Longans vs Lychees – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing longans to lychees, we picked the lychees.
Why?
These two fruits are more closely related than they look from the outside, both being members of the soapberry family. However, there are some differences:
In terms of macros, longans have more protein while lychees have more carbs, and they are equal on fiber, giving longans the lower glycemic index. They’re both good, but longans nominally take the win on this one.
When it comes to vitamins, longans have more of vitamins B1, B2, and C, while lychees have more of vitamins B3, B6, B9, E, K, and choline, making for a respectable win for lychees in this category.
In the category of minerals, longans have more copper and potassium, while lychees have more calcium, iron, manganese phosphorus, and zinc. Thus, a win for lychees here too.
It’s worth looking at polyphenols too—lychees have around 10x more, which is notable.
Adding up the categories makes for an overall win for lychees, but by all means enjoy either or both! Diversity is good.
Want to learn more?
You might like to read:
Replacing Sugar: Top 10 Anti-Inflammatory Sweet Foods ← longans and lychees both make the list
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Women Rowing North – by Dr. Mary Pipher
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ageism is rife, as is misogyny. And those can be internalized too, and compounded as they intersect.
Clinical psychologist Dr. Mary Pipher, herself 75, writes for us a guidebook of, as the subtitle goes, “navigating life’s currents and flourishing as we age”.
The book does assume, by the way, that the reader is…
- a woman, and
- getting old (if not already old)
However, the lessons the book imparts are vital for women of any age, and valuable as a matter of insight and perspective for any reader.
Dr. Pipher takes us on a tour of aging as a woman, and what parts of it we can make our own, do things our way, and take what joy we can from it.
Nor is the book given to “toxic positivity” though—it also deals with themes of hardship, frustration, and loss.
When it comes to those elements, the book is… honest, human, and raw. But also, an exhortation to hope, beauty, and a carpe diem attitude.
Bottom line: this book is highly recommendable to anyone of any age; life is precious and can be short. And be we blessed with many long years, this book serves as a guide to making each one of them count.
Click here to check out Women Rowing North—it really is worth it
Share This Post
-
9 Reasons To Avoid Mobility Training
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Why might someone not want to do mobility training? Here are some important reasons:
Make an informed choice
Here’s Liv’s hit-list of reasons to skip mobility training:
- Poor Circulation: Avoid mobility training if you don’t want to improve or maintain good blood circulation, which aids muscle recovery and reduces soreness.
- Low Energy Levels: Mobility training increases oxygen flow to the brain and muscles, boosting energy. Skip it if you prefer feeling sluggish!
- Digestive Health: Stretches that rotate the torso aid digestion and relieve bloating. Definitely best to avoid it if you’re uninterested in improving digestive health.
- Joint Health: Mobility work stimulates synovial fluid production, reducing joint friction and promoting longevity. You can skip it if you don’t care about comfortable movement.
- Sleep Quality: Gentle stretching triggers relaxation, aiding restful sleep. Avoid it if you enjoy restless nights!
- Pain Tolerance: Stretching trains the nervous system to handle discomfort better. Skip it if you prefer suffering 🙂
- Headache Reduction: Mobility work relieves tension in the neck and shoulders, reducing the occurrence and severity of headaches. No need to do it if you’re fine with frequent headaches.
- Immune System Support: Mobility training boosts lymphatic circulation, aiding the immune system. Avoid it if you prefer your immune system to get exciting in a bad way.
- Stress Reduction: Mobility exercises release endorphins and lower cortisol levels, reducing stress. So, it is certainly best to skip it if you prefer feeling stressed and enjoy the many harmful symptoms of high cortisol levels!
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Mobility As Though A Sporting Pursuit: Train For The Event Of Your Life!
Take care!
Share This Post
-
The Food Additive You Do Want
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Q: When Is A Fiber Not A Fiber?
A: when it’s a resistant starch. What’s it resistant to? Digestion. So, it functions as though a fiber, and by some systems, may get classified as such.
It’s a little like how sucralose is technically a sugar, but the body processes it like a fiber (but beware, because the sweetness of this disaccharide alone can trigger an insulin response anyway—dose dependent)
There may be other problems too:
But today’s not about sucralose, it’s about…
Guar gum’s surprising dietary role
You may have noticed “guar gum” on the list of ingredients of all kinds of things from baked goods to dairy products to condiments to confectionary and more.
It’s also used in cosmetics and explosives, but let’s not focus on that.
It’s used in food products as…
- a bulking agent
- a thickener
- a stabilizer
Our attention was caught by a new study, that found:
Resistant starch intake facilitates weight loss in humans by reshaping the gut microbiota
Often people think of “fiber helps weight loss” as “well yes, if you are bulking out your food with sawdust, you will eat less”, but it’s not that.
There’s an actual physiological process going on here!
We can’t digest it, but our gut microbiota can and will ferment it. See also:
Fiber against pounds: Resistant starch found to support weight loss
Beyond weight loss
Not everyone wants to lose weight, and even where weight loss is a goal, it’s usually not the only goal. As it turns out, adding guar gum into our diet does more things too:
Resistant starch supplement found to reduce liver triglycerides in people with fatty liver disease
(specifically, this was about NAFLD, non-alcoholic fatty liver disease)
Digging a little, it seems the benefits don’t stop there either:
Diet high in guar gum fiber limits inflammation and delays multiple sclerosis symptoms
(this one was a rodent study, but still, it’s promising and it’s consistent with what one would expect based on what else we know about its function in diet)
Should we just eat foods with guar gum in as an additive?
That depends on what they are, but watch out for the other additives if you do!
You can just buy guar gum by itself, by the way (here’s an example product on Amazon).
It’s doubtlessly no fun to take as a supplement (we haven’t tried this one), but it can be baked into bread, if baking’s your thing, or just used as a thickener in recipes where ordinarily you might use cornstarch or something else.
Can I get similar benefits from other foods?
The relevant quality is also present in resistant starches in general, so you might want to check out these foods, for example:
9 Foods That Are High in Resistant Starch
You can also check out ways to increase your fiber intake in general:
Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
Enjoy!
Share This Post
Related Posts
-
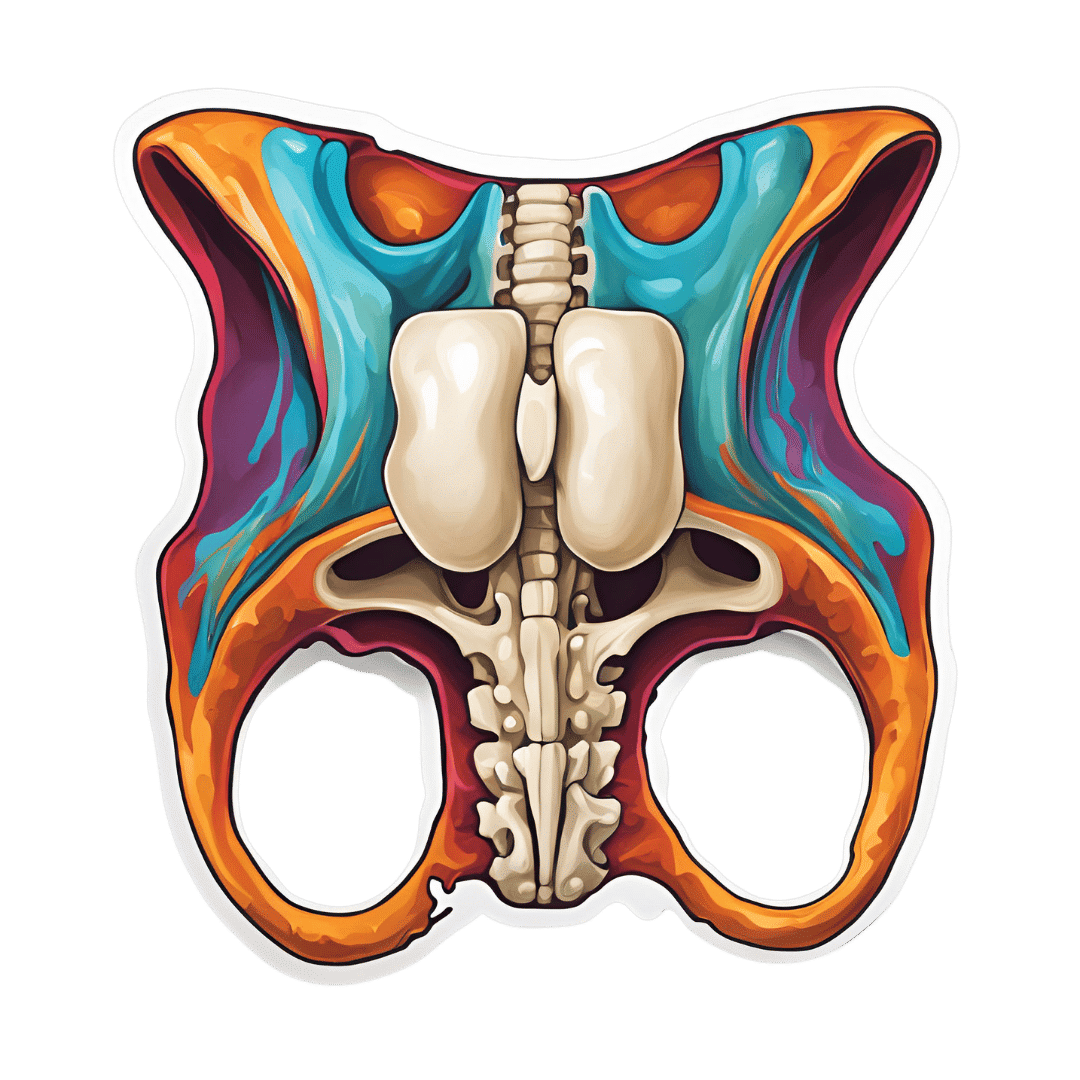
Overcome Front-Of-Hip Pain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Alyssa Kuhn, physiotherapist, demonstrates how:
One, two, three…
One kind of pain affects a lot of related things: hip pain has an impact on everything that’s connected to the pelvis, which is basically the rest of the body, but especially the spine itself. For this reason, it’s critical to keep it in as good condition as possible.
Two primary causes of hip stiffness and pain:
- Anterior pelvic tilt due to posture, weight distribution, or pain. This tightens the front muscles and weakens the back muscles.
- Prolonged sitting, which tightens the hip muscles due to inactivity.
Three exercises are recommended by Dr. Kuhn to relieve pain and stiffness:
- Bridge exercise:
- Lie on a firm surface with your knees bent.
- Push through your feet, engage your hamstrings, and flatten your lower back.
- Hold for 3–5 seconds, relax, and repeat (10–20 reps).
- Wall exercise with arms:
- Stand with your lower back against the wall, feet a step away.
- Tilt your hips backwards, keeping your lower back in contact with the wall.
- Alternate lifting one arm at a time while maintaining back contact with the wall (10–20 reps).
- Wall exercise with legs:
- Same stance as the previous exercise but wider now.
- Lift one heel at a time while keeping your hips stable and your back against the wall.
- Practice for 30–60 seconds, maintaining good form.
As ever, consistency is key for long-term relief. Dr. Kuhn recommends doing these regularly, especially before any expected periods of prolonged sitting (e.g. at desk, or driving, etc). And of course, do try to reduce, or at least break up, those sitting marathons if you can.
For more on all of this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Saunas: Health Benefits (& Caveats)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Heat Is On
In Tuesday’s newsletter, we asked you your (health-related) opinion on saunas, and got the above-depicted, below-described, set of responses:
- About 53% said it is “a healthful activity with many benefits”
- About 25% said it is “best avoided; I feel like I’m dying in there”
- About 12% said “it feels good and therefore can’t be all bad”
So what does the science say?
The heat of saunas carries a health risk: True or False?
False, generally speaking, for any practical purposes. Of course, anything in life comes with a health risk, but statistically speaking, your shower at home is a lot more dangerous than a sauna (risk of slipping with no help at hand).
It took a bit of effort to find a paper on the health risks of saunas, because all the papers on PubMed etc coming up for those keywords were initially papers with “reduces the risk of…”, i.e. ways in which the sauna is healthy.
However, we did find one:
❝Contraindications to sauna bathing include unstable angina pectoris, recent myocardial infarction, and severe aortic stenosis.
Sauna bathing is safe, however, for most people with coronary heart disease with stable angina pectoris or old myocardial infarction.
Very few acute myocardial infarctions and sudden deaths occur in saunas, but alcohol consumption during sauna bathing increases the risk of hypotension, arrhythmia, and sudden death, and should be avoided. ❞
~ Dr. Matti Hannuksela & Dr. Samer Ellahham
Source: Benefits and risks of sauna bathing
So, very safe for most people, safe even for most people with heart disease, but there are exceptions so check with your own doctor of course.
And drinking alcohol anywhere is bad for the health, but in a sauna it’s a truly terrible idea. As an aside, please don’t drink alcohol in the shower, either (risk of slipping with no help at hand, and this time, broken glass too).
On the topic of it being safe for most people’s hearts, see also:
Beneficial effects of sauna bathing for heart failure patients
As an additional note, those who have a particular sensitivity to the heat, may (again please check with your own doctor, as your case may vary) actually benefit from moderate sauna use, to reduce the cardiovascular strain that your body experiences during heatwaves (remember, you can get out of a sauna more easily than you can get out of a heatwave, so for many people it’s a lot easier to do moderation and improve thermoregulatory responses):
Sauna usage can bring many health benefits: True or False?
True! Again, at least for most people. As well as the above-discussed items, here’s one for mortality rates in healthy Finnish men:
Not only that, also…
❝The Finnish saunas have the most consistent and robust evidence regarding health benefits and they have been shown to decrease the risk of health outcomes such as hypertension, cardiovascular disease, thromboembolism, dementia, and respiratory conditions; may improve the severity of musculoskeletal disorders, COVID-19, headache and flu, while also improving mental well-being, sleep, and longevity.
Finnish saunas may also augment the beneficial effects of other protective lifestyle factors such as physical activity.
The beneficial effects of passive heat therapies may be linked to their anti-inflammatory, cytoprotective and anti-oxidant properties and synergistic effects on neuroendocrine, circulatory, cardiovascular and immune function.
Passive heat therapies, notably Finnish saunas, are emerging as potentially powerful and holistic strategies to promoting health and extending the healthspan in all populations. ❞
~ Dr. Jari Laukkanen & Dr. Setor Kunutsor
(the repeated clarification of “Finnish sauna” is not a matter of fervent nationalism, by the way, but rather a matter of disambiguating it from Swedish sauna, which has some differences, most notably a lack of steam)
That reminds us: in Scandinavia, it is usual to use a sauna naked, and in Finland in particular, it is a common social activity amongst friends, coworkers, etc. In the US, many people are not so comfortable with nudity, and indeed, many places that provide saunas, may require the wearing of swimwear. But…
Just one problem: if you’re wearing swimwear because you’ve just been swimming in a pool, you now have chlorinated water soaked into your swimwear, which in the sauna, will become steam + chlorine gas. That’s not so good for your health (and is one reason, beyond tradition and simple normalization, for why swimwear is usually not permitted in Finnish saunas).
Want to read more?
You might like our previous main feature,
Turning Up The Heat Against Diabetes & Alzheimer’s ← you guessed it, sauna may be beneficial against these too
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is alcohol good or bad for you? Yes.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This article originally appeared in Harvard Public Health magazine.
It’s hard to escape the message these days that every sip of wine, every swig of beer is bad for your health. The truth, however, is far more nuanced.
We have been researching the health effects of alcohol for a combined 60 years. Our work, and that of others, has shown that even modest alcohol consumption likely raises the risk for certain diseases, such as breast and esophageal cancer. And heavy drinking is unequivocally harmful to health. But after countless studies, the data do not justify sweeping statements about the effects of moderate alcohol consumption on human health.
Yet we continue to see reductive narratives, in the media and even in science journals, that alcohol in any amount is dangerous. Earlier this month, for instance, the media reported on a new study that found even small amounts of alcohol might be harmful. But the stories failed to give enough context or probe deeply enough to understand the study’s limitations—including that it cherry-picked subgroups of a larger study previously used by researchers, including one of us, who concluded that limited drinking in a recommended pattern correlated with lower mortality risk.
“We need more high-quality evidence to assess the health impacts of moderate alcohol consumption. And we need the media to treat the subject with the nuance it requires. Newer studies are not necessarily better than older research.”
Those who try to correct this simplistic view are disparaged as pawns of the industry, even when no financial conflicts of interest exist. Meanwhile, some authors of studies suggesting alcohol is unhealthy have received money from anti-alcohol organizations.
We believe it’s worth trying, again, to set the record straight. We need more high-quality evidence to assess the health impacts of moderate alcohol consumption. And we need the media to treat the subject with the nuance it requires. Newer studies are not necessarily better than older research.
It’s important to keep in mind that alcohol affects many body systems—not just the liver and the brain, as many people imagine. That means how alcohol affects health is not a single question but the sum of many individual questions: How does it affect the heart? The immune system? The gut? The bones?
As an example, a highly cited study of one million women in the United Kingdom found that moderate alcohol consumption—calculated as no more than one drink a day for a woman—increased overall cancer rates. That was an important finding. But the increase was driven nearly entirely by breast cancer. The same study showed that greater alcohol consumption was associated with lower rates of thyroid cancer, non-Hodgkin lymphoma, and renal cell carcinoma. That doesn’t mean drinking a lot of alcohol is good for you—but it does suggest that the science around alcohol and health is complex.
One major challenge in this field is the lack of large, long-term, high-quality studies. Moderate alcohol consumption has been studied in dozens of randomized controlled trials, but those trials have never tracked more than about 200 people for more than two years. Longer and larger experimental trials have been used to test full diets, like the Mediterranean diet, and are routinely conducted to test new pharmaceuticals (or new uses for existing medications), but they’ve never been done to analyze alcohol consumption.
Instead, much alcohol research is observational, meaning it follows large groups of drinkers and abstainers over time. But observational studies cannot prove cause-and-effect because moderate drinkers differ in many ways from non-drinkers and heavy drinkers—in diet, exercise, and smoking habits, for instance. Observational studies can still yield useful information, but they also require researchers to gather data about when and how the alcohol is consumed, since alcohol’s effect on health depends heavily on drinking patterns.
For example, in an analysis of over 300,000 drinkers in the U.K., one of us found that the same total amount of alcohol appeared to increase the chances of dying prematurely if consumed on fewer occasions during the week and outside of meals, but to decrease mortality if spaced out across the week and consumed with meals. Such nuance is rarely captured in broader conversations about alcohol research—or even in observational studies, as researchers don’t always ask about drinking patterns, focusing instead on total consumption. To get a clearer picture of the health effects of alcohol, researchers and journalists must be far more attuned to the nuances of this highly complex issue.
One way to improve our collective understanding of the issue is to look at both observational and experimental data together whenever possible. When the data from both types of studies point in the same direction, we can have more confidence in the conclusion. For example, randomized controlled trials show that alcohol consumption raises levels of sex steroid hormones in the blood. Observational trials suggest that alcohol consumption also raises the risk of specific subtypes of breast cancer that respond to these hormones. Together, that evidence is highly persuasive that alcohol increases the chances of breast cancer.
Similarly, in randomized trials, alcohol consumption lowers average blood sugar levels. In observational trials, it also appears to lower the risk of diabetes. Again, that evidence is persuasive in combination.
As these examples illustrate, drinking alcohol may raise the risk of some conditions but not others. What does that mean for individuals? Patients should work with their clinicians to understand their personal risks and make informed decisions about drinking.
Medicine and public health would benefit greatly if better data were available to offer more conclusive guidance about alcohol. But that would require a major investment. Large, long-term, gold-standard studies are expensive. To date, federal agencies like the National Institutes of Health have shown no interest in exclusively funding these studies on alcohol.
Alcohol manufacturers have previously expressed some willingness to finance the studies—similar to the way pharmaceutical companies finance most drug testing—but that has often led to criticism. This happened to us, even though external experts found our proposal scientifically sound. In 2018, the National Institutes of Health ended our trial to study the health effects of alcohol. The NIH found that officials at one of its institutes had solicited funding from alcohol manufacturers, violating federal policy.
It’s tempting to assume that because heavy alcohol consumption is very bad, lesser amounts must be at least a little bad. But the science isn’t there, in part because critics of the alcohol industry have deliberately engineered a state of ignorance. They have preemptively discredited any research, even indirectly, by the alcohol industry—even though medicine relies on industry financing to support the large, gold-standard studies that provide conclusive data about drugs and devices that hundreds of millions of Americans take or use daily.
Scientific evidence about drinking alcohol goes back nearly 100 years—and includes plenty of variability in alcohol’s health effects. In the 1980s and 1990s, for instance, alcohol in moderation, and especially red wine, was touted as healthful. Now the pendulum has swung so far in the opposite direction that contemporary narratives suggest every ounce of alcohol is dangerous. Until gold-standard experiments are performed, we won’t truly know. In the meantime, we must acknowledge the complexity of existing evidence—and take care not to reduce it to a single, misleading conclusion.
This article first appeared on The Journalist’s Resource and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: