It’s Not Fantastic To Be Plastic
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We Are Such Stuff As Bottles Are Made Of
We’ve written before about PFAS, often found in non-stick coatings and the like:
PFAS Exposure & Cancer: The Numbers Are High
Today we’re going to be talking about microplastics & nanoplastics!
What are microplastics and nanoplastics?
Firstly, they’renot just the now-banned plastic microbeads that have seen some use is toiletries (although those are classified as microplastics too).
Many are much smaller than that, and if they get smaller than a thousandth of a millimeter, then they get the additional classification of “nanoplastic”.
In other words: not something that can be filtered even if you were to use a single-micron filter. The microplastics would still get through, for example:
Scientists find about a quarter million invisible nanoplastic particles in a liter of bottled water
And unfortunately, that’s bad:
❝What’s disturbing is that small particles can appear in different organs and may cross membranes that they aren’t meant to cross, such as the blood-brain barrier❞
Note: they’re crossing the same blood-brain barrier that many of our nutrients and neurochemicals are too big to cross.
These microplastics are also being found in arterial plaque
What makes arterial plaque bad for the health is precisely its plasticity (the arterial walls themselves are elastic), so you most certainly do not want actual plastic being used as part of the cement that shouldn’t even be lining your arteries in the first place:
Microplastics found in artery plaque linked with higher risk of heart attack, stroke and death
❝In this study, patients with carotid artery plaque in which MNPs were detected had a higher risk of a composite of myocardial infarction, stroke, or death from any cause at 34 months of follow-up than those in whom MNPs were not detected❞
~ Dr. Raffaele Marfella et al.
(MNP = Micro/Nanoplastics)
Source: Microplastics and Nanoplastics in Atheromas and Cardiovascular Events
We don’t know how bad this is yet
There are various ways this might not be as bad as it looks (the results may not be repeated, the samples could have been compromised, etc), but also, perhaps cynically but nevertheless honestly, it could also be worse than we know yet—only more experiments being done will tell us which.
In the meantime, here’s a rundown of what we do and don’t know:
Study links microplastics with human health problems—but there’s still a lot we don’t know
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Working Smarter < Working Brighter!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to working smarter, not harder, there’s plenty of advice and honestly, it’s mostly quite sensible. For example:
(Nice to see they featured a method we talked about last week—great minds!)
But, as standards of productivity rise, the goalposts get moved too, and the treadmill just keeps on going…
- 49% of entrepreneurs say they’ve struggled with some kind of mental illness
- Millennial women are one of the workforce groups at the highest risk of anxiety
- About 7 in 10 millennials experience burnout at work
Not that these things are confined to Millennials, by any stretch, but Millennials make up a huge portion of working people. Ideally, this age group should be able to bring the best of both worlds to the workplace by combining years of experience with youthful energy.
So clearly something is going wrong; the question is: what can be done about it?
Workers of the World, Unwind
A knee-jerk response might be “work to rule”—a tactic long-used by disgruntled exploited workers to do no more than the absolute minimum required to not get fired. And it’s arguably better for them than breaking themselves at work, but that’s not exactly enriching, is it?
This is Brittany Berger, founder of “Work Brighter”.
She’s a content marketing consultant, mental health advocate, and (in her words) a highly ridiculous human who always has a pop culture reference at the ready.
What, besides pop culture references, is she bringing to the table? What is Working Brighter?
❝Working brighter means going beyond generic “work smarter” advice on the internet and personalizing it to work FOR YOU. It means creating your own routines for work, productivity, and self-care.❞
Brittany Berger
Examples of working brighter include…
Asking:
- What would your work involve, if it were more fun?
- How can you make your work more comfortable for you?
- What changes could you make that would make your work more sustainable (i.e., to avoid burnout)?
Remembering:
- Mental health is just health
- Self-care is a “soft skill”
- Rest is work when it’s needed
This is not one of those “what workers really want is not more pay, it’s beanbags” things, by the way (but if you want a beanbag, then by all means, get yourself a beanbag).
It’s about making time to rest, it’s about having the things that make you feel good while you’re working, and making sure you can enjoy working. You’re going to spend a lot of your life doing it; you might as well enjoy it.
❝Nobody goes to their deathbed wishing they’d spent more time at the office❞
Anon
On the contrary, having worked too hard is one of the top reported regrets of the dying!
Article: The Top Five Regrets Of The Dying
And no, they don’t wish they’d “worked smarter, not harder”. They wish (also in the above list, in fact) that they’d had the courage to live a life more true to themselves.
You can do that in your work. Whatever your work is. And if your work doesn’t permit that (be it the evil boss trope, or even that you are the boss and your line of work just doesn’t work that way), time to change that up. Stop focusing on what you can’t do, and look for what you can do.
Spoiler: you can have a blast just trying things out!
That doesn’t mean you should quit your job, or replace your PC with a Playstation, or whatever.
It just means that you deserve comfort and happiness while working, and around your work!
Need a helping hand getting started?
- Create your own self-care plan to avoid burnout
- ⏳ Complete your first “time audit”
- ❣️ Zip through to self-awareness with bullet-journalling
Like A Boss
And pssst, if you’re a business-owner who is thinking “but I have quotas to meet”, your customers are going to love your staff being happier, and will enjoy their interactions with your company much more. Or if your staff aren’t customer-facing, then still, they’ll work better when they enjoy doing it. This isn’t rocket science, but all too many companies give a cursory nod to it before proceeding to ignore it for the rest of the life of the company.
So where do you start, if you’re in those particular shoes?
Read on…
*straightens tie because this is the serious bit* —just kidding, I’m wearing my comfiest dress and fluffy-lined slipper-socks. But that makes this absolutely no less serious:
The Institute for Health and Productivity Management (IHPM) and WorkPlace Wellness Alliance (WPWA) might be a good place to get you on the right track!
❝IHPM/WPWA is a global nonprofit enterprise devoted to establishing the full economic value of employee health as a business asset—a neglected investment in the increased productivity of human capital.
IHPM helps employers identify the full economic cost impact of employee health issues on business performance, design and implement the best programs to reduce this impact by improving functional health and productivity, and measure the success of their efforts in financial terms.❞
The Institute for Health and Productivity Management
They offer courses and consultations, but they also have free downloadables and videos, which are awesome and in many cases may already be enough to seriously improve things for your business already:
Check Out IHPM’s Resources Here!
What can you do to make your working life better for you? We’d love to hear about any changes you make inspired by Brittany’s work—you can always just hit reply, and we’re always glad to hear from you!
Share This Post
-
How To Rest More Efficiently (Yes, Really)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Rest More Efficiently (Yes, Really)
We’ve talked before about how to recover more quickly after a workout, especially if you overdid it. There are a lot of tips in that article, so by all means check it out if you didn’t catch it at the time!
That was very specific to recovering from exercise, though. Today we’re looking at something a little different, a little more holistic.
You’re busier than you think
Maybe your life is an obvious blur of busy-ness. Maybe it’s not. But either way, you’re almost certainly busier than you think. Especially on a cellular level.
Your resting metabolic rate (RMR), or how many calories you burn while at rest (i.e., calories used just to keep you alive) will depend on various factors including age, sex, weight, body composition, and other things.
That said, it’ll probably be between 1000 and 2000 calories per day. You can get a rough idea of what it might be for you, using this calculator:
How Many Calories Do You Burn a Day at Rest (Doing Nothing)?
So if ever you wonder why you feel so exhausted, despite having done nothing, it could be that your body was busy:
- Metabolizing, generally (did you have a big meal?)
- Fighting an illness (bacterial or viral infection, for example)
- Fighting an imaginary illness and creating a real one in the process (stress, inflammation, etc)
- Recovering/rebuilding from something you did yesterday or even before that
- Thinking (your brain is your largest organ by mass, and consumes the most calories by far)
Your brain does not get a free pass on being part of your body! Just like if a certain muscle group were working out constantly for 16 hours you’d be feeling pretty tired, the same goes for the organ that is your brain, if it’s been working out constantly.
Your body is a composite organism—take advantage of that
Dolphins can shut down half of their brain at once, to let each hemisphere of the brain sleep independently in shifts. We (except in the case of split brain patients, where the corpus callosum has been severed) can’t do that, but we can let different parts of the organism that is our body work in shifts.
This is the real meaning of “a change is as a good as a rest”:
If you’ve been doing cognitive work (at your desk perhaps, maybe managing a spreadsheet, say), then taking a break to do crosswords will not, actually, give you break. Because you’re still sitting manipulating letters and numbers. As far as your brain (still having to do work!) is concerned, it’s basically the same. Nor will checking out social media; you’re still sitting examining a screen.
Instead, time to get physically active. Literally just doing the washing up would be a better break! Some yoga or Pilates would be perfect.
In contrast, if you’ve been doing a vigorous bit of gardening, then for example taking a break to lift weights isn’t going to be a break, because again you just switched to a similar task.
Better to pick up that book you’ve been meaning to read, or the crosswords we mentioned earlier. Or just lounge in your nicely-gardened garden.
The important thing is: to not require the same resources from the body (including the brain, it’s still part of the body) that you have been.
For more specific tips than we have room for here today, check out:
How to Take Better Breaks at Work, According to Research
Give your metabolism a break too
Not completely—you don’t need to be put into cryostasis or anything.
But, give your metabolism a rest, in relative terms. Intermittent fasting is great for precisely this; it lets your body rest and reset.
See: Intermittent Fasting: we sort the science from the hype!
So does the practice of meditation, by the way. You don’t have to get fancy with it, either:
Check out: No Frills, Evidence-Based Mindfulness
Enjoy, and rest well!
Share This Post
-
When Bad Joints Stop You From Exercising (5 Things To Change)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The first trick to exercising with bad joints is to have better joints.
Now, this doesn’t necessarily mean you can take a supplement and magically your joint problems will be cured, but there are adjustable lifestyle factors that can and will make things relatively better or worse.
We say “and will”, because you don’t get a choice in that part. Everything we do, every little choice in our day, makes our health a little better or a little worse in some aspect(s). But we do get a choice between “relatively better” and “relatively worse”.
With that in mind, do check out:
- Avoiding/Managing Osteoarthritis
- Avoiding/Managing Rheumatoid Arthritis
- How To Really Look After Your Joints
Ok, you have bad joints though; what next?
Let’s assume you’re doing your best with the above, and/or have simply decided not to, which is your call. You know your circumstances best. Either way, your joints are still not in sufficiently good condition to be able to exercise the way you’d like.
First, the obvious: enjoy low-impact exercises
For example:
- Swimming
- Yoga (much more appropriate here than the commonly-paired “and tai chi”)*
- Isometric exercises (i.e. exercise without movement, e.g. squeezing things, or stationary stability exercises)
*This is not to say that tai chi is bad. But if your problem is specifically your knees, there are many movements in most forms of tai chi that require putting the majority of one’s weight on one bent leg, which means the knee of that leg is going to suffer. If your knees are fine, then this won’t be an issue and it will simply continue strengthening your knees without discomfort. But they have to be fine first.
See also: Exercising With Osteoporosis
Second: support your joints through a full range of motion
If you have bad joints, you probably know that there’s an unfortunate paradox whereby you get to choose between:
- Exercise, and inflame your joints
- Rest, and your joints seize up
This is the way to get around that damaging dilemma.
Moving your joints through a full range of motion regularly is critical for their maintenance, so do that in a way that isn’t straining them:
If it’s your shoulders, for example, you can do (slow, gentle!) backstroke or front-crawl or butterfly motions while standing in the comfort of your living room.
If it’s your knees, then supported squats can do you a world of good. That means, squat in front of a table or other stable object, with your fingertips (or as much of your hands as you need) on it, to take a portion of your weight (it can be a large portion; that’s fine too!) while you go through the full range of motion of the squat. Repeat.
And so forth for other joints.
See also: The Most Underrated Hip Mobility Exercise (Not Stretching)
Third: work up slowly, and stop early
You can do exercises that involve impact, and if you live a fairly normal life, you’ll probably have to (walking is an impact exercise). You can also enjoy cycling (low-impact, but not so low-impact as we discussed in the last section) and work up to running if you want to.
However…
While building up your joints’ mobility and strength, it is generally a good idea to stop before you think you need to.
This means that it’s important to do those exercises in a way that you can stop early. For example, an exercise bike or a treadmill can be a lot of use here, so that you don’t find you need to stop for the day while miles from your house.
If you get such a device, it doesn’t even have to be fancy and/or expensive. This writer got herself an inexpensive exercise bike like this one, and it’s perfectly adequate.
Fourth: prioritize recovery, even if it doesn’t feel like you need it
Everyone should do this anyway, but if your joints are bad, it goes double:
Overdone It? How To Speed Up Recovery After Exercise (According To Actual Science)
Fifth: get professional help
Physiotherapists are great for this. Find one, and take their advice for your specific body and your specific circumstances and goals.
Take care!
Share This Post
Related Posts
-
What is PMDD?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Premenstrual dysphoric disorder (PMDD) is a mood disorder that causes significant mental health changes and physical symptoms leading up to each menstrual period.
Unlike premenstrual syndrome (PMS), which affects approximately three out of four menstruating people, only 3 percent to 8 percent of menstruating people have PMDD. However, some researchers believe the condition is underdiagnosed, as it was only recently recognized as a medical diagnosis by the World Health Organization.
Read on to learn more about its symptoms, the difference between PMS and PMDD, treatment options, and more.
What are the symptoms of PMDD?
People with PMDD typically experience both mood changes and physical symptoms during each menstrual cycle’s luteal phase—the time between ovulation and menstruation. These symptoms typically last seven to 14 days and resolve when menstruation begins.
Mood symptoms may include:
- Irritability
- Anxiety and panic attacks
- Extreme or sudden mood shifts
- Difficulty concentrating
- Depression and suicidal ideation
Physical symptoms may include:
- Fatigue
- Insomnia
- Headaches
- Changes in appetite
- Body aches
- Bloating
- Abdominal cramps
- Breast swelling or tenderness
What is the difference between PMS and PMDD?
Both PMS and PMDD cause emotional and physical symptoms before menstruation. Unlike PMS, PMDD causes extreme mood changes that disrupt daily life and may lead to conflict with friends, family, partners, and coworkers. Additionally, symptoms may last longer than PMS symptoms.
In severe cases, PMDD may lead to depression or suicide. More than 70 percent of people with the condition have actively thought about suicide, and 34 percent have attempted it.
What is the history of PMDD?
PMDD wasn’t added to the Diagnostic and Statistical Manual of Mental Disorders until 2013. In 2019, the World Health Organization officially recognized it as a medical diagnosis.
References to PMDD in medical literature date back to the 1960s, but defining it as a mental health and medical condition initially faced pushback from women’s rights groups. These groups were concerned that recognizing the condition could perpetuate stereotypes about women’s mental health and capabilities before and during menstruation.
Today, many women-led organizations are supportive of PMDD being an official diagnosis, as this has helped those living with the condition access care.
What causes PMDD?
Researchers don’t know exactly what causes PMDD. Many speculate that people with the condition have an abnormal response to fluctuations in hormones and serotonin—a brain chemical impacting mood— that occur throughout the menstrual cycle. Symptoms fully resolve after menopause.
People who have a family history of premenstrual symptoms and mood disorders or have a personal history of traumatic life events may be at higher risk of PMDD.
How is PMDD diagnosed?
Health care providers of many types, including mental health providers, can diagnose PMDD. Providers typically ask patients about their premenstrual symptoms and the amount of stress those symptoms are causing. Some providers may ask patients to track their periods and symptoms for one month or longer to determine whether those symptoms are linked to their menstrual cycle.
Some patients may struggle to receive a PMDD diagnosis, as some providers may lack knowledge about the condition. If your provider is unfamiliar with the condition and unwilling to explore treatment options, find a provider who can offer adequate support. The International Association for Premenstrual Disorders offers a directory of providers who treat the condition.
How is PMDD treated?
There is no cure for PMDD, but health care providers can prescribe medication to help manage symptoms. Some medication options include:
- Selective serotonin reuptake inhibitors (SSRIs), a class of antidepressants that regulate serotonin in the brain and may improve mood when taken daily or during the luteal phase of each menstrual cycle.
- Hormonal birth control to prevent ovulation-related hormonal changes.
- Over-the-counter pain medication like Tylenol, which can ease headaches, breast tenderness, abdominal cramping, and other physical symptoms.
Providers may also encourage patients to make lifestyle changes to improve symptoms. Those lifestyle changes may include:
- Limiting caffeine intake
- Eating meals regularly to balance blood sugar
- Exercising regularly
- Practicing stress management using breathing exercises and meditation
- Having regular therapy sessions and attending peer support groups
For more information, talk to your health care provider.
If you or anyone you know is considering suicide or self-harm or is anxious, depressed, upset, or needs to talk, call the Suicide & Crisis Lifeline at 988 or text the Crisis Text Line at 741-741. For international resources, here is a good place to begin.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Guava vs Pineapple – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
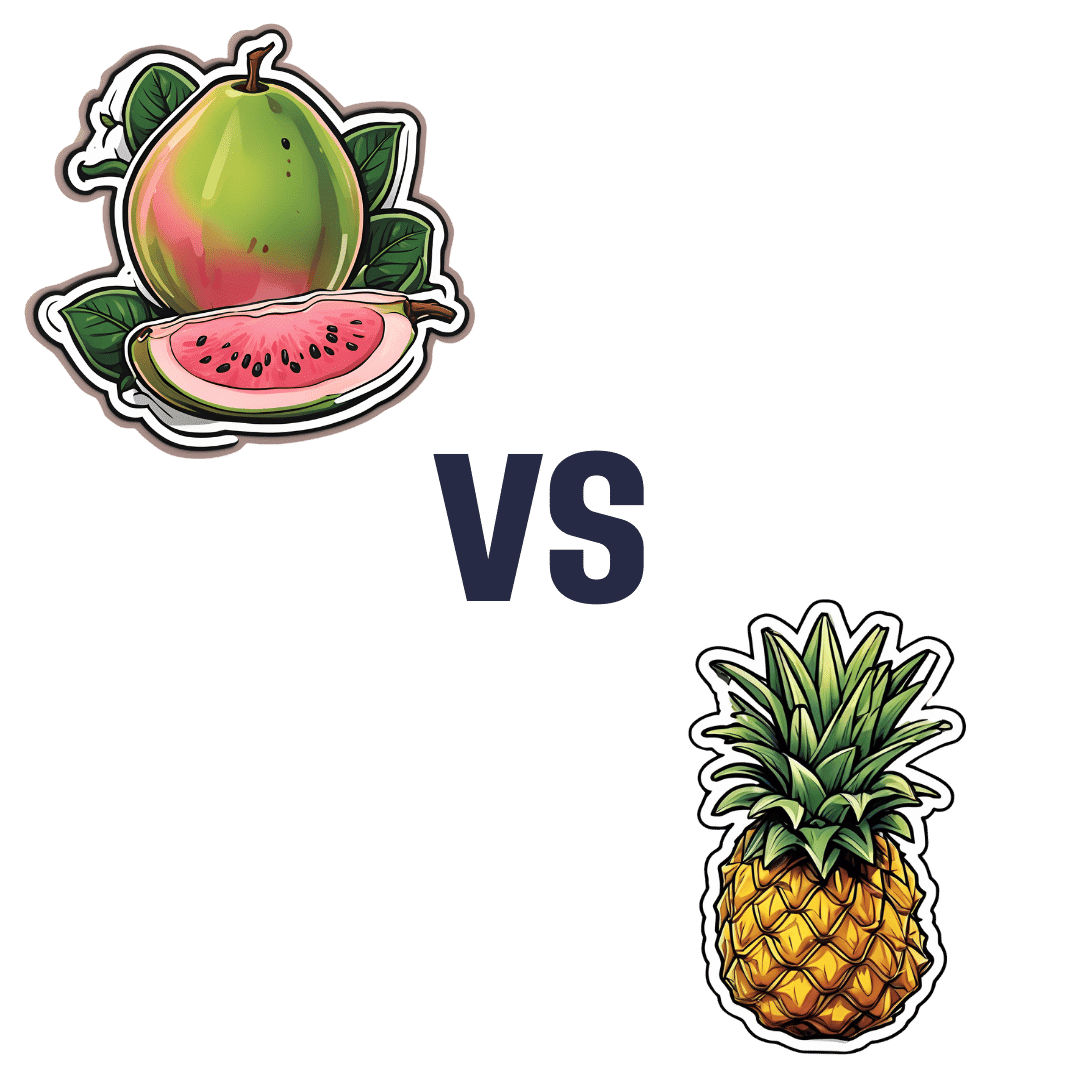
When comparing guava to pineapple, we picked the guava.
Why?
Pineapple is great, but guava just beats it in most ways:
In terms of macros, guava has nearly 4x the fiber and nearly 5x the protein, for the same carbs, giving it the notably lower glycemic index. An easy win for guava in this category.
In the category of vitamins, guava has a lot more of vitamins A, B2, B3, B5, B9, C, E, K, and choline, while pineapple has marginally more vitamin B1. Another clear win for guava.
When it comes to minerals, guava has more calcium, copper, magnesium, phosphorus, potassium, selenium, and zinc, while pineapple has more iron and manganese. One more win for guava.
One big thing in pineapple’s favor is that it contains bromelain, which is an enzyme* found in pineapple (and only in pineapple), that has many very healthful properties, some of them unique to bromelain (and thus: unique to pineapple)
*actually a combination of enzymes, but most often referred to collectively in the singular. But when you do see it referred to as “they”, that’s what that means.
However cool that is, we think it unfair to weight it against guava winning in every other category, so we still say guava gets the overall win.
Of course, enjoy either or both; diversity is good!
Want to learn more?
You might like:
Let’s Get Fruity: Bromelain vs Inflammation & Much More
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How to Do the Work – by Dr. Nicole LaPera
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We have reviewed some self-therapy books before, and they chiefly have focused on CBT and mindfulness, which are great. This one’s different.
Dr. Nicole LaPera has a bolder vision for what we can do for ourselves. Rather than giving us some worksheets for unraveling cognitive distortions or clearing up automatic negative thoughts, she bids us treat the cause, rather than the symptom.
For most of us, this will be the life we have led. Now, we cannot change the parenting style(s) we received (or didn’t), get a redo on childhood, avoid mistakes we made in our adolescence, or face adult life with the benefit of experience we gained right after we needed it most. But we can still work on those things if we just know how.
The subtitle of this book promsies that the reader can/will “recognise your patterns, heal from your past, and create your self”.
That’s accurate, for the content of the book and the advice it gives.
Dr. LaPera’s focus is on being our own best healer, and reparenting our own inner child. Giving each of us the confidence in ourself; the love and care and/but also firm-if-necessary direction that a (good) parent gives a child, and the trust that a secure child will have in the parent looking after them. Doing this for ourselves, Dr. LaPera holds, allows us to heal from traumas we went through when we perhaps didn’t quite have that, and show up for ourselves in a way that we might not have thought about before.
If the book has a weak point, it’s that many of the examples given are from Dr. LaPera’s own life and experience, so how relatable the specific examples will be to any given reader may vary. But, the principles and advices stand the same regardless.
Bottom line: if you’d like to try self-therapy on a deeper level than CBT worksheets, this book is an excellent primer.
Click here to check out How To Do The Work, and empower yourself to indeed do the work!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: