Menopause, & When Not To Let Your Guard Down
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.

This is Dr. Jessica Shepherd, a physician Fellow of the American College of Obstetricians & Gynecologists, CEO at Sanctum Medical & Wellness, and CMO at Hers.
She’s most well-known for her expertise in the field of the menopause. So, what does she want us to know?
Untreated menopause is more serious than most people think
Beyond the famous hot flashes, there’s also the increased osteoporosis risk, which is more well-known at least amongst the health-conscious, but oft-neglected is the increased cardiovascular disease risk:
What Menopause Does To The Heart
…and, which a lot of Dr. Shepherd’s work focuses on, it also increases dementia risk; she cites that 60–80% of dementia cases are women, and it’s also established that it progresses more quickly in women than men too, and this is associated with lower estrogen levels (not a problem for men, because testosterone does it for them) which had previously been a protective factor, but in untreated menopause, was no longer there to help:
Alzheimer’s Sex Differences May Not Be What They Appear
Treated menopause is safer than many people think
The Women’s Health Initiative (WHI) study, conducted in the 90s and published in 2002, linked HRT to breast cancer, causing fear, but it turned out that this was quite bad science in several ways and the reporting was even worse (even the flawed data did not really support the conclusion, much less the headlines); it was since broadly refuted (and in fact, it can be a protective factor, depending on the HRT regimen), but fearmongering headlines made it to mainstream news, whereas “oopsies, never mind, we take that back” didn’t.
The short version of the current state of the science is: breast cancer risk varies depending on age, HRT type, and dosage; some kinds of HRT can increase the risk marginally in those older than 60, but absolute risk is low compared to placebo, and taking estrogen alone can reduce risk at any age in the event of not having a uterus (almost always because of having had a hysterectomy; as a quirk, it is possible to be born without, though).
It’s worth noting that even in the cases where HRT marginally increased the risk of breast cancer, it significantly decreased the risk of cancers in total, as well fractures and all-cause-mortality compared to the placebo group.
In other words, it might be worth having a 0.12% risk of breast cancer, to avoid the >30% risk of osteoporosis, which can ultimately be just as fatal (without even looking at the other things the HRT is protective against).
However! In the case of those who already have (or have had) breast cancer, increasing estrogen levels can indeed make that worse/return, and it becomes more complicated in cases where you haven’t had it, but there is a family history of it, or you otherwise know you have the gene for it.
You can read more about HRT and breast cancer risk (increases and decreases) here:
…and about the same with regard to HMT, here:
The Hormone Therapy That Reduces Breast Cancer Risk & More
Lifestyle matters, and continues to matter
Menopause often receives the following attention from people:
- Perimenopause: “Is this menopause?”
- Menopause: “Ok, choices to make about HRT or not, plus I should watch out for osteoporosis”
- Postmenopause: “Yay, that’s behind me now, back to the new normal”
The reality, Dr. Shepherd advises, is that “postmenopause” is a misnomer because if it’s not being treated, then the changes are continuing to occur in your body.
This is a simple factor of physiology; your body is always rebuilding itself, will never stop until you die, and in untreated menopause+postmenopause, it’s now doing it without much estrogen.
So, you can’t let your guard down!
Thus, she recommends: focus on maintaining muscle mass, bone health, and cardiovascular health. If you focus on those things, the rest (including your brain, which is highly dependent on cardiovascular health) will mostly take care of itself.
Because falls and fractures, particularly hip fractures, drastically reduce quality and length of life in older adults, it is vital to avoid those, and try to be sufficiently robust so that if you do go A over T, you won’t injure yourself too badly, because your bones are strong. As a bonus, the same things (especially that muscle mass we talked about) will help you avoid falling in the first place, by improving stability.
See also: Resistance Is Useful! (Especially As We Get Older)
And about falls specifically: Fall Special: Be Robust, Mobile, & Balanced!
Want to know more from Dr. Shepherd?
You might like this book of hers that we reviewed not long back:
Generation M – by Dr. Jessica Shepherd
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Getting Flexible, Starting As An Adult: How Long Does It Really Take?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Aleks Brzezinska didn’t start stretching until she was 21, and here’s what she found:
We’ll not stretch the truth
A lot of stretching programs will claim “do the splits in 30 days” or similar, and while this may occasionally be true, usually it’ll take longer.
Brzezinska started stretching seriously when she was 21, and made significant flexibility gains between the ages of 21 and 23 with consistent practice. Since then, she’s just maintained her flexibility.
There are facts that affect progress significantly, such as:
- Anatomy: body structure, age, and joint flexibility do influence flexibility; starting younger and/or having hypermobile joints does make it easier.
- Consistency: regular practice (2–3 times a week) is crucial, but avoid overdoing it, especially when sore.
- Lifestyle: weightlifting, running, and similar activities can tighten muscles, making flexibility harder to achieve.
- Hydration: staying hydrated is important for muscle flexibility.
She also recommends incorporating a variety of different stretching types, rather than just one method, for example passive stretching, active stretching, Proprioceptive Neuromuscular Facilitation (PNF) stretching, and mobility work.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Jasmine McDonald’s Ballet Stretching Routine
Take care!
Share This Post
-
Microplastics are in our brains. How worried should I be?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Plastic is in our clothes, cars, mobile phones, water bottles and food containers. But recent research adds to growing concerns about the impact of tiny plastic fragments on our health.
A study from the United States has, for the first time, found microplastics in human brains. The study, which has yet to be independently verified by other scientists, has been described in the media as scary, shocking and alarming.
But what exactly are microplastics? What do they mean for our health? Should we be concerned?
Daniel Megias/Shutterstock What are microplastics? Can you see them?
We often consider plastic items to be indestructible. But plastic breaks down into smaller particles. Definitions vary but generally microplastics are smaller than five millimetres.
This makes some too small to be seen with the naked eye. So, many of the images the media uses to illustrate articles about microplastics are misleading, as some show much larger, clearly visible pieces.
Microplastics have been reported in many sources of drinking water and everyday food items. This means we are constantly exposed to them in our diet.
Such widespread, chronic (long-term) exposure makes this a serious concern for human health. While research investigating the potential risk microplastics pose to our health is limited, it is growing.
How about this latest study?
The study looked at concentrations of microplastics in 51 samples from men and women set aside from routine autopsies in Albuquerque, New Mexico. Samples were from the liver, kidney and brain.
These tiny particles are difficult to study due to their size, even with a high-powered microscope. So rather than trying to see them, researchers are beginning to use complex instruments that identify the chemical composition of microplastics in a sample. This is the technique used in this study.
The researchers were surprised to find up to 30 times more microplastics in brain samples than in the liver and kidney.
They hypothesised this could be due to high blood flow to the brain (carrying plastic particles with it). Alternatively, the liver and kidneys might be better suited to dealing with external toxins and particles. We also know the brain does not undergo the same amount of cellular renewal as other organs in the body, which could make the plastics linger here.
The researchers also found the amount of plastics in brain samples increased by about 50% between 2016 and 2024. This may reflect the rise in environmental plastic pollution and increased human exposure.
The microplastics found in this study were mostly composed of polyethylene. This is the most commonly produced plastic in the world and is used for many everyday products, such as bottle caps and plastic bags.
This is the first time microplastics have been found in human brains, which is important. However, this study is a “pre-print”, so other independent microplastics researchers haven’t yet reviewed or validated the study.
The most common plastic found was polyethylene, which is used to make plastic bags and bottle caps. Maciej Bledowski/Shutterstock How do microplastics end up in the brain?
Microplastics typically enter the body through contaminated food and water. This can disrupt the gut microbiome (the community of microbes in your gut) and cause inflammation. This leads to effects in the whole body via the immune system and the complex, two-way communication system between the gut and the brain. This so-called gut-brain axis is implicated in many aspects of health and disease.
We can also breathe in airborne microplastics. Once these particles are in the gut or lungs, they can move into the bloodstream and then travel around the body into various organs.
Studies have found microplastics in human faeces, joints, livers, reproductive organs, blood, vessels and hearts.
Microplastics also migrate to the brains of wild fish. In mouse studies, ingested microplastics are absorbed from the gut into the blood and can enter the brain, becoming lodged in other organs along the way.
To get into brain tissue, microplastics must cross the blood-brain-barrier, an intricate layer of cells that is supposed to keep things in the blood from entering the brain.
Although concerning, this is not surprising, as microplastics must cross similar cell barriers to enter the urine, testes and placenta, where they have already been found in humans.
Is this a health concern?
We don’t yet know the effects of microplastics in the human brain. Some laboratory experiments suggest microplastics increase brain inflammation and cell damage, alter gene expression and change brain structure.
Aside from the effects of the microplastic particles themselves, microplastics might also pose risks if they carry environmental toxins or bacteria into and around the body.
Various plastic chemicals could also leach out of the microplastics into the body. These include the famous hormone-disrupting chemicals known as BPAs.
But microplastics and their effects are difficult to study. In addition to their small size, there are so many different types of plastics in the environment. More than 13,000 different chemicals have been identified in plastic products, with more being developed every year.
Microplastics are also weathered by the environment and digestive processes, and this is hard to reproduce in the lab.
A goal of our research is to understand how these factors change the way microplastics behave in the body. We plan to investigate if improving the integrity of the gut barrier through diet or probiotics can prevent the uptake of microplastics from the gut into the bloodstream. This may effectively stop the particles from circulating around the body and lodging into organs.
How do I minimise my exposure?
Microplastics are widespread in the environment, and it’s difficult to avoid exposure. We are just beginning to understand how microplastics can affect our health.
Until we have more scientific evidence, the best thing we can do is reduce our exposure to plastics where we can and produce less plastic waste, so less ends up in the environment.
An easy place to start is to avoid foods and drinks packaged in single-use plastic or reheated in plastic containers. We can also minimise exposure to synthetic fibres in our home and clothing.
Sarah Hellewell, Senior Research Fellow, The Perron Institute for Neurological and Translational Science, and Research Fellow, Faculty of Health Sciences, Curtin University; Anastazja Gorecki, Teaching & Research Scholar, School of Health Sciences, University of Notre Dame Australia, and Charlotte Sofield, PhD Candidate, studying microplastics and gut/brain health, University of Notre Dame Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
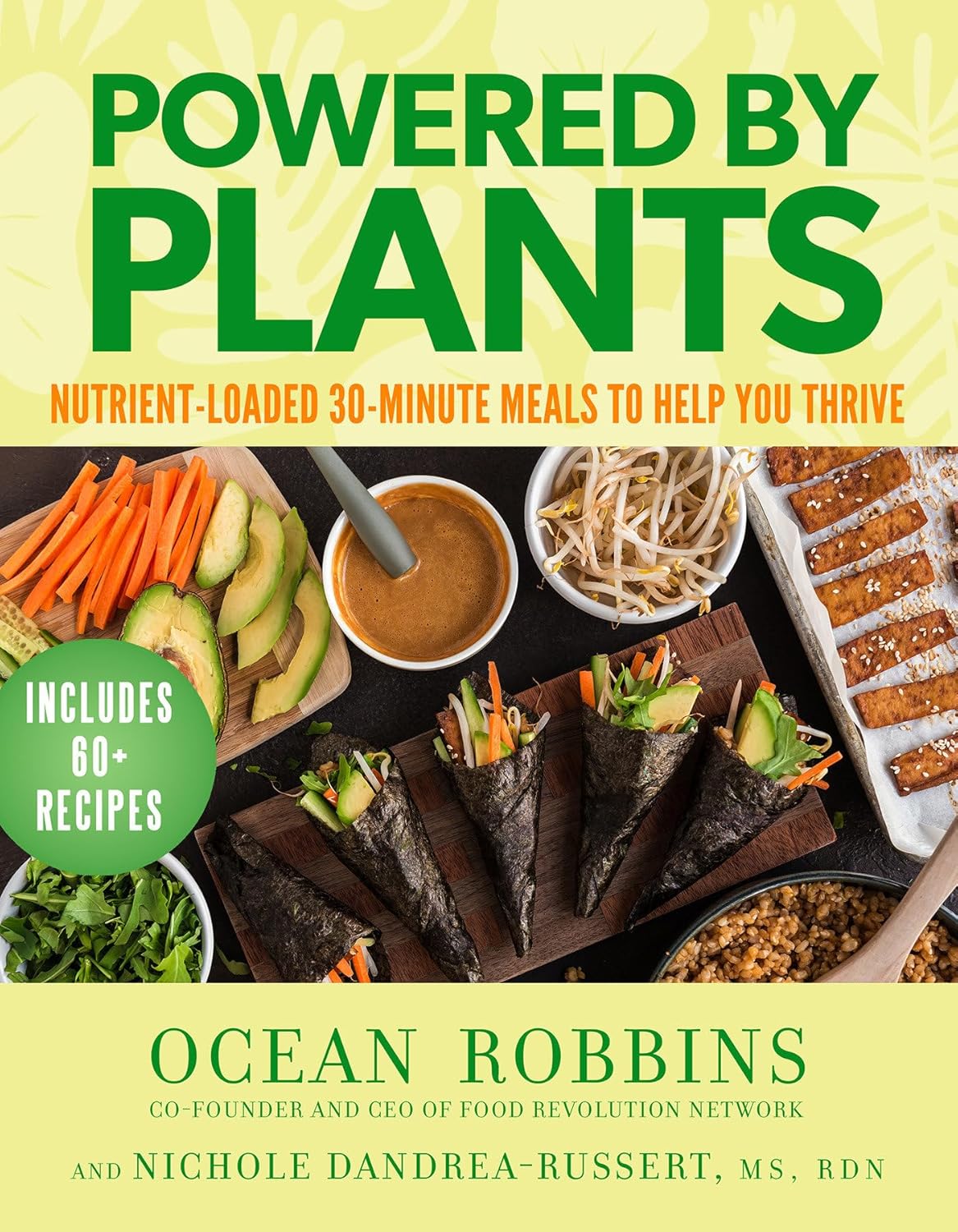
Powered by Plants – by Ocean Robbins & Nichole Dandrea-Russert
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Of the two authors, the former is a professional public speaker, and the latter is a professional dietician. As a result, we get a book that is polished and well-presented, while actually having a core of good solid science (backed up with plenty of references).
There’s an introductory section that’s all about the “notable nutrients”, that will be focused on in the ingredients choices for the recipes in the rest of the book.
The recipes themselves are simple enough to do quickly, yet interesting enough that you’ll want to do them, and certainly they contain all the plant-based nutrient-density you might expect.
Bottom line: if you’d like to expand your plant-based cooking with a focus on nutrition and ease without sacrificing fun, then this is a great cookbook for that.
Click here to check out Powered by Plants, and get powered by plants!
Share This Post
Related Posts
-
Ozempic’s cousin drug liraglutide is about to get cheaper. But how does it stack up?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
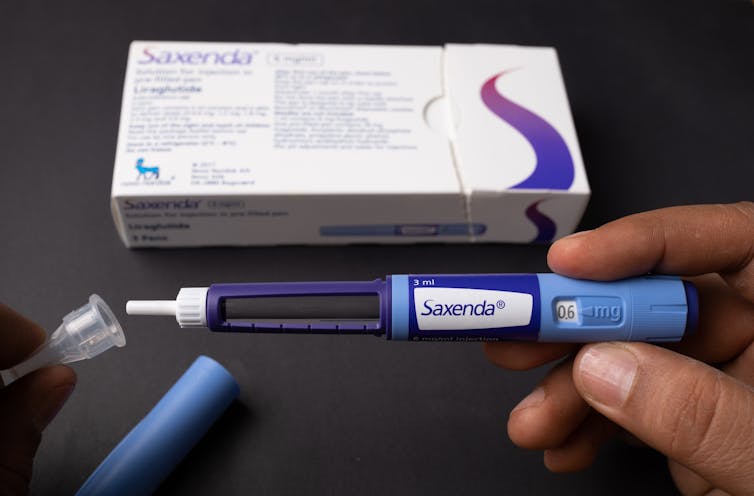
Fourteen years ago, the older drug cousin of semaglutide (Ozempic and Wegovy) came onto the market. The drug, liraglutide, is sold under the brand names Victoza and Saxenda.
Patents for Victoza and Saxenda have now expried. So other drug companies are working to develop “generic” versions. These are likely be a fraction of current cost, which is around A$400 a month.
So how does liraglutide compare with semaglutide?
Halfpoint/Shutterstock How do these drugs work?
Liraglutide was not originally developed as a weight-loss treatment. Like semaglutide (Ozempic), it originally treated type 2 diabetes.
The class of drugs liraglutide and semaglutide belong to are known as GLP-1 mimetics, meaning they mimic the natural hormone GLP-1. This hormone is released from your small intestines in response to food and acts in several ways to improve the way your body handles glucose (sugar).
How do they stop hunger?
Liraglutide acts in several regions of the unconscious part of your brain, specifically the hypothalamus, which controls metabolism, and parts of the brain stem responsible for communicating your body’s nutrient status to the hypothalamus.
Its actions here appear to reduce hunger in two different ways. First, it helps you to feel full earlier, making smaller meals more satisfying. Second, it alters your “motivational salience” towards food, meaning it reduces the amount of food you seek out.
Liraglutide’s original formulation, designed to treat type 2 diabetes, was marketed as Victoza. Its ability to cause weight loss was evident soon after it entered the market.
Shortly after, a stronger formulation, called Saxenda, was released, which was intended for weight loss in people with obesity.
How much weight can you lose with liraglutide?
People respond differently and will lose different amounts of weight. But here, we’ll note the average weight loss users can expect. Some will lose more (sometimes much more), others will lose less, and a small proportion won’t respond.
The first GLP-1 mimicking drug was exenatide (Bayetta). It’s still available for treating type 2 diabetes, but there are currently no generics. Exenatide does provide some weight loss, but this is quite modest, typically around 3-5% of body weight.
For liraglutide, those using the drug to treat obesity will use the stronger one (Saxenda), which typically gives about 10% weight loss.
Semaglutide, with the stronger formulation called Wegovy, typically results in 15% weight loss.
The newest GLP-1 mimicking drug on the market, tirzepatide (Mounjaro for type 2 diabetes and Zepbound for weight loss), results in weight loss of around 25% of body weight.
What happens when you stop taking them?
Despite the effectiveness of these medications in helping with weight loss, they do not appear to change people’s weight set-point.
So in many cases, when people stop taking them, they experience a rebound toward their original weight.
People often regain weight when when they stop taking the drug. Mohammed_Al_Ali/Shutterstock What is the dose and how often do you need to take it?
Liraglutide (Victoza) for type 2 diabetes is exactly the same drug as Saxenda for weight loss, but Saxenda is a higher dose.
Although the target for each formulation is the same (the GLP-1 receptor), for glucose control in type 2 diabetes, liraglutide has to (mainly) reach the pancreas.
But to achieve weight loss, it has to reach parts of the brain. This means crossing the blood-brain barrier – and not all of it makes it, meaning more has to be taken.
All the current formulations of GLP-1 mimicking drug are injectables. This won’t change when liraglutide generics hit the market.
However, they differ in how frequently they need to be injected. Liraglutide is a once-daily injection, whereas semaglutide and tirzepatide are once-weekly. (That makes semaglutide and tirzepatide much more attractive, but we won’t see semaglutide as a generic until 2033.)
What are the side effects?
Because all these medicines have the same target in the body, they mostly have the same side effects.
The most common are a range of gastrointestinal upsets including nausea, vomiting, bloating, constipation and diarrhoea. These occur, in part, because these medications slow the movement of food out of the stomach, but are generally managed by increasing the dose slowly.
Recent clinical data suggests the slowing in emptying of the stomach can be problematic for some people, and may increase the risk of of food entering the lungs during operations, so it is important to let your doctor know if you are taking any of these drugs.
Because these are injectables, they can also lead to injection-site reactions.
Gastrointestinal side effects are most common. Halfpoint/Shutterstock During clinical trials, there were some reports of thyroid disease and pancreatitis (inflammation of the pancreas). However, it is not clear that these can be attributed to GLP-1 mimicking drugs.
In animals, GLP-1 mimicking drugs drugs have been found to negatively alter the growth of the embryo. There is currently no controlled clinical trial data on their use during pregnancy, but based on animal data, these medicines should not be used during pregnancy.
Who can use them?
The GLP-1 mimicking drugs for weight loss (Wegovy, Saxenda, Zepbound/Mounjaro) are approved for use by people with obesity and are meant to only be used in conjunction with diet and exercise.
These drugs must be prescribed by a doctor and for obesity are not covered by the Pharmaceutical Benefits Scheme, which is one of the reasons why they are expensive. But in time, generic versions of liraglutide are likely to be more affordable.
Sebastian Furness, ARC Future Fellow, School of Biomedical Sciences, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
5 Things To Know About Passive Suicidal Ideation
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you’ve ever wanted to go to sleep and never wake up, or have some accident/incident/illness take you with no action on your part, or a loved one has ever expressed such thoughts/feelings to you… Then this video is for you. Dr. Scott Eilers explains:
Tired of living
We’ll not keep them a mystery; here are the five things that Dr. Eilers wants us to know about passive suicidal ideation:
- What it is: a desire for something to end your life without taking active steps. While it may seem all too common, it’s not necessarily inevitable or unchangeable.
- What it means in terms of severity: it isn’t a clear indicator of how severe someone’s depression is. It doesn’t necessarily mean that the person’s depression is mild; it can be severe even without active suicidal thoughts, or indeed, suicidality at all.
- What it threatens: although passive suicidal ideation doesn’t usually involve active planning, it can still be dangerous. Over time, it can evolve into active suicidal ideation or lead to risky behaviors.
- What it isn’t: passive suicidal ideation is different from intrusive thoughts, which are unwanted, distressing thoughts about death. The former involves a desire for death, while the latter does not.
- What it doesn’t have to be: passive suicidal ideation is often a symptom of underlying depression or a mood disorder, which can be treated through therapy, medication, or a combination of both. Seeking treatment is crucial and can be life-changing.
For more on all of the above, here’s Dr. Eilers with his own words:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- The Mental Health First Aid You’ll Hopefully Never Need ← about depression generally
- How To Stay Alive (When You Really Don’t Want To) ← about suicidality specifically
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Celery vs Carrot – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing celery to carrot, we picked the carrot.
Why?
In terms of macros, carrot has more protein, carbs, and fiber, and is thus the “most food per food” option. The carb:fiber ratio is such that they have about the same glycemic index (when raw, anyway).
In the category of vitamins, celery has more of vitamins B9 and K, while carrot has more of vitamins A, B1, B2, B3, B5, B6, C, E, and choline. An easy win for carrot here.
When it comes to minerals, celery has more calcium and selenium, while carrot has more copper, iron, magnesium, manganese, phosphorus, potassium, and zinc. Another clear win for carrot.
In short, both are very respectable foods, but carrot simply has more in it, and it’s all good.
Enjoy!
Want to learn more?
You might like to read:
Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: