Mythbusting Moldy Food
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most Food Should Not Be Fuzzy
In yesterday’s newsletter, we asked you for your policy when it comes to mold on food (aside from intentional mold, e.g. blue cheese etc), and the responses were interesting:
- About 49% said “throw the whole thing away no matter what it is; it is dangerous”
- About 24% said “cut the mold off and eat the rest of whatever it is”
- The remainder were divided equally between “eat it all; keep the immune system on its toes” and “cut the mold off bread, but moldy animal products are dangerous”
So what does the science say?
Some molds are safe to eat: True or False?
True! We don’t think this is contentious so we’ll not spend much time on it, but just for the sake of being methodical: foods that are supposed to have mold on, including many kinds of cheese and even some kinds of cured meat (salami is an example; that powdery coating is mold).
We could give a big list of safe and unsafe molds, but that would be a list of names and let’s face it, they don’t introduce themselves by name.
However! The litmus test of “is it safe to eat” is:
Did you acquire it with this mold already in place and exactly as expected and advertised?
- If so, it is safe to eat (unless you have an allergy or such)
- If not, it is almost certainly not safe to eat
(more on why, later)
The “sniff test” is a good way to tell if moldy food is bad: True or False?
False. Very false. Because of how the sense of smell works.
You may feel like smell is a way of knowing about something at a distance, but the only way you can smell something is if particles of it are physically connecting with your olfactory receptors inside you. Yes, that has unfortunate implications about bathroom smells, but for now, let’s keep our attention in the kitchen.
If you sniff a moldy item of food, you will now have its mold spores inside your respiratory system. You absolutely do not want them there.
If we cut off the mold, the rest is safe to eat: True or False?
True or False, depending on what it is:
- Hard vegetables (e.g carrots, cabbage), and hard cheeses (e.g. Gruyère, Gouda) – cut off with an inch margin, and it should be safe
- Soft vegetables (e.g. tomatoes, and any vegetables that were hard but are now soft after cooking) – discard entirely; it is unsafe
- Anything else – discard entirely; it is unsafe
The reason for this is because in the case of the hard products mentioned, the mycelium roots of the mold cannot penetrate far.
In the case of the soft products mentioned, the surface mold is “the tip of the iceberg”, and the mycelium roots, which you will not usually be able to see, will penetrate the rest of it.
“Anything else” seems like quite a sweeping statement, but fruits, soft cheeses, yogurt, liquids, jams and jellies, cooked grains and pasta, meats, and yes, bread, are all things where the roots can penetrate deeply and easily. Regardless of you only being able to see a small amount, the whole thing is probably moldy.
The USDA has a handy downloadable factsheet:
Molds On Food: Are They Dangerous?
Eating a little mold is good for the immune system: True or False?
False, generally. There are of course countless types of mold, but not only are many of them pathogenic (mycotoxins), but also, a food that has mold will usually also have pathogenic bacteria along with the mold.
See for example: Occurrence, Toxicity, and Analysis of Major Mycotoxins in Food
Food poisoning will never make you healthier.
But penicillin is safe to eat: True or False?
False, and also penicillin is not the mold on your bread (or other foods).
Penicillin, an antibiotic* molecule, is produced by some species of Penicillium sp., a mold. There are hundreds of known species of Penicillium sp., and most of them are toxic, usually in multiple ways. Take for example:
Penicillium roqueforti PR toxin gene cluster characterization
*it is also not healthy to consume antibiotics unless it is seriously necessary. Antibiotics will wipe out most of your gut’s “good bacteria”, leaving you vulnerable. People have died from C. diff infections for this reason. So obviously, if you really need to take antibiotics, take them as directed, but if not, don’t.
See also: Four Ways Antibiotics Can Kill You
One last thing…
It may be that someone reading this is thinking “I’ve eaten plenty of mold, and I’m fine”. Or perhaps someone you tell about this will say that.
But there are two reasons this logic is flawed:
- Survivorship bias (like people who smoke and live to 102; we just didn’t hear from the 99.9% of people who smoke and die early)
- Being unaware of illness is not being absent of illness. Anyone who’s had an alarming diagnosis of something that started a while ago will know this, of course. It’s also possible to be “low-level ill” often and get used to it as a baseline for health. It doesn’t mean it’s not harmful for you.
Stay safe!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Alpha, beta, theta: what are brain states and brain waves? And can we control them?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There’s no shortage of apps and technology that claim to shift the brain into a “theta” state – said to help with relaxation, inward focus and sleep.
But what exactly does it mean to change one’s “mental state”? And is that even possible? For now, the evidence remains murky. But our understanding of the brain is growing exponentially as our methods of investigation improve.
Brain-measuring tech is evolving
Currently, no single approach to imaging or measuring brain activity gives us the whole picture. What we “see” in the brain depends on which tool we use to “look”. There are myriad ways to do this, but each one comes with trade-offs.
We learnt a lot about brain activity in the 1980s thanks to the advent of magnetic resonance imaging (MRI).
Eventually we invented “functional MRI”, which allows us to link brain activity with certain functions or behaviours in real time by measuring the brain’s use of oxygenated blood during a task.
We can also measure electrical activity using EEG (electroencephalography). This can accurately measure the timing of brain waves as they occur, but isn’t very accurate at identifying which specific areas of the brain they occur in.
Alternatively, we can measure the brain’s response to magnetic stimulation. This is very accurate in terms of area and timing, but only as long as it’s close to the surface.
What are brain states?
All of our simple and complex behaviours, as well as our cognition (thoughts) have a foundation in brain activity, or “neural activity”. Neurons – the brain’s nerve cells – communicate by a sequence of electrical impulses and chemical signals called “neurotransmitters”.
Neurons are very greedy for fuel from the blood and require a lot of support from companion cells. Hence, a lot of measurement of the site, amount and timing of brain activity is done via measuring electrical activity, neurotransmitter levels or blood flow.
We can consider this activity at three levels. The first is a single-cell level, wherein individual neurons communicate. But measurement at this level is difficult (laboratory-based) and provides a limited picture.
As such, we rely more on measurements done on a network level, where a series of neurons or networks are activated. Or, we measure whole-of-brain activity patterns which can incorporate one or more so-called “brain states”.
According to a recent definition, brain states are “recurring activity patterns distributed across the brain that emerge from physiological or cognitive processes”. These states are functionally relevant, which means they are related to behaviour.
Brain states involve the synchronisation of different brain regions, something that’s been most readily observed in animal models, usually rodents. Only now are we starting to see some evidence in human studies.
Various kinds of states
The most commonly-studied brain states in both rodents and humans are states of “arousal” and “resting”. You can picture these as various levels of alertness.
Studies show environmental factors and activity influence our brain states. Activities or environments with high cognitive demands drive “attentional” brain states (so-called task-induced brain states) with increased connectivity. Examples of task-induced brain states include complex behaviours such as reward anticipation, mood, hunger and so on.
In contrast, a brain state such as “mind-wandering” seems to be divorced from one’s environment and tasks. Dropping into daydreaming is, by definition, without connection to the real world.
We can’t currently disentangle multiple “states” that exist in the brain at any given time and place. As mentioned earlier, this is because of the trade-offs that come with recording spatial (brain region) versus temporal (timing) brain activity.
Brain states vs brain waves
Brain state work can be couched in terms such as alpha, delta and so forth. However, this is actually referring to brain waves which specifically come from measuring brain activity using EEG.
EEG picks up on changing electrical activity in the brain, which can be sorted into different frequencies (based on wavelength). Classically, these frequencies have had specific associations:
- gamma is linked with states or tasks that require more focused concentration
- beta is linked with higher anxiety and more active states, with attention often directed externally
- alpha is linked with being very relaxed, and passive attention (such as listening quietly but not engaging)
- theta is linked with deep relaxation and inward focus
- and delta is linked with deep sleep.
Brain wave patterns are used a lot to monitor sleep stages. When we fall asleep we go from drowsy, light attention that’s easily roused (alpha), to being relaxed and no longer alert (theta), to being deeply asleep (delta).
Can we control our brain states?
The question on many people’s minds is: can we judiciously and intentionally influence our brain states?
For now, it’s likely too simplistic to suggest we can do this, as the actual mechanisms that influence brain states remain hard to detangle. Nonetheless, researchers are investigating everything from the use of drugs, to environmental cues, to practising mindfulness, meditation and sensory manipulation.
Controversially, brain wave patterns are used in something called “neurofeedback” therapy. In these treatments, people are given feedback (such as visual or auditory) based on their brain wave activity and are then tasked with trying to maintain or change it. To stay in a required state they may be encouraged to control their thoughts, relax, or breathe in certain ways.
The applications of this work are predominantly around mental health, including for individuals who have experienced trauma, or who have difficulty self-regulating – which may manifest as poor attention or emotional turbulence.
However, although these techniques have intuitive appeal, they don’t account for the issue of multiple brain states being present at any given time. Overall, clinical studies have been largely inconclusive, and proponents of neurofeedback therapy remain frustrated by a lack of orthodox support.
Other forms of neurofeedback are delivered by MRI-generated data. Participants engaging in mental tasks are given signals based on their neural activity, which they use to try and “up-regulate” (activate) regions of the brain involved in positive emotions. This could, for instance, be useful for helping people with depression.
Another potential method claimed to purportedly change brain states involves different sensory inputs. Binaural beats are perhaps the most popular example, wherein two different wavelengths of sound are played in each ear. But the evidence for such techniques is similarly mixed.
Treatments such as neurofeedback therapy are often very costly, and their success likely relies as much on the therapeutic relationship than the actual therapy.
On the bright side, there’s no evidence these treatment do any harm – other than potentially delaying treatments which have been proven to be beneficial.
Susan Hillier, Professor: Neuroscience and Rehabilitation, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
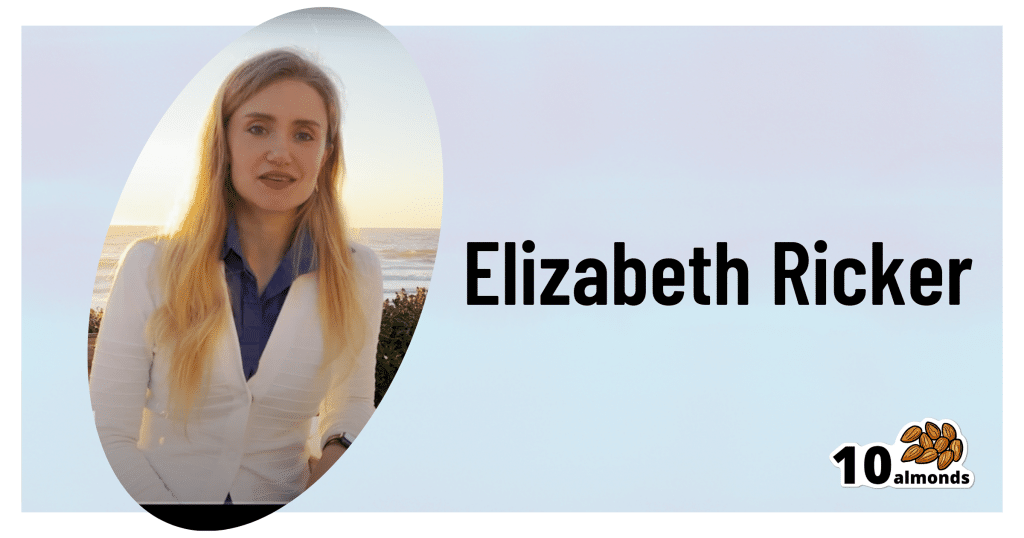
Cognitive Enhancement Without Drugs
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cognitive Enhancement Without Drugs
This is Elizabeth Ricker. She’s a Harvard-and-MIT-trained neuroscientist and researcher, who now runs the “Citizen Science” DIY-neurohacking organization, NeuroEducate.
Sounds fun! What’s it about?
The philosophy that spurs on her research and practice can be summed up as follows:
❝I’m not going to leave my brain up to my doctor or [anyone else]… My brain is my own responsibility, and I’m going to do the best that I can to optimize it❞
Her goal is not just to optimize her own brain though; she wants to make the science accessible to everyone.
What’s this about Citizen Science?
“Citizen Science” is the idea that while there’s definitely an important role in society for career academics, science itself should be accessible to all. And, not just the conclusions, but the process too.
This can take the form of huge experiments, often facilitated these days by apps where we opt-in to allow our health metrics (for example) to be collated with many thousands of others, for science. It can also involve such things as we talked about recently, getting our own raw genetic data and “running the numbers” at home to get far more comprehensive and direct information than the genetic testing company would ever provide us.
For Ricker, her focus is on the neuroscience side of biohacking, thus, neurohacking.
I’m ready to hack my brain! Do I need a drill?
Happily not! Although… Bone drills for the skull are very convenient instruments that make it quite hard to go wrong even with minimal training. The drill bit has a little step/ledge partway down, which means you can only drill through the thickness of the skull itself, before the bone meeting the wider part of the bit stops you from accidentally drilling into the brain. Still, please don’t do this at home.
What you can do at home is a different kind of self-experimentation…
If you want to consider which things are genuinely resulting in cognitive enhancement and which things are not, you need to approach the matter like a scientist. That means going about it in an organized fashion, and recording results.
There are several ways cognitive enhancement can be measured, including:
- Learning and memory
- Executive function
- Emotional regulation
- Creative intelligence
Let’s look at each of them, and what can be done. We don’t have a lot of room here; we’re a newsletter not a book, but we’ll cover one of Ricker’s approaches for each:
Learning and memory
This one’s easy. We’re going to leverage neuroplasticity (neurons that fire together, wire together!) by simple practice, and introduce an extra element to go alongside your recall. Perhaps a scent, or a certain item of clothing. Tell yourself that clinical studies have shown that this will boost your recall. It’s true, but that’s not what’s important; what’s important is that you believe it, and bring the placebo effect to bear on your endeavors.
You can test your memory with word lists, generated randomly by AI, such as this one:
You’ll soon find your memory improving—but don’t take our word for it!
Executive function
Executive function is the aspect of your brain that tells the other parts how to work, when to work, and when to stop working. If you’ve ever spent 30 minutes thinking “I need to get up” but you were stuck in scrolling social media, that was executive dysfunction.
This can be trained using the Stroop Color and Word Test, which shows you words, specifically the names of colors, which will themselves be colored, but not necessarily in the color the word pertains to. So for example, you might be shown the word “red”, colored green. Your task is to declare either the color of the word only, ignoring the word itself, or the meaning of the word only, ignoring its appearance. It can be quite challenging, but you’ll get better quite quickly:
The Stroop Test: Online Version
Emotional Regulation
This is the ability to not blow up angrily at the person with whom you need to be diplomatic, or to refrain from laughing when you thought of something funny in a sombre situation.
It’s an important part of cognitive function, and success or failure can have quite far-reaching consequences in life. And, it can be trained too.
There’s no online widget for this one, but: when and if you’re in a position to safely* do so, think about something that normally triggers a strong unwanted emotional reaction. It doesn’t have to be something life-shattering, but just something that you feel in some way bad about. Hold this in your mind, sit with it, and practice mindfulness. The idea is to be able to hold the unpleasant idea in your mind, without becoming reactive to it, or escaping to more pleasant distractions. Build this up.
*if you perchance have PTSD, C-PTSD, or an emotional regulation disorder, you might want to talk this one through with a qualified professional first.
Creative Intelligence
Another important cognitive skill, and again, one that can be cultivated and grown.
The trick here is volume. A good, repeatable test is to think of a common object (e.g. a rock, a towel, a banana) and, within a time constraint (such as 15 minutes) list how many uses you can think of for that item.
Writer’s storytime: once upon a time, I was sorting through an inventory of medical equipment with a colleague, and suggested throwing out our old arterial clamps, as we had newer, better ones—in abundance. My colleague didn’t want to part with them, so I challenged him “Give me one use for these, something we could in some possible world use them for that the new clamps don’t do better, and we’ll keep them”. He said “Thumbscrews”, and I threw my hands up in defeat, saying “Fine!”, as he had technically fulfilled my condition.
What’s the hack to improve this one? Just more volume. Creativity, as it turns out, isn’t something we can expend—like a muscle, it grows the more we use it. And because the above test is repeatable (with different objects), you can track your progress.
And if you feel like using your grown creative muscle to write/paint/compose/etc your magnum opus, great! Or if you just want to apply it to the problem-solving of everyday life, also great!
In summary…
Our brain is a wonderful organ with many functions. Society expects us to lose these as we get older, but the simple, scientific truth is that we can not only maintain our cognitive function, but also enhance and grow it as we go.
Want to know more from today’s featured expert?
You might enjoy her book, “Smarter Tomorrow”, which we reviewed back in March
Share This Post
-
Herbs For Evidence-Based Health & Healing
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Herbs have been used since prehistoric times to treat injuries and illnesses, but which ones actually work, as opposed to being “old wives’ tales”?
Even today, in pharmacies herbals products may come with a disclaimer “based on traditional use only”, which, in scientific terms, means it likely performs no better than placebo.
This is a “Saturday Life Hacks” edition, not a “Research Review Monday”, so we won’t be doing any deep-dives today, and will instead keep things short and snappy. We’ll also spotlight one main benefit, rather than trying to cover all bases, as we often have room to do on a Monday!
Basil
Helps boost immunity:
Chamomile
Significantly reduces symptoms of osteoarthritis:
(This one challenged your writer’s resolve as it does so many things, it was hard to pick just one. So, she went with one that’s less known that “settling the stomach” and “relieving PMS” and “relaxation” and so forth)
Echinacea
Significantly reduces the risk of catching a cold (but won’t help once you’ve caught it):
Echinacea for preventing and treating the common cold
Elderberry
Significantly hastens recovery from upper respiratory viral infections:
Evening Primrose
Fights neuropathy, along with many other benefits:
An updated review on pharmacological activities and phytochemical constituents of evening primrose
Fennel
Antinflammatory, along with many other benefits:
Ginkgo biloba
Antioxidant effects provide anti-aging benefits:
Advances in the Studies of Ginkgo Biloba Leaves Extract on Aging-Related Diseases
Ginseng
Combats fatigue:
Ginseng as a Treatment for Fatigue: A Systematic Review
Lavender
Enjoyed for its sedative effects, which is really does have:
Evidence for Sedative Effects of the Essential Oil of Lavender after Inhalation
Sage
Helps fight HIV type 1 and Herpes simplex type 2 (and probably other viruses, but that’s what we have the science for right now):
Aqueous extracts from peppermint, sage and lemon balm leaves display potent anti-HIV-1 activity
Valerian
Inconclusive data; “traditional use only” for restful sleep.
Can’t have everything!
Share This Post
Related Posts
-
Doctors Are as Vulnerable to Addiction as Anyone. California Grapples With a Response
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
BEVERLY HILLS, Calif. — Ariella Morrow, an internal medicine doctor, gradually slid from healthy self-esteem and professional success into the depths of depression.
Beginning in 2015, she suffered a string of personal troubles, including a shattering family trauma, marital strife, and a major professional setback. At first, sheer grit and determination kept her going, but eventually she was unable to keep her troubles at bay and took refuge in heavy drinking. By late 2020, Morrow could barely get out of bed and didn’t shower or brush her teeth for weeks on end. She was up to two bottles of wine a day, alternating it with Scotch whisky.
Sitting in her well-appointed home on a recent autumn afternoon, adorned in a bright lavender dress, matching lipstick, and a large pearl necklace, Morrow traced the arc of her surrender to alcohol: “I’m not going to drink before 5 p.m. I’m not going to drink before 2. I’m not going to drink while the kids are home. And then, it was 10 o’clock, 9 o’clock, wake up and drink.”
As addiction and overdose deaths command headlines across the nation, the Medical Board of California, which licenses MDs, is developing a new program to treat and monitor doctors with alcohol and drug problems. But a fault line has appeared over whether those who join the new program without being ordered to by the board should be subject to public disclosure.
Patient advocates note that the medical board’s primary mission is “to protect healthcare consumers and prevent harm,” which they say trumps physician privacy.
The names of those required by the board to undergo treatment and monitoring under a disciplinary order are already made public. But addiction medicine professionals say that if the state wants troubled doctors to come forward without a board order, confidentiality is crucial.
Public disclosure would be “a powerful disincentive for anybody to get help” and would impede early intervention, which is key to avoiding impairment on the job that could harm patients, said Scott Hambleton, president of the Federation of State Physician Health Programs, whose core members help arrange care and monitoring of doctors for substance use disorders and mental health conditions as an alternative to discipline.
But consumer advocates argue that patients have a right to know if their doctor has an addiction. “Doctors are supposed to talk to their patients about all the risks and benefits of any treatment or procedure, yet the risk of an addicted doctor is expected to remain a secret?” Marian Hollingsworth, a volunteer advocate with the Patient Safety Action Network, told the medical board at a Nov. 14 hearing on the new program.
Doctors are as vulnerable to addiction as anyone else. People who work to help rehabilitate physicians say the rate of substance use disorders among them is at least as high as the rate for the general public, which the federal Substance Abuse and Mental Health Services Administration put at 17.3% in a Nov. 13 report.
Alcohol is a very common drug of choice among doctors, but their ready access to pain meds is also a particular risk.
“If you have an opioid use disorder and are working in an operating room with medications like fentanyl staring you down, it’s a challenge and can be a trigger,” said Chwen-Yuen Angie Chen, an addiction medicine doctor who chairs the Well-Being of Physicians and Physicians-in-Training Committee at Stanford Health Care. “It’s like someone with an alcohol use disorder working at a bar.”
From Pioneer to Lagger
California was once at the forefront of physician treatment and monitoring. In 1981, the medical board launched a program for the evaluation, treatment, and monitoring of physicians with mental illness or substance use problems. Participants were often required to take random drug tests, attend multiple group meetings a week, submit to work-site surveillance by colleagues, and stay in the program for at least five years. Doctors who voluntarily entered the program generally enjoyed confidentiality, but those ordered into it by the board as part of a disciplinary action were on the public record.
The program was terminated in 2008 after several audits found serious flaws. One such audit, conducted by Julianne D’Angelo Fellmeth, a consumer interest lawyer who was chosen as an outside monitor for the board, found that doctors in the program were often able to evade the random drug tests, attendance at mandatory group therapy sessions was not accurately tracked, and participants were not properly monitored at work sites.
Today, MDs who want help with addiction can seek private treatment on their own or in many cases are referred by hospitals and other health care employers to third parties that organize treatment and surveillance. The medical board can order a doctor on probation to get treatment.
In contrast, the California licensing boards of eight other health-related professions, including osteopathic physicians, registered nurses, dentists, and pharmacists, have treatment and monitoring programs administered under one master contract by a publicly traded company called Maximus Inc. California paid Maximus about $1.6 million last fiscal year to administer those programs.
When and if the final medical board regulations are adopted, the next step would be for the board to open bidding to find a program administrator.
Fall From Grace
Morrow’s troubles started long after the original California program had been shut down.
The daughter of a prominent cosmetic surgeon, Morrow grew up in Palm Springs in circumstances she describes as “beyond privileged.” Her father, David Morrow, later became her most trusted mentor.
But her charmed life began to fall apart in 2015, when her father and mother, Linda Morrow, were indicted on federal insurance fraud charges in a well-publicized case. In 2017, the couple fled to Israel in an attempt to escape criminal prosecution, but later they were both arrested and returned to the United States to face prison sentences.
The legal woes of Morrow’s parents, later compounded by marital problems related to the failure of her husband’s business, took a heavy toll on Morrow. She was in her early 30s when the trouble with her parents started, and she was working 16-hour days to build a private medical practice, with two small children at home. By the end of 2019, she was severely depressed and turning increasingly to alcohol. Then, the loss of her admitting privileges at a large Los Angeles hospital due to inadequate medical record-keeping shattered what remained of her self-confidence.
Morrow, reflecting on her experience, said the very strengths that propel doctors through medical school and keep them going in their careers can foster a sense of denial. “We are so strong that our strength is our greatest threat. Our power is our powerlessness,” she said. Morrow ignored all the flashing yellow lights and even the red light beyond which serious trouble lay: “I blew through all of it, and I fell off the cliff.”
By late 2020, no longer working, bedridden by depression, and drinking to excess, she realized she could no longer will her way through: “I finally said to my husband, ‘I need help.’ He said, ‘I know you do.’”
Ultimately, she packed herself off to a private residential treatment center in Texas. Now sober for 21 months, Morrow said the privacy of the addiction treatment she chose was invaluable because it shielded her from professional scrutiny.
“I didn’t have to feel naked and judged,” she said.
Morrow said her privacy concerns would make her reluctant to join a state program like the one being considered by the medical board.
Physician Privacy vs. Patient Protection
The proposed regulations would spare doctors in the program who were not under board discipline from public disclosure as long as they stayed sober and complied with all the requirements, generally including random drug tests, attendance at group sessions, and work-site monitoring. If the program put a restriction on a doctor’s medical license, it would be posted on the medical board’s website, but without mentioning the doctor’s participation in the program.
Yet even that might compromise a doctor’s career since “having a restricted license for unspecified reasons could have many enduring personal and professional implications, none positive,” said Tracy Zemansky, a clinical psychologist and president of the Southern California division of Pacific Assistance Group, which provides support and monitoring for physicians.
Zemansky and others say doctors, just like anyone else, are entitled to medical privacy under federal law, as long as they haven’t caused harm.
Many who work in addiction medicine also criticized the proposed new program for not including mental health problems, which often go hand in hand with addiction and are covered by physician health programs in other states.
“To forgo mental health treatment, I think, is a grave mistake,” Morrow said. For her, depression and alcoholism were inseparable, and the residential program she attended treated her for both.
Another point of contention is money. Under the current proposal, doctors would bear all the costs of the program.
The initial clinical evaluation, plus the regular random drug tests, group sessions, and monitoring at their work sites could cost participants over $27,000 a year on average, according to estimates posted by the medical board. And if they were required to go for 30-day inpatient treatment, that would add an additional $40,000 — plus nearly $36,000 in lost wages.
People who work in the field of addiction medicine believe that is an unfair burden. They note that most programs for physicians in other states have outside funding to reduce the cost to participants.
“The cost should not be fully borne by the doctors, because there are many other people that are benefiting from this, including the board, malpractice insurers, hospitals, the medical association,” said Greg Skipper, a semi-retired addiction medicine doctor who ran Alabama’s state physician health program for 12 years. In Alabama, he said, those institutions contribute to the program, significantly cutting the amount doctors have to pay.
The treatment program that Morrow attended in spring of 2021, at The Menninger Clinic in Houston, cost $80,000 for a six-week stay, which was covered by a concerned family member. “It saved my life,” she said.
Though Morrow had difficulty maintaining her sobriety in the first year after treatment, she has now been sober since April 2, 2022. These days, Morrow regularly attends therapy and Alcoholics Anonymous and has pivoted to become an addiction medicine doctor.
“I am a better doctor today because of my experience — no question,” Morrow said. “I am proud to be a doctor who’s an alcoholic in recovery.”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Enjoy Bitter Foods For Your Heart & Brain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Bitter Is Better
A good general rule of thumb for “does this food contain a lot of healthy polyphenols?” is:
“is this (edible) plant bitter/astringent/pungent”?
If it is, it’s probably rich in polyphenols:
Deciphering the role of bitter and astringent polyphenols in promoting well-being
…which is why it’s no surprise that black coffee and bitter chocolate score highly, as do hot peppers and even garlic.
See also: Our Top 5 Spices: How Much Is Enough For Benefits?
Even fruits, generally considered something sweet to eat, often contain more polyphenols when they are bitter—many berries are great examples of this!
Read more: Goji Berries: Which Benefits Do They Really Have?
You can read more about the science of this here:
Sensory Nutrition and Bitterness and Astringency of Polyphenols
Important for multiple reasons (including heart and brain health)
Polyphenols have many benefits, and they’re most well known for their heart-healthy properties, but their antioxidant effect (and other mechanisms) also means these foods are generally neuroprotectants too:
The science of this is not all as obvious as you might think!
It is reasonable to expect “ok, this has antioxidant effect, so it will reduce oxidative damage to brain cells too”, and while that is true (and yes, polyphenols do cross the blood-brain barrier), they also help in other ways, including through the gut:
What if I don’t like bitter/astringent/pungent foods?
If you do not have a medical condition that proscribes them (do check with your doctor if unsure), the best advice is to simply eat them anyway, and your tastes will adapt.
It will also help if you avoid sweet foods (though this too is also a good general rule of thumb!), as this will move the balance of where your brain’s “set range” is for “good taste”.
Bonus tip: dark chocolate (80%+ cocoa if possible, 95% if you can get it) and chilli peppers go great with each other. Here’s an example of a chilli chocolate product on Amazon; it’s 70% cocoa (which is not bad, but could be better). You might be able to get a higher percentage locally, especially if you ask your local chocolatière, or make it yourself!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Statins: His & Hers?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Hidden Complexities of Statins and Cardiovascular Disease (CVD)
This is Dr. Barbara Roberts. She’s a cardiologist and the Director of the Women’s Cardiac Center at one of the Brown University Medical School teaching hospitals. She’s an Associate Clinical Professor of Medicine and takes care of patients, teaches medical students, and does clinical research. She specializes in gender-specific aspects of heart disease, and in heart disease prevention.
We previously reviewed Dr. Barbara Roberts’ excellent book “The Truth About Statins: Risks and Alternatives to Cholesterol-Lowering Drugs”. It prompted some requests to do a main feature about Statins, so we’re doing it today. It’s under the auspices of “Expert Insights” as we’ll be drawing almost entirely from Dr. Roberts’ work.
So, what are the risks of statins?
According to Dr. Roberts, one of the biggest risks is not just drug side-effects or anything like that, but rather, what they simply won’t treat. This is because statins will lower LDL (bad) cholesterol levels, without necessarily treating the underlying cause.
Imagine you got Covid, and it’s one of the earlier strains that’s more likely deadly than “merely” debilitating.
You’re coughing and your throat feels like you gargled glass.
Your doctor gives you a miracle cough medicine that stops your coughing and makes your throat feel much better.
(Then a few weeks later, you die, because this did absolutely nothing for the underlying problem)
You see the problem?
Are there problematic side-effects too, though?
There can be. But of course, all drugs can have side effects! So that’s not necessarily news, but what’s relevant here is the kind of track these side-effects can lead one down.
For example, Dr. Roberts cites a case in which a woman’s LDL levels were high and she was prescribed simvastatin (Zocor), 20mg/day. Here’s what happened, in sequence:
- She started getting panic attacks. So, her doctor prescribed her sertraline (Zoloft) (a very common SSRI antidepressant) and when that didn’t fix it, paroxetine (Paxil). This didn’t work either… because the problem was not actually her mental health. The panic attacks got worse…
- Then, while exercising, she started noticing progressive arm and leg weakness. Her doctor finally took her off the simvastatin, and temporarily switched to ezetimibe (Zetia), a less powerful nonstatin drug that blocks cholesterol absorption, which change eased her arm and leg problem.
- As the Zetia was a stopgap measure, the doctor put her on atorvastatin (Lipitor). Now she got episodes of severe chest pressure, and a skyrocketing heart rate. She also got tremors and lost her body temperature regulation.
- So the doctor stopped the atorvastatin and tried rosovastatin (Crestor), on which she now suffered exhaustion (we’re not surprised, by this point) and muscle pains in her arms and chest.
- So the doctor stopped the rosovastatin and tried lovastatin (Mevacor), and now she had the same symptoms as before, plus light-headedness.
- So the doctor stopped the lovastatin and tried fluvastatin (Lescol). Same thing happened.
- So he stopped the fluvastatin and tried pravastatin (Pravachol), without improvement.
- So finally he took her off all these statins because the high LDL was less deleterious to her life than all these things.
- She did her own research, and went back to the doctor to ask for cholestyramine (Questran), which is a bile acid sequestrent and nothing to do with statins. She also asked for a long-acting niacin. In high doses, niacin (one of the B-vitamins) raises HDL (good) cholesterol, lowers LDL, and lowers tryglycerides.
- Her own non-statin self-prescription (with her doctor’s signature) worked, and she went back to her life, her work, and took up running.
Quite a treatment journey! Want to know more about the option that actually worked?
Read: Bile Acid Resins or Sequestrants
What are the gender differences you/she mentioned?
Actually mostly sex differences, since this appears to be hormonal (which means that if your hormones change, so will your risk). A lot of this is still pending more research—basically it’s a similar problem in heart disease to one we’ve previously talked about with regard to diabetes. Diabetes disproportionately affects black people, while diabetes research disproportionately focuses on white people.
In this case, most heart disease research has focused on men, with women often not merely going unresearched, but also often undiagnosed and untreated until it’s too late. And the treatments, if prescribed? Assumed to be the same as for men.
Dr. Roberts tells of how medicine is taught:
❝When I was in medical school, my professors took the “bikini approach” to women’s health: women’s health meant breasts and reproductive organs. Otherwise the prototypical patient was presented as a man.❞
There has been some research done with statins and women, though! Just, still not a lot. But we do know for example that some statins can be especially useful for treating women’s atherosclerosis—with a 50% success rate, rather than 31% for men.
For lowering LDL itself, however, it can work but is generally not so hot in women.
Fun fact:
In men:
- High total cholesterol
- High non-HDL cholesterol
- High LDL cholesterol
- Low HDL cholesterol
…are all significantly associated with an increased risk of death from CVD.
In women:
…levels of LDL cholesterol even more than 190 were associated with only a small, statistically insignificant increased risk of dying from CVD.
So…
The fact that women derive less benefit from a medicine that mainly lowers LDL cholesterol, may be because elevated LDL cholesterol is less harmful to women than it is to men.
And also: Treatment and Response to Statins: Gender-related Differences
And for that matter: Women Versus Men: Is There Equal Benefit and Safety from Statins?*
Definitely a case where Betteridge’s Law of Headlines applies!
What should women do to avoid dying of CVD, then?
First, quick reminder of our general disclaimer: we can’t give medical advice and nothing here comprises such. However… One particularly relevant thing we found illuminating in Dr. Roberts’ work was this observation:
The metabolic syndrome is diagnosed if you have three (or more) out of five of the following:
- Abdominal obesity (waist >35″ if a woman or >40″ if a man)
- Fasting blood sugars of 100mg/dl or more
- Fasting triglycerides of 150mg/dl or more
- Blood pressure of 130/85 or higher
- HDL <50 if a woman or <40 if a man
And yet… because these things can be addressed with exercise and a healthy diet, which neither pharmaceutical companies nor insurance companies have a particular stake in, there’s a lot of focus instead on LDL levels (since there are a flock of statins that can be sold be lower them)… Which, Dr. Roberts says, is not nearly as critical for women.
So women end up getting prescribed statins that cause panic attacks and all those things we mentioned earlier… To lower our LDL, which isn’t nearly as big a factor as the other things.
In summary:
Statins do have their place, especially for men. They can, however, mask underlying problems that need treatment—which becomes counterproductive.
When it comes to women, statins are—in broad terms—statistically not as good. They are a little more likely to be helpful specifically in cases of atherosclerosis, whereby they have a 50/50 chance of helping.
For women in particular, it may be worthwhile looking into alternative non-statin drugs, and, for everyone: diet and exercise.
Further reading: How Can I Safely Come Off Statins?
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: