Neurotransmitter Cheatsheet
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Which Neurotransmitter?
There are a lot of neurotransmitters that are important for good mental health (and, by way of knock-on effects, physical health).
However, when pop-science headlines refer to them as “feel-good chemicals” (yes but which one?!) or “the love molecule” (yes but which one?!) or other such vague names when referring to a specific neurotransmitter, it’s easy to get them mixed up.
So today we’re going to do a little disambiguation of some of the main mood-related neurotransmitters (there are many more, but we only have so much room), and what things we can do to help manage them.
Dopamine
This one predominantly regulates reward responses, though it’s also necessary for critical path analysis (e.g. planning), language faculties, and motor functions. It makes us feel happy, motivated, and awake.
To have more:
- eat foods that are rich in dopamine or its precursors such as tyrosine (bananas and almonds are great)
- do things that you find rewarding
Downsides: is instrumental in most addictions, and also too much can result in psychosis. For most people, that level of “too much” isn’t obtainable due to the homeostatic system, however.
See also: Rebalancing Dopamine (Without “Dopamine Fasting”)
Serotonin
This one predominantly helps regulate our circadian rhythm. It also makes us feel happy, calm, and awake.
To have more:
- get more sunlight, or if the light must be artificial, then (ideally) full-spectrum light, or (if it’s what’s available) blue light
- spend time in nature; we are hardwired to feel happy in the environments in which we evolved, which for most of human history was large open grassy expanses with occasional trees (however, for modern purposes, a park or appropriate garden will suffice).
Downsides: this is what keeps us awake at night if we had too much light before bed, and also too much serotonin can result in (potentially fatal) serotonin syndrome. Most people can’t get that much serotonin due to our homeostatic system, but some drugs can force it upon us.
See also: Seasonal Affective Disorder Strategies
Oxytocin
This one predominantly helps us connect to others on an emotional level. It also makes us feel happy, calm, and relaxed.
To have more:
- hug a loved one (or even just think about doing so, if they’re not available)
- look at pictures/videos of cute puppies, kittens, and the like—this triggers a similar response
Downsides: negligible. Socially speaking, it can cause us to drop our guard, most for most people most of the time, this is not a problem. It can also reduce sexual desire—it’s in large part responsible for the peaceful lulled state post-orgasm. It’s not responsible for the sleepiness in men though; that’s mostly prolactin.
See also: Only One Kind Of Relationship Promotes Longevity This Much!
Adrenaline
This one predominantly affects our sympathetic nervous system; it elevates heart rate, blood pressure, and other similar functions. It makes us feel alert, ready for action, and energized.
To have more:
- listen to a “power anthem” piece of music. What it is can depend on your musical tastes; whatever gets you riled up in an empowering way.
- engage in something competitive that you feel strongly about while doing it—or by the same mechanism, a solitary activity where the stakes feel high even if it’s actually quite safe (e.g. watching a thriller or a horror movie, if that’s your thing).
Downsides: its effects are not sustainable, and (in cases of chronic stress) the body will try to sustain them anyway, which has a deleterious effect. Because adrenaline and cortisol are closely linked, chronically high adrenal action will tend to mean chronically high cortisol also.
See also: Lower Your Cortisol! (Here’s Why & How)
PS: it is also called epinephrine, and chemically different but almost identical in most ways, noradrenaline or norepinephrine
Some final words
You’ll notice that in none of the “how to have more” did we mention drugs. That’s because:
- a drug-free approach is generally the best thing to try first, at the very least
- there are simply a lot of drugs to affect each one (or more), and talking about them would require talking about each drug in some detail.
However, the following may be of interest for some readers:
Antidepressants: Personalization Is Key!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Gut Diversity vs Aging
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
…and other items from this week’s health news:
How A Diverse Gut Microbiome Can Make You Younger
It’s well-known (to regular 10almonds readers, at the very least) that gut microbiome diversity is broadly a very good thing for health. What’s good for the gut is good for the heart, and what’s good for the heart is good for the brain, and also the gut is in many ways a hugely influential factor in our immune system, which includes not just when it comes to fighting pathogens, but also when it comes to healthy immune regulation, i.e. against immune dysfunction and chronic inflammation, which latter is bad for pretty much everything.
However, a new study has found a link between gut health and aging; specifically, that the aging microbiome produces fewer metabolites that are needed for good health, resulting in a compounding effect of aging.
Most interestingly, however, this relation has found to be causal the other way around, that is to say, it’s not just “when older, the gut doesn’t work so well”, but rather, “when given a better gut microbiome, effects of aging are reversed”.
Caveat: this was a mouse study and it wasn’t all aspects of aging, but it was enough aspects of aging to be very worthy of note, and there’s no reason the same principles shouldn’t apply in humans:
Read in full: Metabolic modeling reveals aging microbiome produces fewer vital substances
Related: Stop Sabotaging Your Gut
Maybe you can drink some calories, after all (if you do this with them)
“Don’t drink your calories” is generally good advice; liquids are typically absorbed much more quickly than solids (increasing total caloric consumption, as well as the initial shock to the metabolism), and most sugary drinks (which absolutely includes pure fruit juice, by the way, as it has been stripped of fiber in the juicing process) produce an impressive spike in blood sugars, and thus insulin levels (both are bad things to spike).
However, smoothies do better than juices, due to still having fiber in them. And, research has found, smoothies with seeds in flatten the blood sugar curve even more, likely due to the combination of fiber and fats:
Read in full: Smoothies with seeds may improve glycemic control, study shows
Related: 3 Day Juice Fasting? Not So Fast! ← why you should absolutely not expect the same results from juices
Where there’s smoke, there’s… An increase in mental health conditions?
Wildfires have been raging in some parts of the US lately, and needless to say, these aren’t great for the health. As well as the initial most obvious risks, there are a lot of follow-up risks (including weakened immune systems as well as increased presence of pathogens in the air; people think of smoke as purifying, but it’s not, it’s mostly just hot air bringing germs with it), and, by the numbers, a large increase in hospital visits for mental health conditions including depression, anxiety, and mood disorders:
Read in full: Exposure to wildfire smoke linked to worsening mental health conditions
Related: The Dangers Of Fires, Floods, & Having Your Hair Washed
Take care!
Share This Post
-
Fix Tight Hamstrings In Just 3 Steps
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There’s a better way to increase your flexibility than just stretching and stretching and hoping for the best. Here’s a 3-step method that will transform your flexibility:
As easy as 1-2-3
Only one part actually involves stretching:
Step 1: reciprocal inhibition
- Concept: when one muscle contracts, the opposing muscle relaxes—which is what we need.
- Goal: engage hip flexors to encourage hamstring relaxation.
- Method:
- Kneeling hamstring stretch position with one leg forward.
- Support with yoga blocks or a chair; use a cushion for comfort.
- Maintain a slight arch in the lower back and hinge forward slightly.
- Attempt to lift the foot off the floor, even if it doesn’t move.
- Hold for around 10 seconds.
Step 2: engaging more muscle fibers
- Concept: our muscles contain a lot of fibers, and often not all of them come along for the ride when we do something (exercising, stretching, etc), and those fibers that weren’t engaged will hold back the whole process.
- Goal: activate more fibers in the hamstring for a deeper stretch.
- Method:
- Same kneeling position, slight back arch, and forward hinge.
- Drive the heel into the floor as if trying to dent it.
- Apply significant effort but hold for only 10 seconds.
- A small bend in the knee is acceptable.
Step 3: manipulating the nervous system
- Concept: the nervous system often limits flexibility due to safety signals (causing sensations of discomfort to tell us to stop a lot sooner than we really need to).
- Goal: passive stretching to reduce nervous system resistance.
- Method:
- Avoid muscle engagement or movement—stay completely relaxed.
- Focus on calmness, with slow, steady breaths.
- Avoid signs of tension (e.g. clenched fists, short/sharp breathing). While your nervous system is trying to communicate to you that you are in danger, you need to communicate to your nervous system that this is fine actually, so in order to reassure your nervous system you need to avoid signs that will tip it off that you’re worried too.
- Don’t overstretch; prioritize a relaxed, safe feeling.
For more on all of this, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Tight Hamstrings? Here’s A Test To Know If It’s Actually Your Sciatic Nerve
Take care!
Share This Post
-
Cottage cheese is back and all over TikTok. Two dietitians explain why social media’s obsessed
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You might remember cottage cheese from your childhood. Back then, it was considered “diet food”. You ate it out of the tub, with celery or spread it on crackers for a low-calorie snack. Then cottage cheese went out of fashion.
But cottage cheese is having a resurgence. In recent months, Google searches for “cottage cheese” have risen to the highest levels since 2004.
Social media influencers have been promoting its benefits on TikTok and Instagram with hashtags such as #cottagecheese, #cottagecheeseforlife, and #cottagecheeserecipe. Sales of cottage cheese around the world have skyrocketed.
Let’s see why cottage cheese is having such a moment.
Karolina Kaboompics/Pexels What is cottage cheese?
Cottage cheese is a fresh dairy cheese product with a mild flavour and a slightly tangy taste. It is made by curdling cow’s milk, then draining the whey, leaving behind the curds. These curds are usually small and lumpy, and the texture can vary from creamy to dry, depending on the amount of whey left in the cheese.
The term “cottage cheese” is said to have originated because the cheese was generally made in cottage-type houses from leftover milk, after making butter.
Cottage cheese is cheap, costing about A$12 per kilogram in the supermarket, similar to ricotta cheese.
It’s also surprisingly simple to make at home using freely available recipes. All you need is milk, salt and a splash of vinegar.
We’re using cottage cheese in new ways
It’s difficult to know what started the latest cottage cheese trend. But the creativity of social media means people are sharing alternative ways to use cottage cheese, changing people’s views from it being boring and lacking flavour to it being versatile and healthy.
People are spreading cottage cheese on toast and using it to make dishes such as porridge, dips, salads, bread and flatbreads. They’re using it in cakes and scones, and in desserts such as mousse and ice cream.
Is cottage cheese healthy?
Compared with other cheeses, cottage cheese is low in fat and therefore energy (kilojoules or kJ). This makes it a smart choice for people looking to cut down on their daily energy intake.
For example, 100 grams of cottage cheese contains about 556kJ. The same amount of cheddar contains 1,254kJ and parmesan 1,565kJ.
Many cheeses are rich in protein but they often contain higher amounts of kilojoules due to their fat content. But cottage cheese has substantial amounts of protein with fewer kilojoules.
This makes cottage cheese an ideal option for people aiming to maximise their protein intake without eating large amounts of kilojoules.
Some 100g of cottage cheese provides 17g protein. This is about the same found in three eggs, 60g chicken breast or 320 millilitres (about 300g) full-fat yoghurt.
People are sharing images of their cottage cheese creations on TikTok and Instagram. New Africa/Shutterstock Cottage cheese also contains high levels of vitamin B12 (important for healthy brain function), riboflavin (supports healthy skin and eyes), phosphorus (helps build strong bones and teeth) and folate (essential for cell growth).
However, cottage cheese is lower in calcium compared with other cheeses. It contains just 89 milligrams per 100g. This compares with parmesan (948mg), haloumi (620mg) and ricotta (170mg).
You’ve convinced me. How can I use cottage cheese?
Beyond its excellent nutrition profile, the resurgence of cottage cheese is enabling people to experiment in the kitchen. Its neutral flavour and varied textures – ranging from smooth to chunky – makes it suitable for a range of dishes, from sweet to savoury.
TikTok and Instagram have some great recipes. You could start with an old faithful recipe of celery and cottage cheese, and work your way towards new options such as cottage cheese ice cream.
The healthiest recipes will be those that combine cottage cheese with wholefoods such as fruits, vegetables, nuts and seeds, and lean protein sources.
For instance, you can make a cottage cheese wrap then fill it with vegetables and a lean source of protein (such as chicken or fish).
Other combinations include cottage cheese salad dressings, vegetable dips and egg salads.
Cottage cheese’s rise in popularity is well deserved. Including more cottage cheese in your diet is a smart choice for getting a high dose of protein without adding processed ingredients or too much energy. Embrace the trend and get creative in the kitchen.
Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland and Emily Burch, Accredited Practising Dietitian and Lecturer, Southern Cross University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Alzheimer’s Sex Differences May Not Be What They Appear
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Alzheimer’s Sex Differences May Not Be What They Appear
Women get Alzheimer’s at nearly twice the rate than men do, and deteriorate more rapidly after onset, too.
So… Why?
There are many potential things to look at, but four stand out for quick analysis:
- Chromosomes: women usually have XX chromosomes, to men’s usual XY. There are outliers to both groups, people with non-standard combinations of chromosomes, but not commonly enough to throw out the stats.
- Hormones: women usually have high estrogen and low testosterone, compared to men. Again there are outliers and this is a huge oversimplification that doesn’t even look at other sex hormones, but broadly speaking (which sounds vague, but is actually what is represented in epidemiological studies), it will be so.
- Anatomy: humans have some obvious sexual dimorphism (again, there are outliers, but again, not enough to throw out the stats); this seems least likely to be relevant (Alzheimer’s is probably not stored in the breasts, for examples), though average body composition (per muscle:fat ratio) could admittedly be a factor.
- Social/lifestyle: once again, #NotAllWomen etc, but broadly speaking, women and men often tend towards different social roles in some ways, and as we know, of course lifestyle can play a part in disease pathogenesis.
As a quick aside before we continue, if you’re curious about those outliers, then a wiki-walk into the fascinating world of intersex conditions, for example, could start here. But by and large, this won’t affect most people.
So… Which parts matter?
Back in 2018, Dr. Maria Teresa Ferretti et al. kicked up some rocks in this regard, looking not just at genes (as much research has focussed on) or amyloid-β (again, well-studied) but also at phenotypes and metabolic and social factors—bearing in mind that all three of those are heavily influenced by hormones. Noting, for example, that (we’ll quote directly here):
- Men and women with Alzheimer disease (AD) exhibit different cognitive and psychiatric symptoms, and women show faster cognitive decline after diagnosis of mild cognitive impairment (MCI) or AD dementia.
- Brain atrophy rates and patterns differ along the AD continuum between the sexes; in MCI, brain atrophy is faster in women than in men.
- The prevalence and effects of cerebrovascular, metabolic and socio-economic risk factors for AD are different between men and women.
See: Sex differences in Alzheimer disease—the gateway to precision medicine
So, have scientists controlled for each of those factors?
Mostly not! But they have found clues, anyway, while noting the limitations of the previous way of conducting studies. For example:
❝Women are more likely to develop Alzheimer’s disease and experience faster cognitive decline compared to their male counterparts. These sex differences should be accounted for when designing medications and conducting clinical trials❞
~ Dr. Feixiong Cheng
Read: Research finds sex differences in immune response and metabolism drive Alzheimer’s disease
Did you spot the clue?
It was “differences in immune response and metabolism”. These things are both influenced by (not outright regulated by, but strongly influenced by) sex hormones.
❝As [hormonal] sex influences both the immune system and metabolic process, our study aimed to identify how all of these individual factors influence one another to contribute to Alzheimer’s disease❞
~ Dr. Justin Lathia
Ignoring for a moment progesterone’s role in metabolism, estrogen is an immunostimulant and testosterone is an immunosuppressant. These thus both also have an effect in inflammation, which yes, includes neuroinflammation.
But wait a minute, shouldn’t that mean that women are more protected, not less?
It should! Except… Alzheimer’s is an age-related disease, and in the age-bracket that generally gets Alzheimer’s (again, there are outliers), menopause has been done and dusted for quite a while.
Which means, and this is critical: post-menopausal women not on HRT are essentially left without the immune boost usually directed by estrogen, while men of the same age will be ticking over with their physiology that (unlike that of the aforementioned women) was already adapted to function with negligible estrogen.
Specifically:
❝The metabolic consequences of estrogen decline during menopause accelerate neuropathology in women❞
~ Dr. Rasha Saleh
Critical idea to take away from all this:
Alzheimer’s research is going to be misleading if it doesn’t take into account sex differences, and not just that, but also specifically age-relevant sex differences—because that can flip the narrative. If we don’t take age into account, we could be left thinking estrogen is to blame, when in fact, it appears to be the opposite.
In the meantime, if you’re a woman of a certain age, you might talk with a doctor about whether HRT could be beneficial for you, if you haven’t already:
❝Women at genetic risk for AD (carrying at least one APOE e4 allele) seem to be particularly benefiting from MHT❞
(MHT = Menopausal Hormone Therapy; also commonly called HRT, which is the umbrella term for Hormone Replacement Therapies in general)
~ Dr. Herman Depypere
Source study: Menopause hormone therapy significantly alters pathophysiological biomarkers of Alzheimer’s disease
Pop-sci press release version: HRT could ward off Alzheimer’s among at-risk women
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
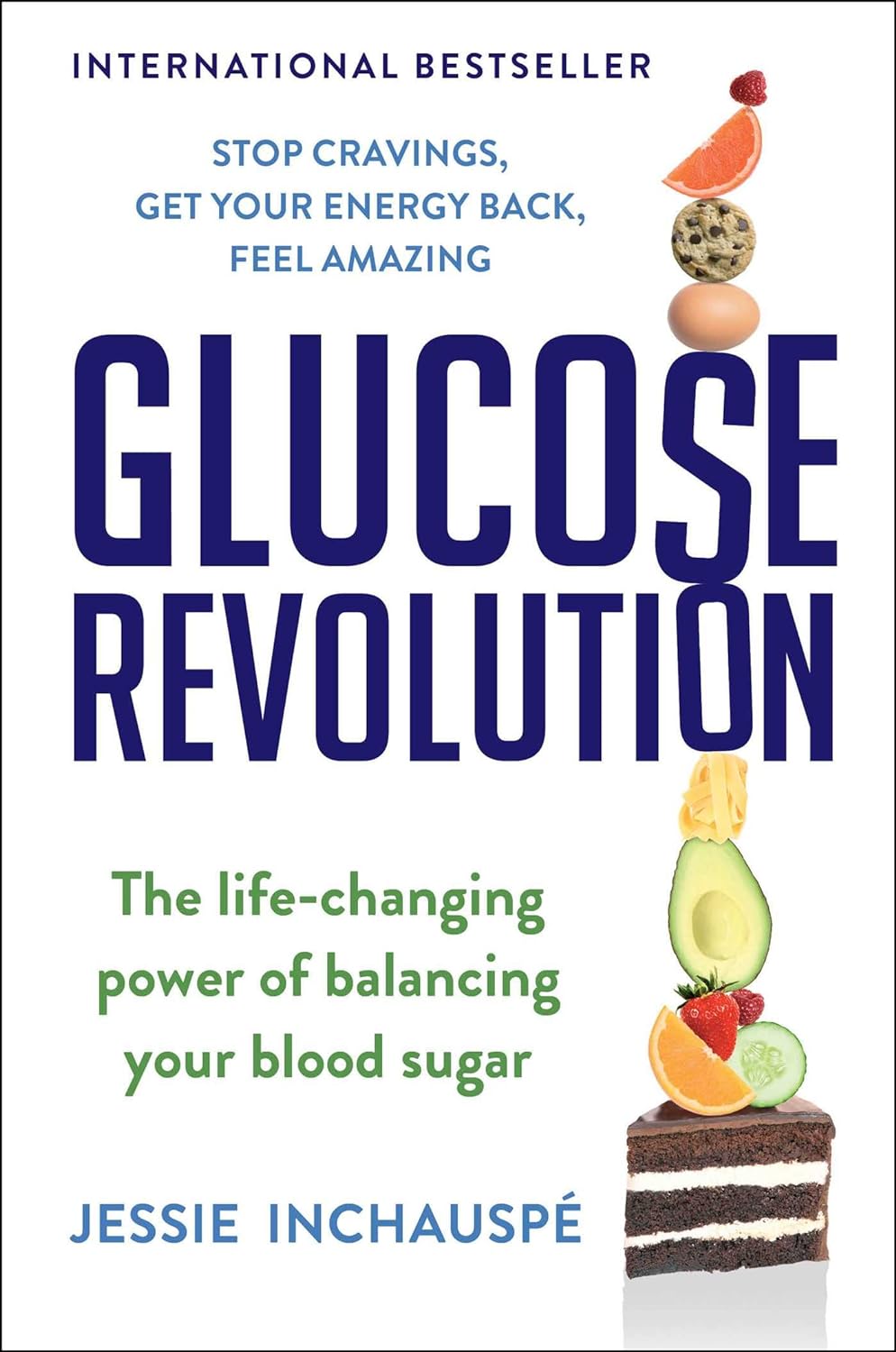
Glucose Revolution – by Jessie Inchauspé
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
While we all know that keeping balanced blood sugars is important for all us (be we diabetic, pre-diabetic, or not at all), it can be a mystifying topic!
Beyond a generic “sugar is bad”…
- What does it all mean and how does it all work?
- Should we go low-carb?
- What’s the deal with fruit?
- Carbs or protein for breakfast?
- Is “quick energy” ever a good thing?
- How do starches weigh in again?
It’s all so confusing!
Happily, Jessie Inchauspé has the incredible trifecta of qualifications to help us: she’s a biochemist, a keen cook, and a great educator. What we mean by this latter is:
Instead of dry textbook explanations, or “trust me” hand-waives, she explains biochemistry in a clear, simple, digestible (if you’ll pardon the pun) way with very helpful diagrams what things cause (or flatten) blood sugar spikes and how and why. If you read this book, you will understand, without guesswork or gaps, exactly what is happening on a physical level, and why and how her “10 hacks” work.
Her “10 hacks” are explained so thoroughly that each gets a chapter of its own, but we’ll not keep them a mystery from you meanwhile, they are:
- Eat foods in the right order
- Add a green starter to your meals
- Stop counting calories
- Flatten your breakfast curve
- Have any type of sugar you like—they’re all the same
- Pick dessert over a sweet snack
- Reach for the vinegar before you eat
- After you eat, move
- If you have to snack, go savoury
- Put some clothes on your carbs
She then finishes up with a collection of handy cheat-sheets and some of her own recipes.
Bottom line: this isn’t just a “how-to” book. It gives the how-to, yes, but it also gives such good explanations that you’ll never be confused again by what’s going on in your glucose-related health.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Other Significant Others – by Rhaina Cohen
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As we get older, it’s a function of statistics that increasingly many of us are divorced or widowed. While some will—after whatever time seems right to them—get back into dating, what about those of us who decide that we won’t?
Rhaina Cohen explores the importance of friendship, mutual support, and (Platonic!) closeness and yes, even kinds of intimacy (for that too can be Platonic!) as we go on.
Even from a purely evolutionary approach, we are fundamentally social creatures, and while as individuals we may exist on a spectrum from reclusive to extroverted, we all thrive better when we at least have access to community and friends.
The style of the book is easy-reading and exploratory, and is very compelling as a call-to-arms for those who may wish to give/receive support to/from those with whom we are not necessarily sleeping.
Because at the end of the day, why should sex and/or romance be a required feature for legal protections? Aren’t we adults who can make our own decisions about whom we trust to care for us?
Bottom line: if you’re happily partnered and expect to pre-decease your partner, this book might not be directly important for you (it might for your partner, though). Everyone else? This book may be important at some point. That point might even be now already; only you know.
Click here to check out The Other Significant Others, and make your own choices in life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: