Get The Right Help For Your Pain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How Much Does It Hurt?
Sometimes, a medical professional will ask us to “rate your pain on a scale of 1–10”.
It can be tempting to avoid rating one’s pain too highly, because if we say “10” then where can we go from there? There is always a way to make pain worse, after all.
But that kind of thinking, however logical, is folly—from a practical point of view. Instead of risking having to give an 11 later, you have now understated your level-10 pain as a “7” and the doctor thinks “ok, I’ll give Tylenol instead of morphine”.
A more useful scale
First, know this:
Zero is not “this is the lowest level of pain I get to”.
Zero is “no pain”.
As for the rest…
- My pain is hardly noticeable.
- I have a low level of pain; I am aware of my pain only when I pay attention to it.
- My pain bothers me, but I can ignore it most of the time.
- I am constantly aware of my pain, but can continue most activities.
- I think about my pain most of the time; I cannot do some of the activities I need to do each day because of the pain.
- I think about my pain all of the time; I give up many activities because of my pain.
- I am in pain all of the time; It keeps me from doing most activities.
- My pain is so severe that it is difficult to think of anything else. Talking and listening are difficult.
- My pain is all that I can think about; I can barely move or talk because of my pain.
- I am in bed and I can’t move due to my pain; I need someone to take me to the emergency room because of my pain.
10almonds tip: are you reading this on your phone? Screenshot the above, and keep it for when you need it!
One extra thing to bear in mind…
Medical staff will be more likely to believe a pain is being overstated, on a like-for-like basis, if you are a woman, or not white, or both.
There are some efforts to compensate for this:
A new government inquiry will examine women’s pain and treatment. How and why is it different?
Some other resources of ours:
- The 7 Approaches To Pain Management ← a pain specialist discusses the options available
- Managing Chronic Pain (Realistically!) ← when there’s no quick fix, but these things can buy you some hours’ relief at least / stop the pain from getting worse in the moment
- Science-Based Alternative Pain Relief ← for when you’re maxxed out on painkillers, and need something more/different, these are the things the science says will work
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cannabis & Heart Attacks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For many, cannabis use has taken the place that alcohol used to have when it comes to wanting a “downer”, that is to say, a drug that relaxes us as opposed to stimulating us.
Indeed, it is generally considered safer than alcohol ← however this is not a strong claim, because alcohol is much more dangerous than one would think given its ubiquity and (in many places, at least) social acceptability.
We’ve talked a bit about cannabis use before, in its various forms, for example:
Cannabis Myths vs Reality ← a very good starting point for the curious
And one specifically about the use of THC gummies (THC is the psychoactive compound in cannabis, i.e. it’s the chemical that gets people high, as opposed to CBD, which is not psychoactive) as a sleep aid:
Sweet Dreams Are Made of THC (Or Are They?)
And for those skipping the THC, we’ve also written about CBD use, including:
CBD Oil: What Does The Science Say? and Do CBD Gummies Work?
So, about cannabis and heart attacks
Alcohol is a relaxant, and yet it can contribute to heart disease (amongst many other things, of course):
Can We Drink To Good Health? ← this is mostly about red wine’s putative heart health benefits, how the idea got popularized, and how it doesn’t stand up to scrutiny when actually looking at the evidence.
And cannabis, another relaxant? Not so good either!
New research has shown that cannabis users have a higher risk of heart attacks, even among younger and otherwise healthy individuals. This is based on analyzing data from 4,636,628 relatively healthy adults.
Specifically, the data showed that even young healthy cannabis users get:
- Sixfold increased risk of heart attack
- Fourfold increased risk of ischemic stroke
- Threefold increased risk of cardiovascular death, heart attack, or stroke
We mention the otherwise “relatively healthy” nature of the participants, because it’s important to note that less healthy people (who were perhaps using cannabis to self-medicate for some serious condition) were not included in the dataset, as it’d skew the data unhelpfully and it’d make the risk look a lot higher than the risk levels we mentioned above.
The mechanisms by which cannabis affects heart health are not fully understood, but hypotheses include:
- Disrupting heart rhythm regulation
- Increasing oxygen demand in the heart muscle
- Causing endothelial dysfunction, which affects blood vessel function
Further, heart attack risk peaked one hour after cannabis use, and while this doesn’t prove causality, it certainly doesn’t make cannabis look safe.
You can read the paper in its entirety here:
Want a safer way to relax?
We recommend:
- No-Frills, Evidence-Based Mindfulness
- Meditation Games That You’ll Actually Enjoy
- Which Style Of Yoga Is Best For You?
- 7 Kinds Of Rest When Sleep Is Not Enough
- Better Sex = Longer Life (Here’s How)
Enjoy!
Share This Post
-
Mango vs Pineapple – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing mango to pineapple, we picked the pineapple.
Why?
It was close! Both of these tropical fruits have almost identical macros, and when it comes to vitamins and minerals, mango has slightly more vitamins while pineapple has slightly more minerals, so that balances out too. Their glycemic loads are 11 and 13 respectively, so: very low, and very similar.
See also: Which Sugars Are Healthier, And Which Are Just The Same?
In terms of what sets them apart:
Mango has a lot of vitamin A, to the point that it can interfere with blood-thinners if you take those.
Pineapple has bromelain, an enzyme with unique anti-inflammatory properties that we must devote a Research Review Monday to one of these days, because there’s a lot to say, but the short version is, it’s very powerful.
Since bromelain is found only in pineapples, whereas vitamin A is easy to find in abundance in many foods, we went with the pineapple.
Enjoy!
Share This Post
-
How a Michigan community center supports young people’s mental health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Even before the COVID-19 pandemic made mental health problems worse for people of all ages, young people already struggled with a lack of support and treatment for issues like depression, anxiety, and ADHD.
Like many states, Michigan doesn’t have enough health care providers, and youth mental health professionals are in high demand.
Some local groups step in to support kids when they aren’t getting the help they need or experience long wait times for services.
To learn more about how one community-based organization tackles these challenges, Public Good News spoke with Avion Williams, Youth Coordinator at Community Family Life Center.
Here’s what she said.
[Editor’s note: The contents of this interview have been edited for length and clarity.]
Public Good News: Can you tell us more about your organization and where you’re located?
A.W.: Community Family Life Center is a community outreach center. We offer a multitude of after-school programs and services to Ypsilanti-Ann Arbor and even the Belleville community.
Ypsilanti is a small community. It was originally a farmer’s town. You will still see a lot of older families here.
A lot of our restaurants are like mom-and-pop shops. We have our downtown area, which is now being modernized a little bit, but again, a lot of shops are family-owned businesses that have been around for decades.
We have a lot of colleges. We have Eastern Michigan, which is the college I actually attend, and that’s in Ypsilanti. But we also have colleges right next door that are 10 minutes away, like University of Michigan and Concordia.
So it’s a college town, very family-oriented, but also a very small town with not too many resources.
PGN: Can you share some of your experiences as a youth coordinator trying to help young people access your organization’s services and programs?
A.W.: So we offer a ton of different programs, but our main focus is for kids to have something to do. There’s definitely a lot of young people in Ypsilanti.
I’m 25, and when I was in high school, a lot of people in my grade were having children. And they weren’t just having one baby, they were having multiple babies. You know, maybe one in tenth grade, another when we graduated our senior year, another right after. So a lot of people my age have a lot of children. And now I work with a lot of their children.
Many of those children come to after-school programs, and they’re in need of not just school things like math and reading, but they’re in need of, you know, love and care. Maybe mom can’t do everything because she has to work two or three jobs, or she doesn’t have the best financial help, and so she doesn’t know what to do.
And these young children get stuck with teachers that may not necessarily know how to give the best support, because maybe they’re stressed.
We have after-school programs and community centers like ours, where we get all of that.
Not only do we have to deal with mental health, we have to deal with these babies being hungry. We have to teach what mental health is.
PGN: What about therapy? How does that fit into the picture?
A.W.: Sometimes in society, people just throw therapy out there, like, ‘Go to therapy, go to therapy, go to therapy,’ but they don’t talk about the process of what it’s like getting a therapist.
I love the idea of therapy. Don’t get me wrong. Having somebody to talk to is very real. Having the right person to talk to is very real, right?
But I think sometimes we don’t talk about how everybody is not able to get therapy.
And a lot of times when people are ready for therapy, it’s after everything has happened.
You know, ‘Mom is gone, dad is gone. I’m doing terribly in school now. I’m acting out. Now I’m lashing out. I’m super hungry. I don’t have money for this. I don’t have money for that. I don’t know what to do about this…’ and then it’s like, ‘okay, I think I need therapy.’
Instead of us approaching it as, ‘Hey, this person’s mom is a young mom, maybe we should see if we can get therapy for both of them.’ Or when that child is being born, or when we see this young mom at the hospital and we see that she’s pregnant. Let’s offer some help before things start to hit the fan, right?
And maybe this mom doesn’t even have the proper health care to receive therapy, or let alone, doesn’t have the money to pay for it.
PGN: How does your organization respond to this need?
A.W.: We have a lot of ways to access our therapists. We started maybe two years ago, and at first a lot of people weren’t going. And now there’s so many people going that yes, we have this wait list.
So we also all do daily check-ins with our kids. We really do get to know our kids and their families and have consistent conversations with parents.
I always tell my kids this is a safe space to talk. I’m open to hear anything my students have to say.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
What happens in my brain when I get a migraine? And what medications can I use to treat it?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Migraine is many things, but one thing it’s not is “just a headache”.
“Migraine” comes from the Greek word “hemicrania”, referring to the common experience of migraine being predominantly one-sided.
Some people experience an “aura” preceding the headache phase – usually a visual or sensory experience that evolves over five to 60 minutes. Auras can also involve other domains such as language, smell and limb function.
Migraine is a disease with a huge personal and societal impact. Most people cannot function at their usual level during a migraine, and anticipation of the next attack can affect productivity, relationships and a person’s mental health.
Francisco Gonzelez/Unsplash What’s happening in my brain?
The biological basis of migraine is complex, and varies according to the phase of the migraine. Put simply:
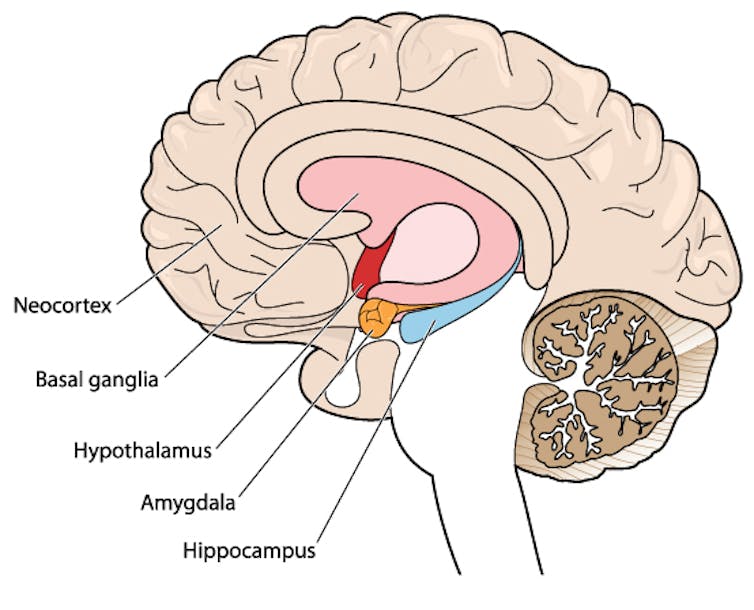
The earliest phase is called the prodrome. This is associated with activation of a part of the brain called the hypothalamus which is thought to contribute to many symptoms such as nausea, changes in appetite and blurred vision.
The hypothalamus is shown here in red. Blamb/Shutterstock Next is the aura phase, when a wave of neurochemical changes occur across the surface of the brain (the cortex) at a rate of 3–4 millimetres per minute. This explains how usually a person’s aura progresses over time. People often experience sensory disturbances such as flashes of light or tingling in their face or hands.
In the headache phase, the trigeminal nerve system is activated. This gives sensation to one side of the face, head and upper neck, leading to release of proteins such as CGRP (calcitonin gene-related peptide). This causes inflammation and dilation of blood vessels, which is the basis for the severe throbbing pain associated with the headache.
Finally, the postdromal phase occurs after the headache resolves and commonly involves changes in mood and energy.
What can you do about the acute attack?
A useful way to conceive of migraine treatment is to compare putting out campfires with bushfires. Medications are much more successful when applied at the earliest opportunity (the campfire). When the attack is fully evolved (into a bushfire), medications have a much more modest effect.
Aspirin
For people with mild migraine, non-specific anti-inflammatory medications such as high-dose aspirin, or standard dose non-steroidal medications (NSAIDS) can be very helpful. Their effectiveness is often enhanced with the use of an anti-nausea medication.
Triptans
For moderate to severe attacks, the mainstay of treatment is a class of medications called “triptans”. These act by reducing blood vessel dilation and reducing the release of inflammatory chemicals.
Triptans vary by their route of administration (tablets, wafers, injections, nasal sprays) and by their time to onset and duration of action.
The choice of a triptan depends on many factors including whether nausea and vomiting is prominent (consider a dissolving wafer or an injection) or patient tolerability (consider choosing one with a slower onset and offset of action).
As triptans constrict blood vessels, they should be used with caution (or not used) in patients with known heart disease or previous stroke.
Triptans should be used cautiously in patients with heart disease. CDC/Unsplash Gepants
Some medications that block or modulate the release of CGRP, which are used for migraine prevention (which we’ll discuss in more detail below), also have evidence of benefit in treating the acute attack. This class of medication is known as the “gepants”.
Gepants come in the form of injectable proteins (monoclonal antibodies, used for migraine prevention) or as oral medication (for example, rimegepant) for the acute attack when a person has not responded adequately to previous trials of several triptans or is intolerant of them.
They do not cause blood vessel constriction and can be used in patients with heart disease or previous stroke.
Ditans
Another class of medication, the “ditans” (for example, lasmiditan) have been approved overseas for the acute treatment of migraine. Ditans work through changing a form of serotonin receptor involved in the brain chemical changes associated with the acute attack.
However, neither the gepants nor the ditans are available through the Pharmaceutical Benefits Scheme (PBS) for the acute attack, so users must pay out-of-pocket, at a cost of approximately A$300 for eight wafers.
What about preventing migraines?
The first step is to see if lifestyle changes can reduce migraine frequency. This can include improving sleep habits, routine meal schedules, regular exercise, limiting caffeine intake and avoiding triggers such as stress or alcohol.
Despite these efforts, many people continue to have frequent migraines that can’t be managed by acute therapies alone. The choice of when to start preventive treatment varies for each person and how inclined they are to taking regular medication. Those who suffer disabling symptoms or experience more than a few migraines a month benefit the most from starting preventives.
Some people will take medicines to prevent migraines. Tbel Abuseridze/Unsplash Almost all migraine preventives have existing roles in treating other medical conditions, and the physician would commonly recommend drugs that can also help manage any pre-existing conditions. First-line preventives include:
- tablets that lower blood pressure (candesartan, metoprolol, propranolol)
- antidepressants (amitriptyline, venlafaxine)
- anticonvulsants (sodium valproate, topiramate).
Some people have none of these other conditions and can safely start medications for migraine prophylaxis alone.
For all migraine preventives, a key principle is starting at a low dose and increasing gradually. This approach makes them more tolerable and it’s often several weeks or months until an effective dose (usually 2- to 3-times the starting dose) is reached.
It is rare for noticeable benefits to be seen immediately, but with time these drugs typically reduce migraine frequency by 50% or more.
‘Nothing works for me!’
In people who didn’t see any effect of (or couldn’t tolerate) first-line preventives, new medications have been available on the PBS since 2020. These medications block the action of CGRP.
The most common PBS-listed anti-CGRP medications are injectable proteins called monoclonal antibodies (for example, galcanezumab and fremanezumab), and are self-administered by monthly injections.
These drugs have quickly become a game-changer for those with intractable migraines. The convenience of these injectables contrast with botulinum toxin injections (also effective and PBS-listed for chronic migraine) which must be administered by a trained specialist.
Up to half of adolescents and one-third of young adults are needle-phobic. If this includes you, tablet-form CGRP antagonists for migraine prevention are hopefully not far away.
Data over the past five years suggest anti-CGRP medications are safe, effective and at least as well tolerated as traditional preventives.
Nonetheless, these are used only after a number of cheaper and more readily available first-line treatments (all which have decades of safety data) have failed, and this also a criterion for their use under the PBS.
Mark Slee, Associate Professor, Clinical Academic Neurologist, Flinders University and Anthony Khoo, Lecturer, Flinders University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Your Vitamins are Obsolete: The Vitamer Revolution – by Dr. Sheldon Zablow
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this is not:a book to tell you “throw out your vitamins and just eat these foods”.
This book focuses mainly on two vitamins in which deficiencies are common especially as we get older: B9 and B12.
So, what does the title mean? It’s not so much that your vitamins are obsolete—that would imply that they were more useful previously, which is not the case. Rather, the most common forms of vitamins B9 and B12 provided in supplements are folic acid and cyanocobalamin, respectively, which as he demonstrates with extensive research to back up his claims, cannot be easily absorbed or used especially well.
About those vitamers: a vitamer is simply a form of a vitamin—most vitamins we need can arrive in a variety of forms. In the case of vitamins B9 and B12, he advocates for ditching vitamers folic acid and cyanocobalamin, cheap as they are, and springing for bioactive vitamers L-methylfolate, methylcobalamin, and adenosylcobalamin.
He also discusses (again, just as well-evidenced as the above things) why we might struggle to get enough from our diet after a certain age. For example, if trying to get these vitamins from meat, 50% of people over 50 cannot manufacture enough stomach acid to break down that protein to release the vitamins.
And as for methyl-B12 vitamers, you might expect you can get those from meat, and technically you can, but they don’t occur in all animals, just in one kind of animal. Specifically, the kind that has the largest brain-to-body ratio. However, eating the meat of this animal can result in protein folding errors in general and Creutzfeldt–Jakob disease in particular, so the author does not recommend eating humans, however nutritionally convenient that would be.
All this means that supplementation after a certain age really can be a sensible way to do it—but do it wisely, and pick the right vitamers.
The style of the book is informationally dense, but very readable even for a layperson provided one starts at the beginning and reads forwards, as otherwise one will find oneself in a mire of terms whose explanations one missed when they were first introduced.
Bottom line: if you are over 50 and/or have any known or suspected issues with vitamins B9 and/or B12, this book becomes very important reading.
Click here to check out Your Vitamins Are Obsolete, and get your body what it needs!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Grains: Bread Of Life, Or Cereal Killer?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Going Against The Grain?
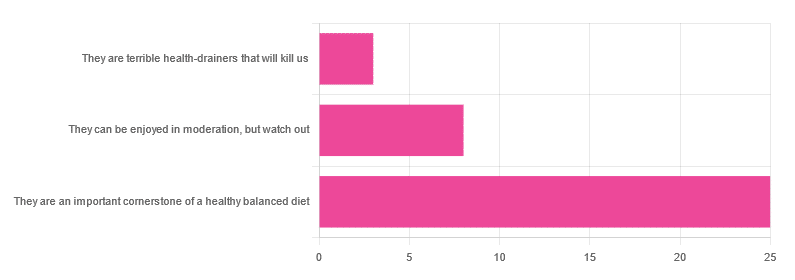
In Wednesday’s newsletter, we asked you for your health-related opinion of grains (aside from any gluten-specific concerns), and got the above-depicted, below-described, set of responses:
- About 69% said “They are an important cornerstone of a healthy balanced diet”
- About 22% said “They can be enjoyed in moderation, but watch out”
- About 8% said “They are terrible health-drainers that will kill us”
So, what does the science say?
They are terrible health-drainers that will kill us: True or False?
True or False depending on the manner of their consumption!
There is a big difference between the average pizza base and a bowl of oats, for instance. Or rather, there are a lot of differences, but what’s most critical here?
The key is: refined and ultraprocessed grains are so inferior to whole grains as to be actively negative for health in most cases for most people most of the time.
But! It’s not because processing is ontologically evil (in reality: some processed foods are healthy, and some unprocessed foods are poisonous). although it is a very good general rule of thumb.
So, we need to understand the “why” behind the “key” that we just gave above, and that’s mostly about the resultant glycemic index and associated metrics (glycemic load, insulin index, etc).
In the case of refined and ultraprocessed grains, our body gains sugar faster than it can process it, and stores it wherever and however it can, like someone who has just realised that they will be entertaining a houseguest in 10 minutes and must tidy up super-rapidly by hiding things wherever they’ll fit.
And when the body tries to do this with sugar from refined grains, the result is very bad for multiple organs (most notably the liver, but the pancreas takes quite a hit too) which in turn causes damage elsewhere in the body, not to mention that we now have urgently-produced fat stored in unfortunate places like our liver and abdominal cavity when it should have gone to subcutaneous fat stores instead.
In contrast, whole grains come with fiber that slows down the absorption of the sugars, such that the body can deal with them in an ideal fashion, which usually means:
- using them immediately, or
- storing them as muscle glycogen, or
- storing them as subcutaneous fat
👆 that’s an oversimplification, but we only have so much room here.
For more on this, see:
Glycemic Index vs Glycemic Load vs Insulin Index
And for why this matters, see:
Which Sugars Are Healthier, And Which Are Just The Same?
And for fixing it, see:
They can be enjoyed in moderation, but watch out: True or False?
Technically True but functionally False:
- Technically true: “in moderation” is doing a lot of heavy lifting here. One person’s “moderation” may be another person’s “abstemiousness” or “gluttony”.
- Functionally false: while of course extreme consumption of pretty much anything is going to be bad, unless you are Cereals Georg eating 10,000 cereals each day and being a statistical outlier, the issue is not the quantity so much as the quality.
Quality, we discussed above—and that is, as we say, paramount. As for quantity however, you might want to know a baseline for “getting enough”, so…
They are an important cornerstone of a healthy balanced diet: True or False?
True! This one’s quite straightforward.
3 servings (each being 90g, or about ½ cup) of whole grains per day is associated with a 22% reduction in risk of heart disease, 5% reduction in all-cause mortality, and a lot of benefits across a lot of disease risks:
❝This meta-analysis provides further evidence that whole grain intake is associated with a reduced risk of coronary heart disease, cardiovascular disease, and total cancer, and mortality from all causes, respiratory diseases, infectious diseases, diabetes, and all non-cardiovascular, non-cancer causes.
These findings support dietary guidelines that recommend increased intake of whole grain to reduce the risk of chronic diseases and premature mortality.❞
~ Dr. Dagfinn Aune et al.
We’d like to give a lot more sources for the same findings, as well as papers for all the individual claims, but frankly, there are so many that there isn’t room. Suffice it to say, this is neither controversial nor uncertain; these benefits are well-established.
Here’s a very informative pop-science article, that also covers some of the things we discussed earlier (it shows what happens during refinement of grains) before getting on to recommendations and more citations for claims than we can fit here:
Harvard School Of Public Health | Whole Grains
“That’s all great, but what if I am concerned about gluten?”
There certainly are reasons you might be, be it because of a sensitivity, allergy, or just because perhaps you’d like to know more.
Let’s first mention: not all grains contain gluten, so it’s perfectly possible to enjoy naturally gluten-free grains (such as oats and rice) as well as gluten-free pseudocereals, which are not actually grains but do the same job in culinary and nutritional terms (such as quinoa and buckwheat, despite the latter’s name).
Finally, if you’d like to know more about gluten’s health considerations, then check out our previous mythbusting special:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: