your goal, you can skip this one already.
The authors explain, as many diet and not-diet-but-diet-adjacent book authors do, that this is not a diet—and then do refer to it as the Colorado Diet throughout. So… Is it a diet?
The answer is a clear “yes, but”—and the caveat is “yes, but also some associated lifestyle practices”.
The diet component is basically a very low-carb diet to start with (with the day’s ration of carbs being a small amount of oats and whatever you can get from some non-starchy vegetables such as greens, tomatoes, etc), and then reintroducing more carbohydrate centric foods one by one, stopping after whole grains. If you are vegan or vegetarian, you can also skip this one already, because this advises eating six animal protein centric meals per day.
The non-diet components are very general healthy-living advices mixed in with popular “diet culture” advices, such as practice mindful eating, don’t eat after 8pm, exercise more, use small plates, enjoy yourself, pre-portion your snacks, don’t drink your calories, get 8 hours sleep, weigh all your food, etc.
Bottom line: this is a very mixed bag, even to the point of being a little chaotic. It gives sometimes contradictory advice, and/but this results in a very “something for everyone” cafeteria approach to dieting. The best recommendation we can give for this book is “it has very many ideas for you to try and see if they work for you”.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
16/8 Intermittent Fasting For Beginners
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Health Insider explains in super-simple fashion why and how to do Intermittent Fasting (IF), which is something that can sound complicated at first, but becomes very simple and easy once understood.
What do we need to know?
Intermittent fasting (IF) is a good, well-evidenced way to ease your body’s metabolic load, and
give your organs a chance to recover from the strain of digestion and its effects. That’s not just your gastrointestinal organs! It’s your pancreas and liver too, amongst others—this is about glucose metabolism as much as it is about digestion.This, in turn, allows your body some downtime to do its favorite thing, which is: maintenance!
This maintenance takes the form of enhanced cellular apoptosis and autophagy, helping to keep cells young and cancer-free.
In other words, with well-practised intermittent fasting, we can reduce our risk of metabolic disease (including heart disease and diabetes) as well as cancer and neurodegeneration.
You may be wondering: this sounds miraculous; what’s the catch? There are a couple:
- While fasting from food, the body’s enhanced metabolism requires more water, so you’ll need to take extra care keep on top of your hydration (this is one reason why Ramadan fasting, while healthy for most people, is not as healthy as IF—because Ramadan fasting means abstaining from water, too).
- If you are diabetic, and especially if you have Type 1 Diabetes, fasting may not be a safe option for you, since if you get a hypo in the middle of your fasting period, it’s obviously not a good idea to wait another many hours before fixing it.
Extra note on that last one: it’s easy to think “can’t I just lower my bolus insulin instead of eating?” and while superficially yes that will raise your blood sugar levels, it’s because the sugar will be sticking around in your blood, and not actually getting released into the organs that need it. So while your blood glucose monitor may say you’re fine, you will be starving your organs and if you keep it up they may suffer serious damage.
Disclaimer: our standard legal/medical disclaimer applies, and this is intended for educational purposes only; please do speak with your endocrinologist before changing anything you usually do with regard to your blood sugar maintenance.
Ok, back onto the cheerier topic at hand:
Aside from the above: for most people, IF is a remarkably healthful practice in very many ways.
For more on the science, practicalities, and things to do/avoid, enjoy this short (4:53) video:
Click Here If The Embedded Video Doesn’t Load Automatically
Want to know more?
Check out our previous main feature on this topic:
Intermittent Fasting: Mythbusting Edition
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why is cancer called cancer? We need to go back to Greco-Roman times for the answer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One of the earliest descriptions of someone with cancer comes from the fourth century BC. Satyrus, tyrant of the city of Heracleia on the Black Sea, developed a cancer between his groin and scrotum. As the cancer spread, Satyrus had ever greater pains. He was unable to sleep and had convulsions.
Advanced cancers in that part of the body were regarded as inoperable, and there were no drugs strong enough to alleviate the agony. So doctors could do nothing. Eventually, the cancer took Satyrus’ life at the age of 65.
Cancer was already well known in this period. A text written in the late fifth or early fourth century BC, called Diseases of Women, described how breast cancer develops:
hard growths form […] out of them hidden cancers develop […] pains shoot up from the patients’ breasts to their throats, and around their shoulder blades […] such patients become thin through their whole body […] breathing decreases, the sense of smell is lost […]
Other medical works of this period describe different sorts of cancers. A woman from the Greek city of Abdera died from a cancer of the chest; a man with throat cancer survived after his doctor burned away the tumour.
Where does the word ‘cancer’ come from?
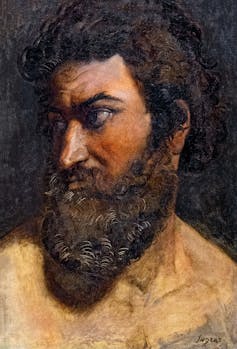
Why does the word ‘cancer’ have its roots in the ancient Greek and Latin words for crab? The physician Galen offers one explanation. Pierre Roche Vigneron/Wikimedia The word cancer comes from the same era. In the late fifth and early fourth century BC, doctors were using the word karkinos – the ancient Greek word for crab – to describe malignant tumours. Later, when Latin-speaking doctors described the same disease, they used the Latin word for crab: cancer. So, the name stuck.
Even in ancient times, people wondered why doctors named the disease after an animal. One explanation was the crab is an aggressive animal, just as cancer can be an aggressive disease; another explanation was the crab can grip one part of a person’s body with its claws and be difficult to remove, just as cancer can be difficult to remove once it has developed. Others thought it was because of the appearance of the tumour.
The physician Galen (129-216 AD) described breast cancer in his work A Method of Medicine to Glaucon, and compared the form of the tumour to the form of a crab:
We have often seen in the breasts a tumour exactly like a crab. Just as that animal has feet on either side of its body, so too in this disease the veins of the unnatural swelling are stretched out on either side, creating a form similar to a crab.
Not everyone agreed what caused cancer
The physician Erasistratus didn’t think black bile was to blame. Didier Descouens/Musée Ingres-Bourdelle/Wikimedia, CC BY-SA In the Greco-Roman period, there were different opinions about the cause of cancer.
According to a widespread ancient medical theory, the body has four humours: blood, yellow bile, phlegm and black bile. These four humours need to be kept in a state of balance, otherwise a person becomes sick. If a person suffered from an excess of black bile, it was thought this would eventually lead to cancer.
The physician Erasistratus, who lived from around 315 to 240 BC, disagreed. However, so far as we know, he did not offer an alternative explanation.
How was cancer treated?
Cancer was treated in a range of different ways. It was thought that cancers in their early stages could be cured using medications.
These included drugs derived from plants (such as cucumber, narcissus bulb, castor bean, bitter vetch, cabbage); animals (such as the ash of a crab); and metals (such as arsenic).
Galen claimed that by using this sort of medication, and repeatedly purging his patients with emetics or enemas, he was sometimes successful at making emerging cancers disappear. He said the same treatment sometimes prevented more advanced cancers from continuing to grow. However, he also said surgery is necessary if these medications do not work.
Surgery was usually avoided as patients tended to die from blood loss. The most successful operations were on cancers of the tip of the breast. Leonidas, a physician who lived in the second and third century AD, described his method, which involved cauterising (burning):
I usually operate in cases where the tumours do not extend into the chest […] When the patient has been placed on her back, I incise the healthy area of the breast above the tumour and then cauterize the incision until scabs form and the bleeding is stanched. Then I incise again, marking out the area as I cut deeply into the breast, and again I cauterize. I do this [incising and cauterizing] quite often […] This way the bleeding is not dangerous. After the excision is complete I again cauterize the entire area until it is dessicated.
Cancer was generally regarded as an incurable disease, and so it was feared. Some people with cancer, such as the poet Silius Italicus (26-102 AD), died by suicide to end the torment.
Patients would also pray to the gods for hope of a cure. An example of this is Innocentia, an aristocratic lady who lived in Carthage (in modern-day Tunisia) in the fifth century AD. She told her doctor divine intervention had cured her breast cancer, though her doctor did not believe her.
Innocentia from Carthage, in modern-day Tunisia, believed divine intervention cured her breast cancer. Valery Bareta/Shutterstock From the past into the future
We began with Satyrus, a tyrant in the fourth century BC. In the 2,400 years or so since then, much has changed in our knowledge of what causes cancer, how to prevent it and how to treat it. We also know there are more than 200 different types of cancer. Some people’s cancers are so successfully managed, they go on to live long lives.
But there is still no general “cure for cancer”, a disease that about one in five people develop in their lifetime. In 2022 alone, there were about 20 million new cancer cases and 9.7 million cancer deaths globally. We clearly have a long way to go.
Konstantine Panegyres, McKenzie Postdoctoral Fellow, Historical and Philosophical Studies, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: