Oral retinoids can harm unborn babies. But many women taking them for acne may not be using contraception
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Oral retinoids are a type of medicine used to treat severe acne. They’re sold under the brand name Roaccutane, among others.
While oral retinoids are very effective, they can have harmful effects if taken during pregnancy. These medicines can cause miscarriages and major congenital abnormalities (harm to unborn babies) including in the brain, heart and face. At least 30% of children exposed to oral retinoids in pregnancy have severe congenital abnormalities.
Neurodevelopmental problems (in learning, reading, social skills, memory and attention) are also common.
Because of these risks, the Australasian College of Dermatologists advises oral retinoids should not be prescribed a month before or during pregnancy under any circumstances. Dermatologists are instructed to make sure a woman isn’t pregnant before starting this treatment, and discuss the risks with women of childbearing age.
But despite this, and warnings on the medicines’ packaging, pregnancies exposed to oral retinoids continue to be reported in Australia and around the world.
In a study published this month, we wanted to find out what proportion of Australian women of reproductive age were taking oral retinoids, and how many of these women were using contraception.
Our results suggest a high proportion of women are not using effective contraception while on these drugs, indicating Australia needs a strategy to reduce the risk oral retinoids pose to unborn babies.
Contraception options
Using birth control to avoid pregnancy during oral retinoid treatment is essential for women who are sexually active. Some contraception methods, however, are more reliable than others.
Long-acting-reversible contraceptives include intrauterine devices (IUDs) inserted into the womb (such as Mirena, Kyleena, or copper devices) and implants under the skin (such as Implanon). These “set and forget” methods are more than 99% effective.

The effectiveness of oral contraceptive pills among “perfect” users (following the directions, with no missed or late pills) is similarly more than 99%. But in typical users, this can fall as low as 91%.
Condoms, when used as the sole method of contraception, have higher failure rates. Their effectiveness can be as low as 82% in typical users.
Oral retinoid use over time
For our study, we analysed medicine dispensing data among women aged 15–44 from Australia’s Pharmaceutical Benefit Scheme (PBS) between 2013 and 2021.
We found the dispensing rate for oral retinoids doubled from one in every 71 women in 2013, to one in every 36 in 2021. The increase occurred across all ages but was most notable in young women.
Most women were not dispensed contraception at the same time they were using the oral retinoids. To be sure we weren’t missing any contraception that was supplied before the oral retinoids, we looked back in the data. For example, for an IUD that lasts five years, we looked back five years before the oral retinoid prescription.
Our analysis showed only one in four women provided oral retinoids were dispensed contraception simultaneously. This was even lower for 15- to 19-year-olds, where only about one in eight women who filled a prescription for oral retinoids were dispensed contraception.
A recent study found 43% of Australian year 10 and 69% of year 12 students are sexually active, so we can’t assume this younger age group largely had no need for contraception.
One limitation of our study is that it may underestimate contraception coverage, because not all contraceptive options are listed on the PBS. Those options not listed include male and female sterilisation, contraceptive rings, condoms, copper IUDs, and certain oral contraceptive pills.
But even if we presume some of the women in our study were using forms of contraception not listed on the PBS, we’re still left with a significant portion without evidence of contraception.
What are the solutions?
Other countries such as the United States and countries in Europe have pregnancy prevention programs for women taking oral retinoids. These programs include contraception requirements, risk acknowledgement forms and regular pregnancy tests. Despite these programs, unintended pregnancies among women using oral retinoids still occur in these countries.
But Australia has no official strategy for preventing pregnancies exposed to oral retinoids. Currently oral retinoids are prescribed by dermatologists, and most contraception is prescribed by GPs. Women therefore need to see two different doctors, which adds costs and burden.

Rather than a single fix, there are likely to be multiple solutions to this problem. Some dermatologists may not feel confident discussing sex or contraception with patients, so educating dermatologists about contraception is important. Education for women is equally important.
A clinical pathway is needed for reproductive-aged women to obtain both oral retinoids and effective contraception. Options may include GPs prescribing both medications, or dermatologists only prescribing oral retinoids when there’s a contraception plan already in place.
Some women may initially not be sexually active, but change their sexual behaviour while taking oral retinoids, so constant reminders and education are likely to be required.
Further, contraception access needs to be improved in Australia. Teenagers and young women in particular face barriers to accessing contraception, including costs, stigma and lack of knowledge.
Many doctors and women are doing the right thing. But every woman should have an effective contraception plan in place well before starting oral retinoids. Only if this happens can we reduce unintended pregnancies among women taking these medicines, and thereby reduce the risk of harm to unborn babies.
Dr Laura Gerhardy from NSW Health contributed to this article.
Antonia Shand, Research Fellow, Obstetrician, University of Sydney and Natasha Nassar, Professor of Paediatric and Perinatal Epidemiology and Chair in Translational Childhood Medicine, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Carrots vs Parsnips – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing carrots to parsnips, we picked the parsnips.
Why?
There are arguments for both! But we say parsnips win on overall nutritional density.
In terms of macros, parsnips vary quite a lot from region to another, but broadly speaking, parsnips have more carbs and fiber, and/but the ratios are such that carrots have the lower glycemic index. We’ll call this one a win for carrots.
When it comes to vitamins, carrots have more of vitamins A, B2, B3, B6, and choline, while parsnips have more of vitamins B1, B5, B9, C, E, and K. A small win for parsnips here.
In the category of minerals, carrots are not higher in any minerals, while parsnips are higher in calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. An overwhelming win for parsnips.
While the overall vitamin and mineral content puts parsnips ahead, it’s still worth noting that carrots have highly bioavailable megadoses of vitamin A.
Another thing to note is that the glycemic index recorded for both is when peeled and boiled, whereas both of these root vegetables can be enjoyed raw if you wish, which has a much lower GI.
In short, enjoy either or both, but parsnips are the more nutritionally dense overall.
Want to learn more?
You might like to read:
Glycemic Index vs Glycemic Load vs Insulin Index
Take care!
Share This Post
-
Science-backed ways to take care of your mental health this winter
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The colder, darker months can take a toll on well-being. Two out of five U.S. adults say their mental health worsens in the winter. Plus, about five percent of U.S. adults experience seasonal affective disorder (SAD), a type of depression induced by seasonal changes that typically begins when the weather gets colder and there’s less daylight.
Fortunately, there are science-backed lifestyle changes that can make this time of year more tolerable. Here’s how to take care of your mental health this winter.
Exercise regularly
When you exercise, your body releases endorphins, or “feel-good” chemicals that can improve your mood. A 2024 review of studies found that exercise—particularly walking, jogging, yoga, and strength training—can reduce symptoms of depression.
Before starting a new exercise routine, talk to your health care provider about the types of exercise that may work best for you.
Get outside
While getting outside during the colder months may feel challenging, time outdoors—especially in nature—has been shown to decrease stress, depression, and anxiety. Plus, sunlight helps your body make vitamin D, which may improve your energy and mood.
You can reap the benefits of nature no matter where you live.
“Cities can be very energetic and exciting but also can contribute to both conscious and unconscious stress from the sensory overload and challenges of maneuvering in those spaces,” said Jodie M. Smith, a Mayo Clinic nurse practitioner, in a 2024 Mayo Clinic article. “If you live in an urban environment, exploring to find even a small natural reprieve can be extremely beneficial.”
Prioritize sleep
Inadequate sleep has been linked to depression and anxiety. Taking steps to improve the quality and duration of your sleep can help you become more resilient against stressors.
You can improve your sleep by going to bed and waking up at the same time every day; avoiding caffeine, alcohol, and large meals before bed; keeping your bedroom cool and dark; and limiting exposure to distressing media in the evening.
Practice gratitude
Research suggests that people who practice gratitude are less likely to experience depression. It can also help you make lifestyle changes that improve your well-being overall.
“Practicing gratitude may also make someone a bit more motivated to take care of their health,” said Tyler VanderWeele, co-director of the Initiative on Health, Spirituality, and Religion at the Harvard T.H. Chan School of Public Health, in a 2024 Harvard Health Publishing article. “Maybe they’re more likely to show up for medical appointments or exercise. It may also help with relationships and social support, which we know contribute to health.”
Add more gratitude to your life by sharing what you’re grateful for with others or keeping a gratitude journal.
Spend quality time with loved ones
“Social isolation and loneliness have a serious impact on physical and mental health, quality of life, and longevity,” according to the World Health Organization, with effects comparable to other risk factors like smoking.
Research shows that people who have close confidants are more satisfied with their lives and less likely to experience depression. Even after holiday gatherings have ended, schedule time with friends and family to stay positive and feel supported.
Limit cell phone use
Social media use and “doomscrolling” inflammatory news headlines are both associated with anxiety and depression across age groups, especially in teens.
“Excessive social media use is associated with behaviors, such as poor sleep, increased social comparisons, impact on learning, and exposure to cyberbullying and negative content, that could contribute to the worsening of depressive symptoms,” Dr. Carol Vidal, an assistant professor of psychiatry and behavioral sciences at the Johns Hopkins University School of Medicine, said in a Hopkins Medicine article.
Minimize the time you and your family members spend on your phones by pausing notifications, keeping your phone out of reach when you’re preparing for sleep, using a “grayscale” setting to make scrolling less enticing, and finding phone-free hobbies to enjoy.
Light therapy
Light therapy is one treatment for people who have been diagnosed with SAD. It involves sitting in front of a bright light box for 30 to 45 minutes per day to increase light exposure.
This treatment may not be right for people who take certain medications or have eye diseases. Talk to your health care provider about whether light therapy is right for you and what type of light box you should use.
Seek professional support
If your mental health over the winter interferes with your daily functioning, seek help from a therapist, support group, or mental health hotline. Find resources here.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Share This Post
-
Artichoke vs Heart of Palm– Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing artichoke to heart of palm, we picked the artichoke.
Why?
If you were thinking “isn’t heart of palm full of saturated fat?” then no… Palm oil is, but heart of palm itself has 0.62g/100g fat, of which, 0.13g saturated fat. So, negligible.
As for the rest of the macros, artichoke has more protein, carbs, and fiber, thus being the “more food per food” option. Technically heart of palm has the lower glycemic index, but they are both low-GI foods, so it’s really not a factor here.
Vitamins are where artichoke shines; artichoke has more of vitamins A, B1, B2, B3, B5, B6, B9, C, E, K, and choline, while heart of palm is not higher in any vitamins.
The minerals situation is more balanced: artichoke has more copper, magnesium, phosphorus, and potassium, while heart of palm has more iron, manganese, selenium, and zinc.
Adding up the categories, the winner of this “vegetables with a heart” face-off is clearly artichoke.
Fun fact: in French, “to have the heart of an artichoke” (avoir le coeur d’un artichaut) means to fall in love easily. Perfect vegetable for a romantic dinner, perhaps (especially with all those generous portions of B-vitamins)!
Want to learn more?
You might like to read:
Artichoke vs Cabbage – Which is Healthier?
Take care!
Share This Post
Related Posts
-
How Are You, Really?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How Are You, Really? The Free NHS Health Test
We took this surprisingly incisive 10-minute test from the UK’s famous National Health Service—the test is part of the “Better Health” programme, a free-to-all (yes, even those from/in other countries) initiative aimed at keeping people healthy enough to have less need of medical attention.
As one person who took the test wrote:
❝I didn’t expect that a government initiative would have me talking about how I need to keep myself going to be there for the people I love, let alone that a rapid-pace multiple-choice test would elicit these responses and give personalized replies in turn, but here we are❞
It goes beyond covering the usual bases, in that it also looks at what’s most important to you, and why, and what might keep you from doing the things you want/need to do for your health, AND how those obstacles can be overcome.
Pretty impressive for a 10-minute test!
Is Your Health Above Average Already? Take the Free 10-minute NHS test now!
How old are you, in your heart?
Poetic answers notwithstanding (this writer sometimes feels so old, and yet also much younger than she is), there’s a biological answer here, too.
Again free for the use of all*, here’s a heart age calculator.
*It is suitable for you if you are aged 30–95, and do not have a known complicating cardiovascular disease.
It will ask you your (UK) postcode; just leave that field blank if you’re not in the UK; it’ll be fine.
How Old Are You, In Your Heart? Take the Free 10-minute NHS test now!
(Neither test requires logging into anything, and they do not ask for your email address. The tests are right there on the page, and they give the answers right there on the page, immediately)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
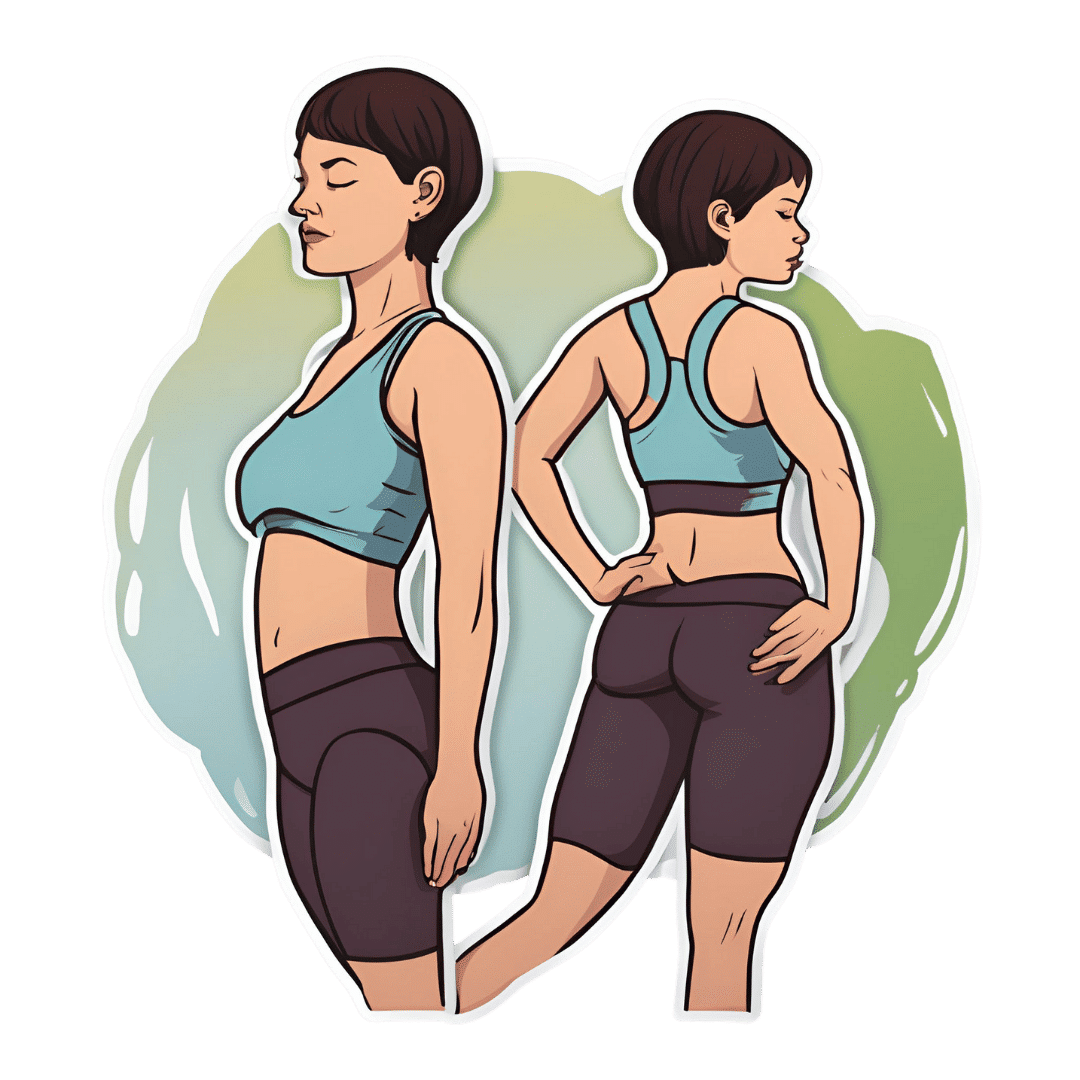
5 Minute Posture Improvement Routine!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
McKay Lang walks us through it:
Step by Step
Breathing exercise:
- Place your hands on your lower abdomen.
- Take three deep breaths, focusing on body tension in the shoulders and neck… And release.
Shoulder squeeze:
- With your hands on your hips, inhale and squeeze your shoulders upwards.
- Hold your breath for 3–4 seconds, then exhale.
- Repeat two more times, holding the squeeze a little longer each time.
Upper shoulder massage:
- Massage your upper shoulder muscles to release tension stored there.
Overhead arm stretch:
- Raise your arms above your head, clasping each elbow with the opposite hand.
- Inhale deeply, stretch upwards, then exhale and release.
- Repeat, alternating elbows.
Neck and head push:
- Place your palms on the back of the head, and push your head into your hands (and vice versa, because of Newton’s Third Law of Motion).
- Do the same sideways (one side and then the other), to engage the other neck muscles.
Cool down:
- Gently unclasp your hands, bring your head upright, and massage your muscles. And breathe.
For variations and a visual demonstration of all, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
6 Ways To Look After Your Back
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Does Music Really Benefit The Brain?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝Is it actually beneficial for the brain to listen to music, or is it just in line with any relaxing activity? And what kind of music is most beneficial❞
The short answer, first of all, is that it is indeed beneficial.
One reason for this without having to get very deep into it, is that a very important thing for general brain health is using it, and that means lighting up all areas of your brain.
Now, we all lead different lives and thus different parts of our brains will get relatively more resources than others depending on what we do with them, and that’s ok.
For example, if you were to scan this writer’s polyglot brain, you’d surely find overdevelopment in areas associated with language use and verbal memory, but if you were to scan a taxi-driver’s brain, then it’d be spatial reasoning and spatial memory that’s overpowered, and for a visual artist, it may be visual processing and creativity that’s enhanced. A musician’s brain? Fine motor skills, auditory processing, auditory memory.
Now, for those of us who aren’t musicians, how then can we light up areas associated with music? By listening to music, of course. It won’t give us the fine motor skills of a concert violinist, but the other areas we mentioned will get a boost.
See also: How To Engage Your Whole Brain ← this covers music too, but it’s about (as the title suggests) the whole brain, so check it out and see if there are any areas you’ve been neglecting!
There are other benefits too, though, including engaging our parasympathetic nervous system, which is good for our heart, gut, brain, and general health—especially if we sing or hum along to the music:
The Science Of Sounds ← this also covers the science (yes, science) of mantra meditation vs music
As for “and what kind of music is most beneficial”, we’d hypothesize that a variety is best, just like with food!
However, there are some considerations to bear in mind, with science to support them. For example…
About tempo:
❝EEG analysis revealed significant changes in brainwave signals across different frequency bands under different tempi.
For instance, slow tempo induced higher Theta and Alpha power in the frontal region, while fast tempo increased Beta and Gamma band power.
Moreover, fast tempo enhanced the average connectivity strength in the frontal, temporal, and occipital regions, and increased phase synchrony value (PLV) between the frontal and parietal regions.❞
Read in full: Music tempo modulates emotional states as revealed through EEG insights
And if you’re wondering about those different brainwave bands, check out:
- How to get many benefits of sleep, while awake! Non-Sleep Deep Rest: A Neurobiologist’s Take ← although it’s not in the title, this does also cover the different brain wave bands
- Alpha, beta, theta: what are brain states and brain waves? And can we control them?
Additionally, if you just want science-backed relaxation, the following 8-minute soundscape was developed by sound technicians working with a team of psychologists and neurologists.
It’s been clinically tested, and found to have a much more relaxing effect (in objective measures of lowering heart rate and lowering cortisol levels, as well as in subjective self-reports) than merely “relaxing music”.
Try it and see for yourself:
Click Here If The Embedded Video Doesn’t Load Automatically!
For much deeper dive into the effect of music on the brain, check out this book we reviewed a while back, by an accomplished musician and neuroscientist (that’s one person, who is both things):
This Is Your Brain on Music – by Dr. Daniel Levitin
Enjoy!
And now for a bonus item…
A s a bit of reader feedback prompted some interesting thoughts:
❝You erred on the which is better section. Read this carefully :Looking at minerals, grapes have more calcium, copper, iron, magnesium, phosphorus, selenium, and zinc, while grapes have more potassium and manganese. A clear win for strawberries here.❞
You’re quite right; thank you for pointing it out, and kindly pardon the typo, which has now been corrected!
The reason for the mistake was because when I (writer responsible for it here, hi) was writing this, I had the information for both fruits in front of me, but the information for grapes was on the right in my field of vision, so I errantly put it on the right on the page, too, while also accidentally crediting strawberries’ minerals to grapes, since strawberries’ data was on the left in my field a vision.
The reason for explaining this: it’s a quirky, very human way to err, in an era when a lot of web content is AI-generated with very different kinds of mistakes (usually because AI is very bad at checking sources, so will confidently state something as true despite the fact that the source was The Onion, or Clickhole, or someone’s facetiously joking answer on Quora, for example).
All in all, while we try to not make typos, we’d rather such human errors than doing like an AI and confidently telling you that Amanita phalloides mushrooms are a rich source of magnesium, and also delicious (they are, reportedly, but they are also the most deadly mushroom on the face of the Earth, also known as the Death Cap mushroom).
In any case, here’s the corrected version of the grapes vs strawberries showdown:
Grapes vs Strawberries – Which is Healthier?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: