Mind Gym – by Gary Mack and David Casstevens
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
While this book seems to be mostly popular amongst young American college athletes and those around them (coaches, parents, etc) its applicability is a lot wider than that.
The thing is, as this book details, we don’t have to settle for less than optimal in our training—whatever “optimal” means for us, at any stage of life.
The style is largely narrative, and conveys a lot of ideas through anecdotes. They are probably true, but whether they occured entirely as-written or have been polished or embellished is not so important, as to to give food for thought, and reflection on how we can hone what we’re doing to work the best for us.
Nor is it just a long pep-talk, though it certainly has a motivational aspect. But rather, it covers also such things as the seven critical areas that we need to excel at if we want to be mentally robust, and—counterintuitively—the value of slowing down sometimes. The authors also talk about the importance of love, labor, and ongoing learning if we want a fulfilled life.
Bottom line: if you are engaged with any sport or sport-like endeavor that you’d like to be better at, this book will sharpen your training and development.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Plum vs Nectarine – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing plums to nectarines, we picked the nectarines.
Why?
Both are great! But nectarines win at least marginally in each category we look at.
In terms of macros, plums have more carbs while nectarines have more fiber, resulting of course in a lower glycemic index. Plums do have a low GI also; just, nectarines have it better.
When it comes to vitamins, plums have more of vitamins A, B6, C, and K, while nectarines have more of vitamins B1, B2, B3, B5, E, and choline.
In the category of minerals, plums are great but not higher in any mineral than nectarines; nectarines meanwhile have more copper, iron, magnesium, manganese, phosphorus, potassium, and zinc.
All in all, enjoy both. And if having dried fruit, then prunes (dried plums) are generally more widely available than dried nectarines. But if you’re choosing one fruit or the other, nectarine is the way to go.
Want to learn more?
You might like to read:
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Replacing Sugar: Top 10 Anti-Inflammatory Sweet Foods
- Top 8 Fruits That Prevent & Kill Cancer
Take care!
Share This Post

Happy Mind, Happy Life – by Dr. Rangan Chatterjee
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let’s start with a “why”. If happiness doesn’t strike you as a worthwhile goal in and of itself, Dr. Chatterjee discusses the health implications of happiness/unhappiness.
And, yes, including in studies where other factors were controlled for, so he shows how happiness/unhappiness does really have a causal role in health—it’s not just a matter of “breaking news: sick people are less happy”.
The author, a British GP (General Practitioner, the equivalent of what the US calls a “family doctor”) with decades of experience, has found a lot of value in the practice of holistic medicine. For this reason, it’s what he recommends to his patients at work, in his books, his blog, and his regular spot on a popular BBC breakfast show.
The writing style is relaxed and personable, without skimping on information density. Indeed, Dr. Chatterjee offers many pieces of holistic health advice, and dozens of practical exercises to boost your happiness and proof you against adversity.
Because, whatever motivational speakers may say, we can’t purely “think ourselves happy”; sometimes we have real external threats and bad things in life. But, we can still improve our experience of even these things, not to mention suffer less, and get through it in better shape with a smile at the end of it.
Bottom line: if you’d like to be happier and healthier (who wouldn’t?), then this book is a sure-fire way to set you on that path.
Click here to check out Happy Mind, Happy Life and upgrade yours!
Share This Post

The Uses of Delusion – by Dr. Stuart Vyse
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most of us try to live rational lives. We try to make the best decisions we can based on the information we have… And if we’re thoughtful, we even try to be aware of common logical fallacies, and overcome our personal biases too. But is self-delusion ever useful?
Dr. Stuart Vyse, psychologist and Fellow for the Committee for Skeptical Inquiry, argues that it can be.
From self-fulfilling prophecies of optimism and pessimism, to the role of delusion in love and loss, Dr. Vyse explores what separates useful delusion from dangerous irrationality.
We also read about such questions as (and proposed answers to):
- Why is placebo effect stronger if we attach a ritual to it?
- Why are negative superstitions harder to shake than positive ones?
- Why do we tend to hold to the notion of free will, despite so much evidence for determinism?
The style of the book is conversational, and captivating from the start; a highly compelling read.
Bottom line: if you’ve ever felt yourself wondering if you are deluding yourself and if so, whether that’s useful or counterproductive, this is the book for you!
Click here to check out The Uses of Delusion, and optimize yours!
Share This Post
Related Posts

What will aged care look like for the next generation? More of the same but higher out-of-pocket costs
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Aged care financing is a vexed problem for the Australian government. It is already underfunded for the quality the community expects, and costs will increase dramatically. There are also significant concerns about the complexity of the system.
In 2021–22 the federal government spent A$25 billion on aged services for around 1.2 million people aged 65 and over. Around 60% went to residential care (190,000 people) and one-third to home care (one million people).
The final report from the government’s Aged Care Taskforce, which has been reviewing funding options, estimates the number of people who will need services is likely to grow to more than two million over the next 20 years. Costs are therefore likely to more than double.
The taskforce has considered what aged care services are reasonable and necessary and made recommendations to the government about how they can be paid for. This includes getting aged care users to pay for more of their care.
But rather than recommending an alternative financing arrangement that will safeguard Australians’ aged care services into the future, the taskforce largely recommends tidying up existing arrangements and keeping the status quo.
No Medicare-style levy
The taskforce rejected the aged care royal commission’s recommendation to introduce a levy to meet aged care cost increases. A 1% levy, similar to the Medicare levy, could have raised around $8 billion a year.
The taskforce failed to consider the mix of taxation, personal contributions and social insurance which are commonly used to fund aged care systems internationally. The Japanese system, for example, is financed by long-term insurance paid by those aged 40 and over, plus general taxation and a small copayment.
Instead, the taskforce puts forward a simple, pragmatic argument that older people are becoming wealthier through superannuation, there is a cost of living crisis for younger people and therefore older people should be required to pay more of their aged care costs.
Separating care from other services
In deciding what older people should pay more for, the taskforce divided services into care, everyday living and accommodation.
The taskforce thought the most important services were clinical services (including nursing and allied health) and these should be the main responsibility of government funding. Personal care, including showering and dressing were seen as a middle tier that is likely to attract some co-payment, despite these services often being necessary to maintain independence.
The task force recommended the costs for everyday living (such as food and utilities) and accommodation expenses (such as rent) should increasingly be a personal responsibility.

Aged care users will pay more of their share for cooking and cleaning.
Lizelle Lotter/ShutterstockMaking the system fairer
The taskforce thought it was unfair people in residential care were making substantial contributions for their everyday living expenses (about 25%) and those receiving home care weren’t (about 5%). This is, in part, because home care has always had a muddled set of rules about user co-payments.
But the taskforce provided no analysis of accommodation costs (such as utilities and maintenance) people meet at home compared with residential care.
To address the inefficiencies of upfront daily fees for packages, the taskforce recommends means testing co-payments for home care packages and basing them on the actual level of service users receive for everyday support (for food, cleaning, and so on) and to a lesser extent for support to maintain independence.
It is unclear whether clinical and personal care costs and user contributions will be treated the same for residential and home care.
Making residential aged care sustainable
The taskforce was concerned residential care operators were losing $4 per resident day on “hotel” (accommodation services) and everyday living costs.
The taskforce recommends means tested user contributions for room services and everyday living costs be increased.
It also recommends that wealthier older people be given more choice by allowing them to pay more (per resident day) for better amenities. This would allow providers to fully meet the cost of these services.
Effectively, this means daily living charges for residents are too low and inflexible and that fees would go up, although the taskforce was clear that low-income residents should be protected.
Moving from buying to renting rooms
Currently older people who need residential care have a choice of making a refundable up-front payment for their room or to pay rent to offset the loans providers take out to build facilities. Providers raise capital to build aged care facilities through equity or loan financing.
However, the taskforce did not consider the overall efficiency of the private capital market for financing aged care or alternative solutions.
Instead, it recommended capital contributions be streamlined and simplified by phasing out up-front payments and focusing on rental contributions. This echoes the royal commission, which found rent to be a more efficient and less risky method of financing capital for aged care in private capital markets.
It’s likely that in a decade or so, once the new home care arrangements are in place, there will be proportionally fewer older people in residential aged care. Those who do go are likely to be more disabled and have greater care needs. And those with more money will pay more for their accommodation and everyday living arrangements. But they may have more choice too.
Although the federal government has ruled out an aged care levy and changes to assets test on the family home, it has yet to respond to the majority of the recommendations. But given the aged care minister chaired the taskforce, it’s likely to provide a good indication of current thinking.

Hal Swerissen, Emeritus Professor, La Trobe University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Women and Minorities Bear the Brunt of Medical Misdiagnosis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Charity Watkins sensed something was deeply wrong when she experienced exhaustion after her daughter was born.
At times, Watkins, then 30, had to stop on the stairway to catch her breath. Her obstetrician said postpartum depression likely caused the weakness and fatigue. When Watkins, who is Black, complained of a cough, her doctor blamed the flu.
About eight weeks after delivery, Watkins thought she was having a heart attack, and her husband took her to the emergency room. After a 5½-hour wait in a North Carolina hospital, she returned home to nurse her baby without seeing a doctor.
When a physician finally examined Watkins three days later, he immediately noticed her legs and stomach were swollen, a sign that her body was retaining fluid. After a chest X-ray, the doctor diagnosed her with heart failure, a serious condition in which the heart becomes too weak to adequately pump oxygen-rich blood to organs throughout the body. Watkins spent two weeks in intensive care.
She said a cardiologist later told her, “We almost lost you.”
Watkins is among 12 million adults misdiagnosed every year in the U.S.
In a study published Jan. 8 in JAMA Internal Medicine, researchers found that nearly 1 in 4 hospital patients who died or were transferred to intensive care had experienced a diagnostic error. Nearly 18% of misdiagnosed patients were harmed or died.
In all, an estimated 795,000 patients a year die or are permanently disabled because of misdiagnosis, according to a study published in July in the BMJ Quality & Safety periodical.
Some patients are at higher risk than others.
Women and racial and ethnic minorities are 20% to 30% more likely than white men to experience a misdiagnosis, said David Newman-Toker, a professor of neurology at Johns Hopkins School of Medicine and the lead author of the BMJ study. “That’s significant and inexcusable,” he said.
Researchers call misdiagnosis an urgent public health problem. The study found that rates of misdiagnosis range from 1.5% of heart attacks to 17.5% of strokes and 22.5% of lung cancers.
Weakening of the heart muscle — which led to Watkins’ heart failure — is the most common cause of maternal death one week to one year after delivery, and is more common among Black women.
Heart failure “should have been No. 1 on the list of possible causes” for Watkins’ symptoms, said Ronald Wyatt, chief science and chief medical officer at the Society to Improve Diagnosis in Medicine, a nonprofit research and advocacy group.
Maternal mortality for Black mothers has increased dramatically in recent years. The United States has the highest maternal mortality rate among developed countries. According to the Centers for Disease Control and Prevention, non-Hispanic Black mothers are 2.6 times as likely to die as non-Hispanic white moms. More than half of these deaths take place within a year after delivery.
Research shows that Black women with childbirth-related heart failure are typically diagnosed later than white women, said Jennifer Lewey, co-director of the pregnancy and heart disease program at Penn Medicine. That can allow patients to further deteriorate, making Black women less likely to fully recover and more likely to suffer from weakened hearts for the rest of their lives.
Watkins said the diagnosis changed her life. Doctors advised her “not to have another baby, or I might need a heart transplant,” she said. Being deprived of the chance to have another child, she said, “was devastating.”
Racial and gender disparities are widespread.
Women and minority patients suffering from heart attacks are more likely than others to be discharged without diagnosis or treatment.
Black people with depression are more likely than others to be misdiagnosed with schizophrenia.
Minorities are less likely than whites to be diagnosed early with dementia, depriving them of the opportunities to receive treatments that work best in the early stages of the disease.
Misdiagnosis isn’t new. Doctors have used autopsy studies to estimate the percentage of patients who died with undiagnosed diseases for more than a century. Although those studies show some improvement over time, life-threatening mistakes remain all too common, despite an array of sophisticated diagnostic tools, said Hardeep Singh, a professor at Baylor College of Medicine who studies ways to improve diagnosis.
“The vast majority of diagnoses can be made by getting to know the patient’s story really well, asking follow-up questions, examining the patient, and ordering basic tests,” said Singh, who is also a researcher at Houston’s Michael E. DeBakey VA Medical Center. When talking to people who’ve been misdiagnosed, “one of the things we hear over and over is, ‘The doctor didn’t listen to me.’”
Racial disparities in misdiagnosis are sometimes explained by noting that minority patients are less likely to be insured than white patients and often lack access to high-quality hospitals. But the picture is more complicated, said Monika Goyal, an emergency physician at Children’s National Hospital in Washington, D.C., who has documented racial bias in children’s health care.
In a 2020 study, Goyal and her colleagues found that Black kids with appendicitis were less likely than their white peers to be correctly diagnosed, even when both groups of patients visited the same hospital.
Although few doctors deliberately discriminate against women or minorities, Goyal said, many are biased without realizing it.
“Racial bias is baked into our culture,” Goyal said. “It’s important for all of us to start recognizing that.”
Demanding schedules, which prevent doctors from spending as much time with patients as they’d like, can contribute to diagnostic errors, said Karen Lutfey Spencer, a professor of health and behavioral sciences at the University of Colorado-Denver. “Doctors are more likely to make biased decisions when they are busy and overworked,” Spencer said. “There are some really smart, well-intentioned providers who are getting chewed up in a system that’s very unforgiving.”
Doctors make better treatment decisions when they’re more confident of a diagnosis, Spencer said.
In an experiment, researchers asked doctors to view videos of actors pretending to be patients with heart disease or depression, make a diagnosis, and recommend follow-up actions. Doctors felt far more certain diagnosing white men than Black patients or younger women.
“If they were less certain, they were less likely to take action, such as ordering tests,” Spencer said. “If they were less certain, they might just wait to prescribe treatment.”
It’s easy to see why doctors are more confident when diagnosing white men, Spencer said. For more than a century, medical textbooks have illustrated diseases with stereotypical images of white men. Only 4.5% of images in general medical textbooks feature patients with dark skin.
That may help explain why patients with darker complexions are less likely to receive a timely diagnosis with conditions that affect the skin, from cancer to Lyme disease, which causes a red or pink rash in the earliest stage of infection. Black patients with Lyme disease are more likely to be diagnosed with more advanced disease, which can cause arthritis and damage the heart. Black people with melanoma are about three times as likely as whites to die within five years.
The covid-19 pandemic helped raise awareness that pulse oximeters — the fingertip devices used to measure a patient’s pulse and oxygen levels — are less accurate for people with dark skin. The devices work by shining light through the skin; their failures have delayed critical care for many Black patients.
Seven years after her misdiagnosis, Watkins is an assistant professor of social work at North Carolina Central University in Durham, where she studies the psychosocial effects experienced by Black mothers who survive severe childbirth complications.
“Sharing my story is part of my healing,” said Watkins, who speaks to medical groups to help doctors improve their care. “It has helped me reclaim power in my life, just to be able to help others.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

The Cold Truth About Respiratory Infections
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Pathogens That Came In From The Cold

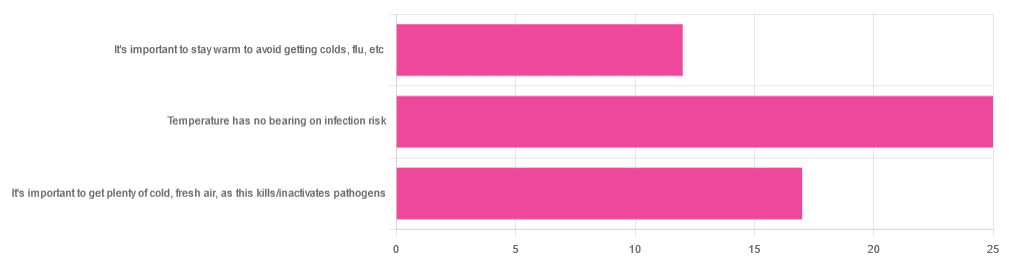
Yesterday, we asked you about your climate-themed policy for avoiding respiratory infections, and got the above-depicted, below-described, set of answers:
- About 46% of respondents said “Temperature has no bearing on infection risk”
- About 31% of respondents said “It’s important to get plenty of cold, fresh air, as this kills/inactivates pathogens”
- About 22% of respondents said “It’s important to stay warm to avoid getting colds, flu, etc”
Some gave rationales, including…
For “stay warm”:
❝Childhood lessons❞
For “get cold, fresh air”:
❝I just feel that it’s healthy to get fresh air daily. Whether it kills germs, I don’t know❞
For “temperature has no bearing”:
❝If climate issue affected respiratory infections, would people in the tropics suffer more than those in colder climates? Pollutants may affect respiratory infections, but I doubt just temperature would do so.❞
So, what does the science say?
It’s important to stay warm to avoid getting colds, flu, etc: True or False?
False, simply. Cold weather does increase the infection risk, but for reasons that a hat and scarf won’t protect you from. More on this later, but for now, let’s lay to rest the idea that bodily chilling will promote infection by cold, flu, etc.
In a small-ish but statistically significant study (n=180), it was found that…
❝There was no evidence that chilling caused any acute change in symptom scores❞
Read more: Acute cooling of the feet and the onset of common cold symptoms
Note: they do mention in their conclusion that chilling the feet “causes the onset of cold symptoms in about 10% of subjects who are chilled”, but the data does not support that conclusion, and the only clear indicator is that people who are more prone to colds generally, were more prone to getting a cold after a cold water footbath.
In other words, people who were more prone to colds remained more prone to colds, just the same.
It’s important to get plenty of cold, fresh air, as this kills/inactivates pathogens: True or False?
Broadly False, though most pathogens do have an optimal operating temperature that (for obvious reasons) is around normal human body temperature.
However, given that they don’t generally have to survive outside of a host body for long to get passed on, the fact that the pathogens may be a little sluggish in the great outdoors will not change the fact that they will be delighted by the climate in your respiratory tract as soon as you get back into the warm.
With regard to the cold air not being a reliable killer/inactivator of pathogens, we call to the witness stand…
Polar Bear Dies From Bird Flu As H5N1 Spreads Across Globe
(it was found near Utqiagvik, one of the northernmost communities in Alaska)
Because pathogens like human body temperature, raising the body temperature is a way to kill/inactivate them: True or False?
True! Unfortunately, it’s also a way to kill us. Because we, too, cannot survive for long above our normal body temperature.
So, for example, bundling up warmly and cranking up the heating won’t necessarily help, because:
- if the temperature is comfortable for you, it’s comfortable for the pathogen
- if the temperature is dangerous to the pathogen, it’s dangerous to you too
This is why the fever response evolved, and/but why many people with fevers die anyway. It’s the body’s way of playing chicken with the pathogen, challenging “guess which of us can survive this for longer!”
Temperature has no bearing on infection risk: True or False?
True and/or False, circumstantially. This one’s a little complex, but let’s break it down to the essentials.
- Temperature has no direct effect, for the reasons we outlined above
- Temperature is often related to humidity, which does have an effect
- Temperature does tend to influence human behavior (more time spent in open spaces with good ventilation vs more time spent in closed quarters with poor ventilation and/or recycled air), which has an obvious effect on transmission rates
The first one we covered, and the third one is self-evident, so let’s look at the second one:
Temperature is often related to humidity, which does have an effect
When the environmental temperature is warmer, water droplets in the air will tend to be bigger, and thus drop to the ground much more quickly.
When the environmental temperature is colder, water droplets in the air will tend to be smaller, and thus stay in the air for longer (along with any pathogens those water droplets may be carrying).
Some papers on the impact of this:
- Cold temperature and low humidity are associated with increased occurrence of respiratory tract infections
- A Decrease in Temperature and Humidity Precedes Human Rhinovirus Infections in a Cold Climate
So whatever temperature you like to keep your environment, humidity is a protective factor against respiratory infections, and dry air is a risk factor.
So, for example:
- If the weather doesn’t suit having good ventilation, a humidifier is a good option
- Being in an airplane is one of the worst places to be for this, outside of a hospital
Don’t have a humidifier? Here’s an example product on Amazon, but by all means shop around.
A crock pot with hot water in and the lid off is also a very workable workaround too
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: