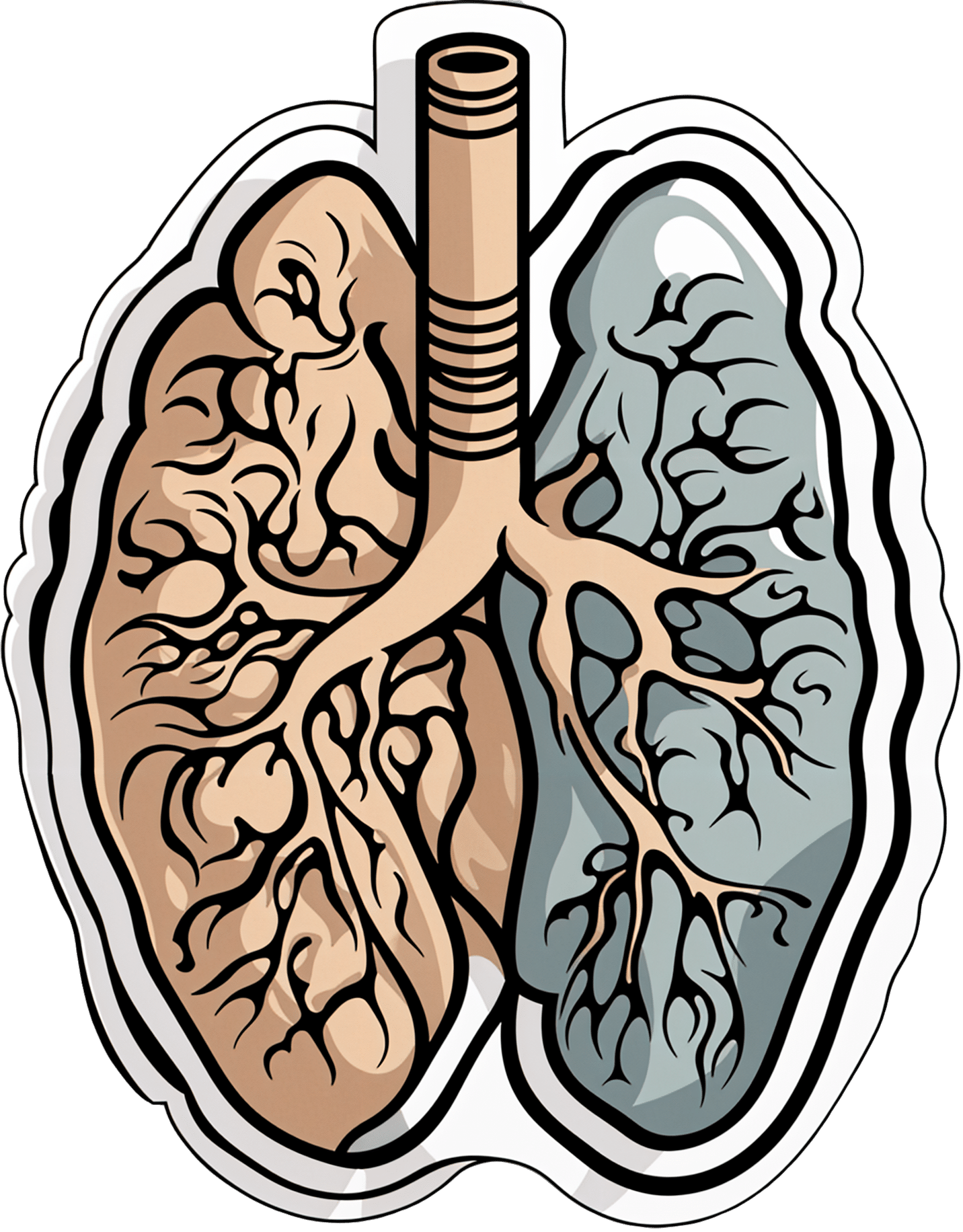
Early Detection May Help Kentucky Tamp Down Its Lung Cancer Crisis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Anthony Stumbo’s heart sank after the doctor shared his mother’s chest X-ray.
“I remember that drive home, bringing her back home, and we basically cried,” said the internal medicine physician, who had started practicing in eastern Kentucky near his childhood home shortly before his mother began feeling ill. “Nobody wants to get told they’ve got inoperable lung cancer. I cried because I knew what this meant for her.”
Now Stumbo, whose mother died the following year, in 1997, is among a group of Kentucky clinicians and researchers determined to rewrite the script for other families by promoting training and boosting awareness about early detection in the state with the highest lung cancer death rate. For the past decade, Kentucky researchers have promoted lung cancer screening, first recommended by the U.S. Preventive Services Task Force in 2013. These days the Bluegrass State screens more residents who are at high risk of developing lung cancer than any state except Massachusetts — 10.6% of eligible residents in 2022, more than double the national rate of 4.5% — according to the most recent American Lung Association analysis.
The effort has been driven by a research initiative called the Kentucky LEADS (Lung Cancer Education, Awareness, Detection, and Survivorship) Collaborative, which in 2014 launched to improve screening and prevention, to identify more tumors earlier, when survival odds are far better. The group has worked with clinicians and hospital administrators statewide to boost screening rates both in urban areas and regions far removed from academic medical centers, such as rural Appalachia. But, a decade into the program, the researchers face an ongoing challenge as they encourage more people to get tested, namely the fear and stigma that swirl around smoking and lung cancer.
Lung cancer kills more Americans than any other malignancy, and the death rates are worst in a swath of states including Kentucky and its neighbors Tennessee and West Virginia, and stretching south to Mississippi and Louisiana, according to data from the Centers for Disease Control and Prevention.
It’s a bit early to see the impact on lung cancer deaths because people may still live for years with a malignancy, LEADS researchers said. Plus, treatment improvements and other factors may also help reduce death rates along with increased screening. Still, data already shows that more cancers in Kentucky are being detected before they become advanced, and thus more difficult to treat, they said. Of total lung cancer cases statewide, the percentage of advanced cases — defined as cancers that had spread to the lymph nodes or beyond — hovered near 81% between 2000 and 2014, according to Kentucky Cancer Registry data. By 2020, that number had declined to 72%, according to the most recent data available.
“We are changing the story of families. And there is hope where there has not been hope before,” said Jennifer Knight, a LEADS principal investigator.
Older adults in their 60s and 70s can hold a particularly bleak view of their mortality odds, given what their loved ones experienced before screening became available, said Ashley Shemwell, a nurse navigator for the lung cancer screening program at Owensboro Health, a nonprofit health system that serves Kentucky and Indiana.
“A lot of them will say, ‘It doesn’t matter if I get lung cancer or not because it’s going to kill me. So I don’t want to know,’” said Shemwell. “With that generation, they saw a lot of lung cancers and a lot of deaths. And it was terrible deaths because they were stage 4 lung cancers.” But she reminds them that lung cancer is much more treatable if caught before it spreads.
The collaborative works with several partners, including the University of Kentucky, the University of Louisville, and GO2 for Lung Cancer, and has received grant funding from the Bristol Myers Squibb Foundation. Leaders have provided training and other support to 10 hospital-based screening programs, including a stipend to pay for resources such as educational materials or a nurse navigator, Knight said. In 2022, state lawmakers established a statewide lung cancer screening program based in part on the group’s work.
Jacob Sands, a lung cancer physician at Boston’s Dana-Farber Cancer Institute, credits the LEADS collaborative with encouraging patients to return for annual screening and follow-up testing for any suspicious nodules. “What the Kentucky LEADS program is doing is fantastic, and that is how you really move the needle in implementing lung screening on a larger scale,” said Sands, who isn’t affiliated with the Kentucky program and serves as a volunteer spokesperson for the American Lung Association.
In 2014, Kentucky expanded Medicaid, increasing the number of lower-income people who qualified for lung cancer screening and any related treatment. Adults 50 to 80 years old are advised to get a CT scan every year if they have accumulated at least 20 pack years and still smoke or have quit within the past 15 years, according to the latest task force recommendation, which widened the pool of eligible adults. (To calculate pack years, multiply the packs of cigarettes smoked daily by years of smoking.) The lung association offers an online quiz, called “Saved By The Scan,” to figure out likely eligibility for insurance coverage.
Half of U.S. patients aren’t diagnosed until their cancer has spread beyond the lungs and lymph nodes to elsewhere in the body. By then, the five-year survival rate is 8.2%.
But regular screening boosts those odds. When a CT scan detects lung cancer early, patients have an 81% chance of living at least 20 years, according to data published in November in the journal Radiology.
Some adults, like Lisa Ayers, didn’t realize lung cancer screening was an option. Her family doctor recommended a CT scan last year after she reported breathing difficulties. Ayers, who lives in Ohio near the Kentucky border, got screened at UK King’s Daughters, a hospital in far eastern Kentucky. The scan didn’t take much time, and she didn’t have to undress, the 57-year-old said. “It took me longer to park,” she quipped.
She was diagnosed with a lung carcinoid tumor, a type of neuroendocrine cancer that can grow in various parts of the body. Her cancer was considered too risky for surgery, Ayers said. A biopsy showed the cancer was slow-growing, and her doctors said they would monitor it closely.
Ayers, a lifelong smoker, recalled her doctor said that her type of cancer isn’t typically linked to smoking. But she quit anyway, feeling like she’d been given a second chance to avoid developing a smoking-related cancer. “It was a big wake-up call for me.”
Adults with a smoking history often report being treated poorly by medical professionals, said Jamie Studts, a health psychologist and a LEADS principal investigator, who has been involved with the research from the start. The goal is to avoid stigmatizing people and instead to build rapport, meeting them where they are that day, he said.
“If someone tells us that they’re not ready to quit smoking but they want to have lung cancer screening, awesome; we’d love to help,” Studts said. “You know what? You actually develop a relationship with an individual by accepting, ‘No.’”
Nationally, screening rates vary widely. Massachusetts reaches 11.9% of eligible residents, while California ranks last, screening just 0.7%, according to the lung association analysis.
That data likely doesn’t capture all California screenings, as it may not include CT scans done through large managed care organizations, said Raquel Arias, a Los Angeles-based associate director of state partnerships at the American Cancer Society. She cited other 2022 data for California, looking at lung cancer screening for eligible Medicare fee-for-service patients, which found a screening rate of 1%-2% in that population.
But, Arias said, the state’s effort is “nowhere near what it needs to be.”
The low smoking rate in California, along with its image as a healthy state, “seems to have come with the unintended consequence of further stigmatizing people who smoke,” said Arias, citing one of the findings from a 2022 report looking at lung cancer screening barriers. For instance, eligible patients may be reluctant to share prior smoking habits with their health provider, she said.
Meanwhile, Kentucky screening efforts progress, scan by scan.
At Appalachian Regional Healthcare, 3,071 patients were screened in 2023, compared with 372 in 2017. “We’re just scratching the surface of the potential lives that we can have an effect on,” said Stumbo, a lung cancer screening champion at the health system, which includes 14 hospitals, most located in eastern Kentucky.
The doctor hasn’t shed his own grief about what his family missed after his mother died at age 51, long before annual screening was recommended. “Knowing that my children were born, and never knowing their grandmother,” he said, “just how sad is that?”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Kitchen Prescription – by Saliha Mahmood Ahmed
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One of the biggest challenges facing anyone learning to cook more healthily, is keeping it tasty. What to cook when your biggest comfort foods all contain things you “should” avoid?
Happily for us, Dr. Ahmed is here with a focus on comfort food that’s good for your gut health. It’s incidentally equally good for the heart and good against diabetes… but Dr. Ahmed is a gastroenterologist, so that’s where she’s coming from with these.
There’s a wide range of 101 recipes here, including many tagged vegetarian, vegan, and/or gluten-free, as appropriate.
While this is not a vegetarian cookbook, Dr. Ahmed does consider the key components of a good diet to be, in order of quantity that should be consumed:
- Fruits and vegetables
- Whole grains
- Legumes
- Pulses
- Nuts and seeds
…and as such, the recipes are mostly plant-based.
The recipes are from all around the world, and/but the ingredients are mostly things that are almost universal. In the event that something might be hard-to-get, she suggests an appropriate substitution.
The recipes are straightforward and clear, as well as being beautifully illustrated.
All in all, a fine addition to anyone’s kitchen!
Get your copy of The Kitchen Prescription from Amazon today!
Share This Post
-
Functional Exercise For Seniors – by James Atkinson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of exercises books are tailored to 20-year-old athletes training for their first Tough Mudder. Others, that the only thing standing between us and a perfect Retroflex Countersupine Divine Pretzel position is a professionally-lit Instagrammable photo.
This one’s not like that.
But! Nor does it think being over a certain age is a reason to not have genuinely robust health, of the kind that may make some younger people envious. So, it lays out, in progressive format, guidelines for exercises targeted at everything we need to build and maintain as we get older.
The writing style is clear, and the illustrations too (the cover art is the same style as the illustrations inside).
Bottom line: if you’re looking for a workout guide that understands you are nearer 80 than 18, and/but also doesn’t assume your age limits your exercise potential to “wrist exercises in chair”, then this book is a fine pick.
Share This Post
-
When Carbs, Proteins, & Fats Switch Metabolic Roles
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Strange Things Happening In The Islets Of Langerhans
It is generally known and widely accepted that carbs have the biggest effect on blood sugar levels (and thus insulin response), fats less so, and protein least of all.
And yet, there was a groundbreaking study published yesterday which found:
❝Glucose is the well-known driver of insulin, but we were surprised to see such high variability, with some individuals showing a strong response to proteins, and others to fats, which had never been characterized before.
Insulin plays a major role in human health, in everything from diabetes, where it is too low*, to obesity, weight gain and even some forms of cancer, where it is too high.
These findings lay the groundwork for personalized nutrition that could transform how we treat and manage a range of conditions.❞
*saying ”too low” here is potentially misleading without clarification; yes, Type 1 Diabetics will have too little [endogenous] insulin (because the pancreas is at war with itself and thus isn’t producing useful quantities of insulin, if any). Type 2, however, is more a case of acquired insulin insensitivity, because of having too much at once too often, thus the body stops listening to it, “boy who cried wolf”-style, and the pancreas also starts to get fatigued from producing so much insulin that’s often getting ignored, and does eventually produce less and less while needing more and more insulin to get the same response, so it can be legitimately said “there’s not enough”, but that’s more of a subjective outcome than an objective cause.
Back to the study itself, though…
What they found, and how they found it
Researchers took pancreatic islets from 140 heterogenous donors (varied in age and sex; ostensibly mostly non-diabetic donors, but they acknowledge type 2 diabetes could potentially have gone undiagnosed in some donors*) and tested cell cultures from each with various carbs, proteins, and fats.
They found the expected results in most of the cases, but around 9% responded more strongly to the fats than the carbs (even more strongly than to glucose specifically), and even more surprisingly 8% responded more strongly to the proteins.
*there were also some known type 2 diabetics amongst the donors; as expected, those had a poor insulin response to glucose, but their insulin response to proteins and fats were largely unaffected.
What this means
While this is, in essence, a pilot study (the researchers called for larger and more varied studies, as well as in vivo human studies), the implications so far are important:
It appears that, for a minority of people, a lot of (generally considered very good) antidiabetic advice may not be working in the way previously understood. They’re going to (for example) put fat on their carbs to reduce the blood sugar spike, which will technically still work, but the insulin response is going to be briefly spiked anyway, because of the fats, which very insulin response is what will lower the blood sugars.
In practical terms, there’s not a lot we can do about this at home just yet—even continuous glucose monitors won’t tell us precisely, because they’re monitoring glucose, not the insulin response. We could probably measure everything and do some math and work out what our insulin response has been like based on the pace of change in blood sugar levels (which won’t decrease without insulin to allow such), but even that is at best grounds for a hypothesis for now.
Hopefully, more publicly-available tests will be developed soon, enabling us all to know our “insulin response type” per the proteome predictors discovered in this study, rather than having to just blindly bet on it being “normal”.
Ironically, this very response may have hidden itself for a while—if taking fats raised insulin response without raising blood sugar levels, then if blood sugar levels are the only thing being measured, all we’ll see is “took fats at dinner; blood sugars returned to normal more quickly than when taking carbs without fats”.
You can read the study in full here:
Proteomic predictors of individualized nutrient-specific insulin secretion in health and disease
Want to know more about blood sugar management?
You might like to catch up on:
- 10 Ways To Balance Your Blood Sugars
- Track Your Blood Sugars For Better Personalized Health
- How To Turn Back The Clock On Insulin Resistance
Take care!
Share This Post
Related Posts
-
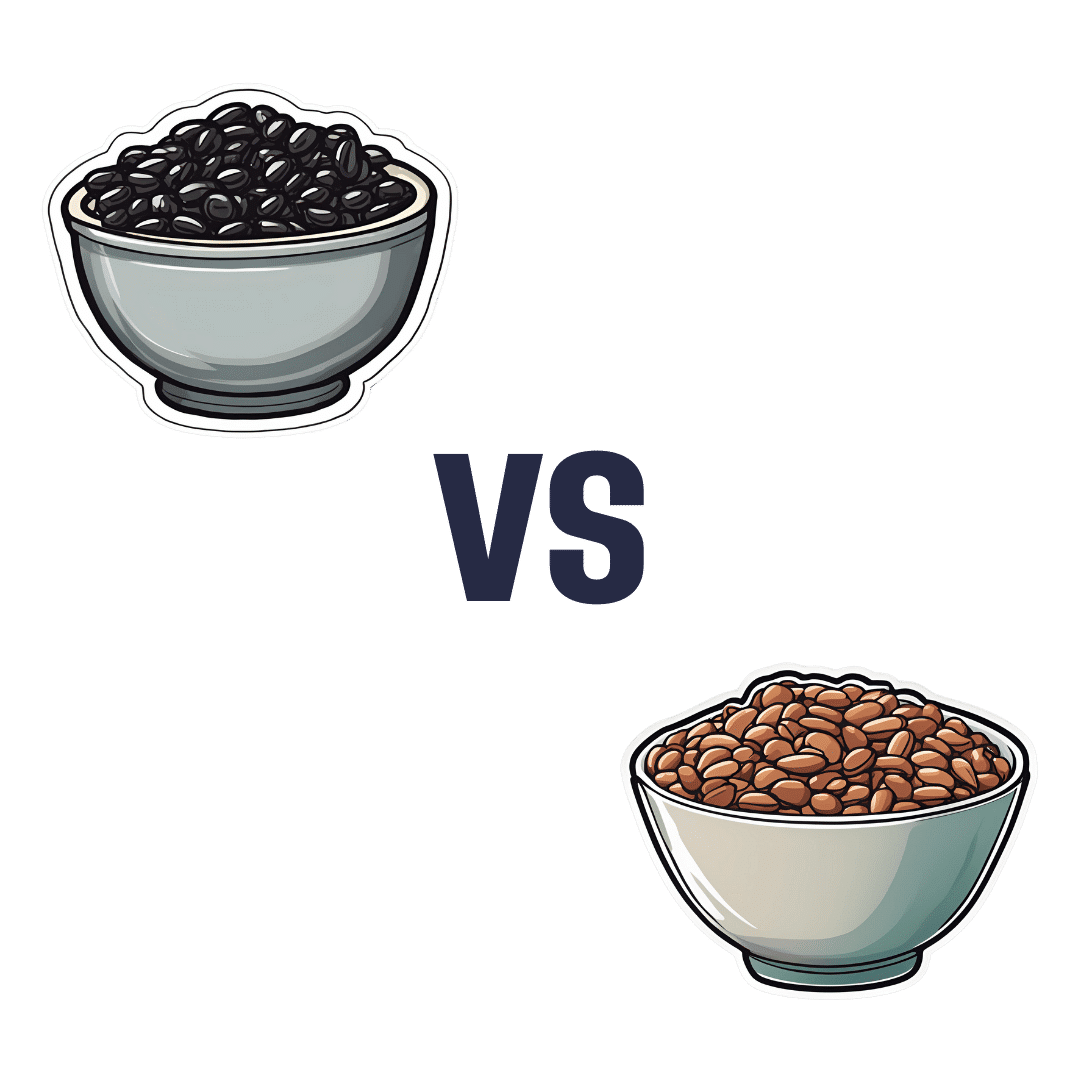
Black Beans vs Pinto Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing black beans to pinto beans, we picked the pinto beans.
Why?
Both of these beans have won all their previous comparisons, so it’s no surprise that this one was very close. Despite their different appearance, taste, and texture, their nutritional profiles are almost identical:
In terms of macros, pinto beans have a tiny bit more protein, carbs, and fiber. So, a nominal win for pinto beans, but again, the difference is very slight.
When it comes to vitamins, black beans have more of vitamins A, B1, B3, and B5, while pinto beans have more of vitamins B2, B6, B9, C, E, K and choline. Superficially, again this is nominally a win for pinto beans, but in most cases the differences are so slight as to be potentially the product of decimal place rounding.
In the category of minerals, black beans have more calcium, copper, iron, and phosphorus, while pinto beans have more magnesium, manganese, selenium, and zinc. That’s a 4:4 tie, but the only one with a meaningful margin of difference is selenium (of which pinto beans have 4x more), so we’re calling this one a very modest win for pinto beans.
All in all, adding these up makes for a “if we really are pressed to choose” win for pinto beans, but honestly, enjoy either in accordance with your preference (this writer prefers black beans!), or better yet, both.
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
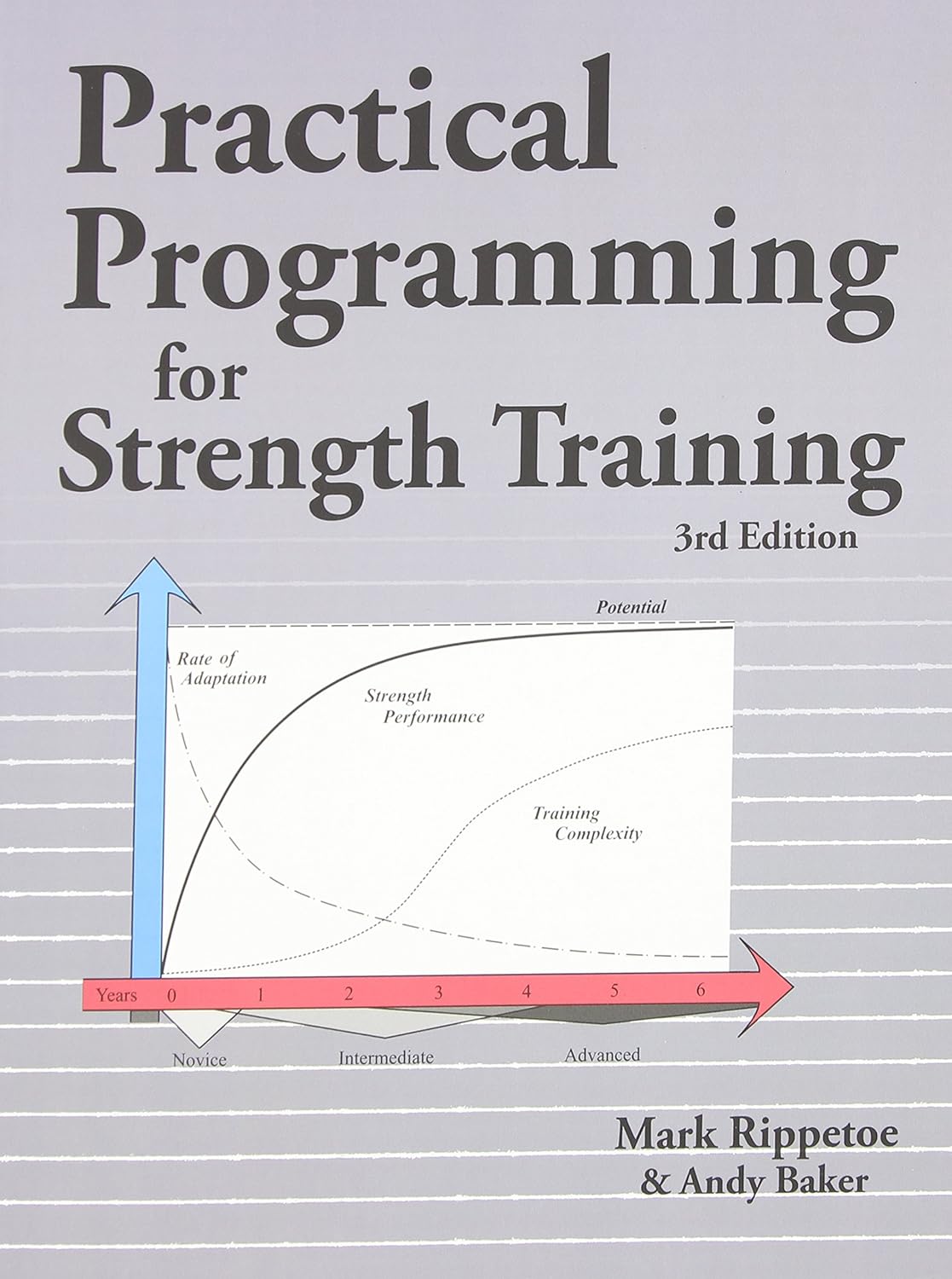
Practical Programming for Strength Training – by Mark Rippetoe & Andy Baker
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Strength training is an important part of overall health maintenance, but it can be hard to find a good guide to progressive strength improvement that isn’t a bodybuilding book.
This one gives a ground-upwards approach, explaining small details to even quite basic things, before taking the reader through to more advanced progressions, and how to get the most strength-building out of each exercise over time.
As such, this is a good book for anyone of any level from beginner to quite experienced, and you can hop in at any point since there are always catch-up summaries and/or reiterations of the previous concepts that we’re now building on from.
The authors do also talk nutrition, hormones, and so forth, but most of it is about the exercises and the progressions thereof.
There is a slightly patronizing chapter towards the end, about “special populations”, for example offering “novice and intermediate training for women”, but it doesn’t take away from the majority of the book, as the exercises don’t care about your gender. Muscles are muscles, and we all start from wherever we are. Yes, testosterone boosts muscle mass, but let’s face it, there are a lot of women in the world who are stronger than a lot of men.
One thing to bear in mind is that a lot of this is barbell training, so you will need a barbell (or access to one at a gym). If purely bodyweight training is your preference, or perhaps some other form of weightlifting (e.g. kettlebells or such) then this isn’t the book for that.
Bottom line: if strength training is your focus and you like barbells, then this is a great book to take you quite a way along that road.
Click here to check out Practical Programming For Strength Training, and get stronger!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
One More Resource Against Osteoporosis!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Your Bones Were Made For Moving Too!
We know that to look after bone health, resistance training is generally what’s indicated. Indeed, we mentioned it yesterday, and we’ve talked about it before:
Resistance Is Useful! (Especially As We Get Older)
We also know that if you have osteoporosis already, some exercises are a better or worse idea than others:
Osteoporosis & Exercises: Which To Do (And Which To Avoid)
However! New research suggests that also getting in your recommended 150 minutes per week of moderate exercise slows bone density loss.
The study by Dr. Tiina Savikangas et al. looked at 299 people in their 70s (just over half being women) and found that, over the course of a year, bone mineral density loss was inversely correlated with moderate exercise as recorded by an accelerometer (as found in most fitness-tracking wearables and smartphones).
In other words: those who got more minutes of exercise, kept more bone mineral density.
As well as monitoring bone mineral density, the study also looked at cross-sectional area, but that remained stable throughout.
As for how much is needed:
❝Even short bursts of activity can be significant for the skeleton, so we also looked at movement in terms of the number and intensity of individual impacts. For example, walking and running cause impacts of different intensities.
We found that impacts that were comparable to at least brisk walking were associated with better preservation of bone mineral density.❞
Read more: Impacts during everyday physical activity can slow bone loss ← pop-science source, interviewing the lead researcher
On which note, we’ve a small bone to pick…
As a small correction, the pop-science source says that the subjects’ ages ranged from 70 to 85 years; the paper, meanwhile, clearly shows that the age-range was 74.4±3.9 years (shown in the “Results” table), rounded to 74.4 ± 4 years, in the abstract. So, certainly no participant was older than 78 years and four months.
Why this matters: the age range itself may be critical or it might not, but what is important is that this highlights how we shouldn’t just believe figures cited in pop-science articles, and it’s always good to click through to the source!
This paper is a particularly fascinating read if you have time, because—unlike a lot of studies—they really took great care to note what exactly can and cannot be inferred from the data, and how and why.
Especially noteworthy was the diligence with which they either controlled for, or recognized that they could not control for, far more variables than most studies even bother to mention.
This kind of transparency is critical for good science, and we’d love to see more of it!
Want to apply this to your life?
Tracking minutes-of-movement is one of the things that fitness trackers are best at, so connect your favourite app (one of these days we’ll do a fitness tracker comparison article) and get moving!
And as for the other things that fitness trackers do? As it turns out, they do have their strengths and weaknesses, which are good to bear in mind:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: