Long COVID is real—here’s how patients can get treatment and support
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What you need to know
- There is still no single, FDA-approved treatment for long COVID, but doctors can help patients manage individual symptoms.
- Long COVID patients may be eligible for government benefits that can ease financial burdens.
- Getting reinfected with COVID-19 can worsen existing long COVID symptoms, but patients can take steps to stay protected.
On March 15—Long COVID Awareness Day—patients shared their stories and demanded more funding for long COVID research. Nearly one in five U.S. adults who contract COVID-19 suffer from long COVID, and up to 5.8 million children have the disease.
Anyone who contracts COVID-19 is at risk of developing long-term illness. Long COVID has been deemed by some a “mass-disabling event,” as its symptoms can significantly disrupt patients’ lives.
Fortunately, there’s hope. New treatment options are in development, and there are resources available that may ease the physical, mental, and financial burdens that long COVID patients face.
Read on to learn more about resources for long COVID patients and how you can support the long COVID patients in your life.
What is long COVID, and who is at risk?
Long COVID is a cluster of symptoms that can occur after a COVID-19 infection and last for weeks, months, or years, potentially affecting almost every organ. Symptoms range from mild to debilitating and may include fatigue, chest pain, brain fog, dizziness, abdominal pain, joint pain, and changes in taste or smell.
Anyone who gets infected with COVID-19 is at risk of developing long COVID, but some groups are at greater risk, including unvaccinated people, women, people over 40, and people who face health inequities.
What types of support are available for long COVID patients?
Currently, there is still no single, FDA-approved treatment for long COVID, but doctors can help patients manage individual symptoms. Some options for long COVID treatment include therapies to improve lung function and retrain your sense of smell, as well as medications for pain and blood pressure regulation. Staying up to date on COVID-19 vaccines may also improve symptoms and reduce inflammation.
Long COVID patients are eligible for disability benefits under the Americans with Disabilities Act. The Pandemic Legal Assistance Network provides pro bono support for long COVID patients applying for these benefits.
Long COVID patients may also be eligible for other forms of government assistance, such as Supplemental Nutrition Assistance Program (SNAP), Temporary Assistance for Needy Families (TANF), Medicaid, and rental and utility assistance programs.
How can friends and family of long COVID patients provide support?
Getting reinfected with COVID-19 can worsen existing long COVID symptoms. Wearing a high-quality, well-fitting mask will reduce your risk of contracting COVID-19 and spreading it to long COVID patients and others. At indoor gatherings, improving ventilation by opening doors and windows, using high-efficiency particulate air (HEPA) filters, and building your own Corsi-Rosenthal box can also reduce the spread of the COVID-19 virus.
Long COVID patients may also benefit from emotional and financial support as they manage symptoms, navigate barriers to treatment, and go through the months-long process of applying for and receiving disability benefits.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Eye Exercises That Measurably Improve Your Vision
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our eyesight, like most of the rest of our body’s functions, will decline if not adequately maintained. Modern lifestyles see most of us indoors for most of the day (which means a reduced maximum focal length) and often looking at screens (even further reduced focal length), which means that part of our eyes responsible for focus will tend to atrophy and wither. And if we want to see something better, we adjust the settings instead of adjusting our eyes. However, it is perfectly possible to recover our clear youthful vision:
See the results for yourself (and see them clearly!)
The exercises that gave him the results he showed between the two tests, are:
- Blink for 30 seconds
- Focus on something in front and (keeping your focus on that stationary point) move your head left & right, upwards & downwards, and diagonally
- Take a break and blink for 30 seconds
- Keep your head still while you move your eyes left & right, upwards & downwards, and diagonally
- Focus on something in front while you move move your head left & right, upwards & downwards, and diagonally
This should temporarily improve your vision immediately, because of what has been going on in the capillaries in and around your eyes, but sustained results require sustained (i.e. daily) practice. This is because the vasculature is only part of the mechanism; it’s also a matter of improving the muscles responsible for focusing the eyes—and like any muscles, it’s not a case of “do it once and enjoy the results forever”. So, even just 2–3 minutes each day is recommended.
For more on all of this plus a visual demonstration, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Are Your Glasses Making Your Eyesight Worse?
or, if you are very serious about having excellent vision for life:
Vision for Life, Revised Edition – by Dr. Meir Schneider ← this one’s a book, and a very good one at that
Take care!
Share This Post
-
Why Curcumin (Turmeric) Is Worth Its Weight In Gold
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Curcumin (Turmeric) is worth its weight in gold
Not financially! But, this inexpensive golden spice has an impressive list of well-studied health benefits, for something so freely available in any supermarket, and there’s a reason it gets a place in “Dr. Greger’s Daily Dozen”, right up there with things like “leafy greens” and “berries” when it comes to superfoods.
Let’s do a quick run-down:
- It fights inflammation, and thus helps fight many diseases where inflammation is a factor (ranging from atherosclerosis to arthritis to Alzheimer’s and more)
- It has powerful antioxidant effects too
- It boosts brain-derived neurotropic factor (BDNF) and thus improves memory and attention
- It helps protect against heart disease…
- …and can give a 65% decreased risk of experiencing a heart attack
- It can help prevent cancer, and reduce cancerous lesions by 40%
- It’s also good against depression
- It even slows aging
In short, it’s—like we said—worth its weight in gold.
Quick advice though before we move on…
If you take curcumin with black pepper, it allows your body to use the curcumin around 2,000% better. This goes whether you’re cooking with both, or take them as a supplement (they’re commonly sold as a combo-capsule for this reason).
Want to get some?
Share This Post
-
Is still water better for you than sparkling water?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Still or sparkling? It’s a question you’ll commonly hear in a café or restaurant and you probably have a preference. But is there any difference for your health?
If you love the fizz, here’s why you don’t have to pass on the sparkling water.
Brent Hofacker/Shutterstock What makes my water sparkle?
This article specifically focuses on comparing still filtered water to carbonated filtered water (called “sparkling water” or “unflavoured seltzer”). Soda water, mineral water, tonic water and flavoured water are similar, but not the same product.
The bubbles in sparkling water are created by adding carbon dioxide to filtered water. It reacts to produce carbonic acid, which makes sparkling water more acidic (a pH of about 3.5) than still (closer to neutral, with a pH around 6.5-8.5).
Which drink is healthiest?
Water is the best way to hydrate our bodies. Research shows when it comes to hydration, still and sparkling water are equally effective.
Some people believe water is healthier when it comes from a sealed bottle. But in Australia, tap water is monitored very carefully. Unlike bottled water, it also has the added benefit of fluoride, which can help protect young children against tooth decay and cavities.
Sparkling or still water is always better than artificially sweetened flavoured drinks or juices.
Isn’t soda water bad for my teeth and bones?
There’s no evidence sparkling water damages your bones. While drinking a lot of soft drinks is linked to increased fractures, this is largely due to their association with higher rates of obesity.
Sparkling water is more acidic than still water, and acidity can soften the teeth’s enamel. Usually this is not something to be too worried about, unless it is mixed with sugar or citrus, which has much higher levels of acidity and can harm teeth.
However, if you grind your teeth often, the softening could enhance the damage it causes. If you’re undertaking a home whitening process, sparkling water might discolour your teeth.
In most other cases, it would take a lot of sparkling water to pass by the teeth, for a long period of time, to cause any noticeable damage.
How does drinking water affect digestion?
There is a misconception drinking water (of any kind) with a meal is bad for digestion.
While theoretically water could dilute stomach acid (which breaks down food), the practice of drinking it doesn’t appear to have any negative effect. Your digestive system simply adapts to the consistency of the meal.
Some people do find that carbonated beverages cause some stomach upset. This is due to the build-up of gases, which can cause bloating, cramping and discomfort. For people with an overactive bladder, the acidity might also aggravate the urinary system.
Interestingly, the fizzy “buzz” you feel in your mouth from sparkling water fades the more you drink it.
Is cold water harder to digest?
You’ve chosen still or sparkling water. What about its temperature?
There are surprisingly few studies about the effect of drinking cold water compared to room temperature. There is some evidence colder water (at two degrees Celsius) might inhibit gastric contractions and slow down digestion. Ice water may constrict blood vessels and cause cramping.
However other research suggests drinking cold water might temporarily boost metabolism, as the body needs to expend energy to warm it up to body temperature. This effect is minimal and unlikely to lead to significant weight loss.
Which water wins?
The bottom line is water is essential, hydrates us and has countless other health benefits. Water, with carbonated bubbles or without, will always be the healthiest drink to choose.
And if you’re concerned about any impact to teeth enamel, one trick is to follow sparkling water with a glass of still. This helps rinse the teeth and return your mouth’s acidity back to normal.
Christian Moro, Associate Professor of Science & Medicine, Bond University and Charlotte Phelps, Senior Teaching Fellow, Medical Program, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
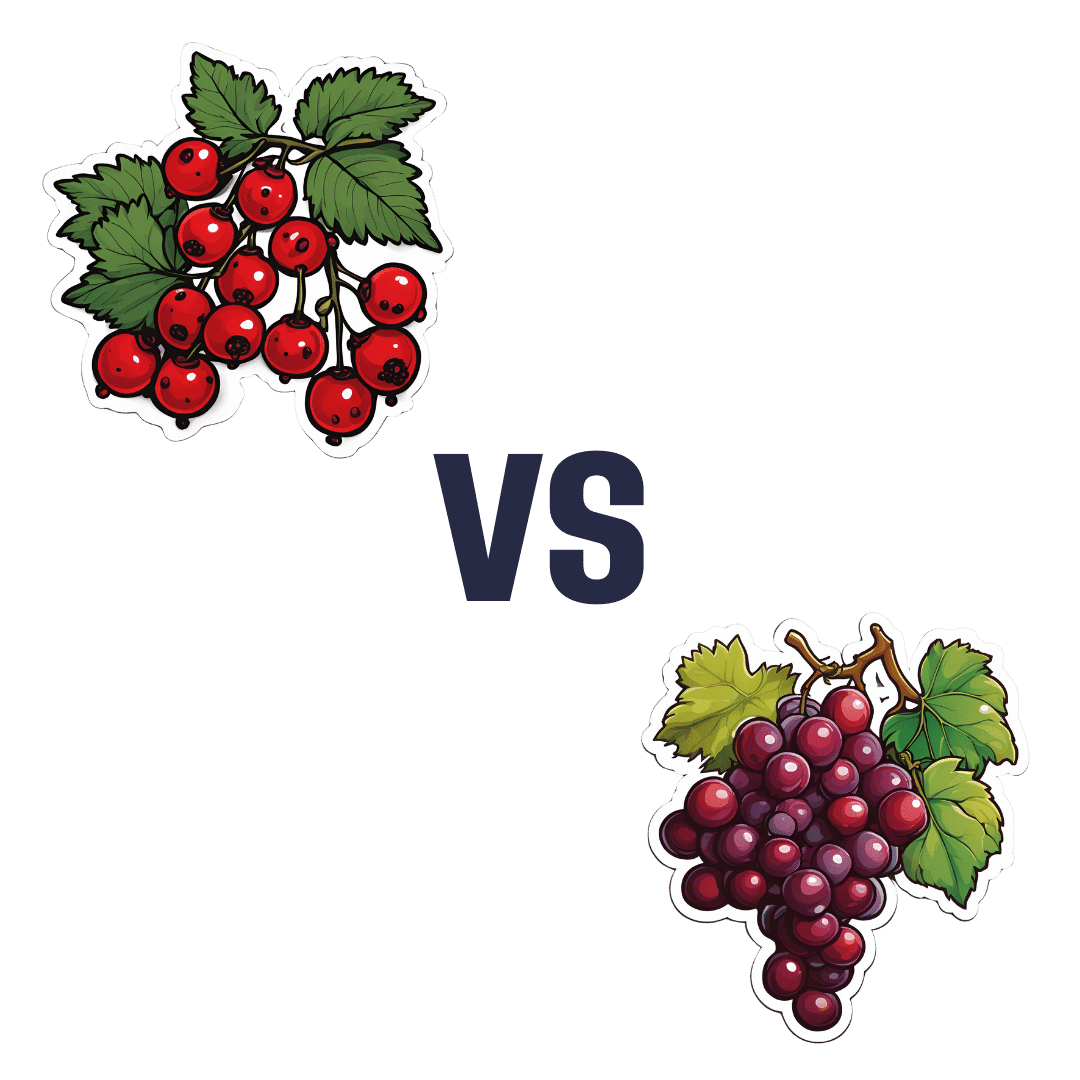
Currants vs Grapes – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing currants to grapes, we picked the currants.
Why?
First, a note on nomenclature: when we say “currants”, we are talking about actual currants, of the Ribes genus, and in this case (as per the image) red ones. We are not talking about “currants” that are secretly tiny grapes that also get called currants in the US. So, there are important botanical differences here, beyond how they have been cultivated; they are literally entirely different plants.
So, about those differences…
In terms of macros, currants have nearly 5x the fiber, while grapes are slightly higher in carbs. So there’s an easy choice here in terms of fiber and on the glycemic index front; currants win easily.
In the category of vitamins, currants have more of vitamins B5, B9, C, and choline, while grapes have more of vitamins A, B1, B2, B3, B6, E, and K. So, a win for grapes in this round.
When it comes to minerals, currants have more calcium, copper, iron, magnesium, phosphorus, potassium, selenium, and zinc, while grapes have more manganese. A win, therefore, for currants again this time.
In terms of polyphenols, currants have a lot more in terms of total polyphenols, including (as a matter of interest) approximately 5x the resveratrol content compared to grapes—and that’s compared to black grapes, which are the “best” kind of grapes for such. Grapes really aren’t a very good source of resveratrol; people just really like the idea of red wine being a health food, so it has been talked up a lot and got a popular reputation despite its extreme paucity of nutritional value.
In any case, adding up the sections makes for a clear overall win for currants, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
21 Most Beneficial Polyphenols & What Foods Have Them
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Prevention Is Better Than Cure
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Preventative healthcare is the theme this week:
New year, new risks
The start of a new year is a great time to update adult vaccinations, including the flu shot, any COVID-19 boosters, and vaccines for pneumonia, shingles, and tetanus—when was your last booster, after all? Vaccination recommendations vary by age and health conditions, so do check what’s appropriate in your case. Key vaccines include the pneumonia vaccine for those 65 and older, the shingles vaccine for adults over 50, and the Tdap vaccine every 10 years to protect against tetanus, diphtheria, and pertussis (whooping cough), especially for new parents and grandparents, to protect infants:
Read in full: Why it’s important to update adult vaccinations for a new year
Related: The Truth About Vaccines
The heart-healthiest swap you can do
Based on a large (n=202,863, of which 160,123 women and 42,740 men) dataset, a higher plant-to-animal protein ratio is associated with significantly lower risks of cardiovascular disease (CVD) and coronary artery disease (CAD), with diets lower in meat (especially if lower in red meat) and instead rich in plant-based proteins like legumes, nuts, and whole grains reducing CVD risk by 19% and coronary artery disease risk by 27%. Which is quite considerable.
Substituting even small amounts of animal protein (especially if it’s red meat) with plant protein further enhances heart health:
Read in full: Higher plant-to-animal protein ratio linked to lower risk for CVD, CAD among U.S. adults
Related: Plant vs Animal Protein: Head to Head
Let’s keep pan-resistant superbugs at bay
Researchers want to warn us about the threat of pan-resistant bacteria, which could render all known antibiotics ineffective, leading to a sharp rise in global infection-related deaths.
To be clear, we don’t have anything pan-resistant yet, but antibiotic-resistant superbugs are getting close, and in the long term, are likely to win the evolutionary arms race if we don’t change things to diverge considerably from our current path. Modeling a hypothetical pan-resistant E. coli strain, researchers predicted U.S. sepsis deaths could increase 18- to 46-fold within five years of its emergence.
The study calls for urgent action, including stricter antibiotic stewardship, new drug development, and monitoring technologies, emphasizing that without intervention, the global impact could be catastrophic:
Read in full: A public health emergency is waiting at the bottom of the antibiotic resistance cliff
Related: Stop Sabotaging Your Immune System ← see also (linked therein), 4 ways antibiotics can kill you
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Food Expiration Dates Don’t Mean What Most People Think They Mean
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Have you ever wondered why rock salt that formed during the Precambrian era has a label on it saying that it expires next month? To take something more delicate, how about eggs that expire next Thursday; isn’t that oddly specific for something that is surely affected by many variables? What matters, and what doesn’t?
Covering their assets
The US in particular wastes huge amounts of food, with 37% of food waste coming from households. Confusion over date labels is a major contributor, accounting for 20% of household food waste. Many people misinterpret these labels, often discarding food that is still safe to eat—which is good for the companies selling the food, because then they get to sell you more.
Date labels were introduced in the 70s with the “open dating” system to indicate optimal freshness, not safety. These dates are often conservative, set by manufacturers to ensure food is consumed at its best quality and encourage repeat purchases. However, many foods remain safe well past their labeled dates, including shelf-stable items like pasta, rice, and canned goods, as well as frozen foods stored properly.
Some foods do pose safety risks, especially meat and dairy products, as well as many grain-based foods, all of which which can harbor harmful bacteria. Infant formula labels are strictly regulated for safety. However, most date labels are not linked to health risks, leading to unnecessary waste.
When it comes down to it, our senses of sight, smell, and taste are more reliable than dates on packaging. Some quick pointers and caveats:
- If it has changed color in some way that’s not associated with a healthily ripening fruit or vegetable, that’s probably bad
- If it is moldy, that’s probably bad (but the degree of badness varies from food to food; see the link beneath today’s video for more on that)
- If a container has developed droplets of water on the inside when it didn’t have those before, that’s probably bad (it means something is respiring, and is thus alive, that probably shouldn’t be)
- If it smells bad, that’s probably bad—however this is not a good safety test, because a bad smell may often mean you are inhaling mold spores, which are not good for your lungs.
- If it tastes different than that food usually does, that’s probably bad (especially if it became bitter, pungent, tangy, sour, or cheesy, and does nor normally taste that way).
Some places have trialled clearer labelling, for example a distinction between “expires” and merely “best before”, but public awareness about the distinction is low. Some places have trialled removing dates entirely, to oblige the consumer to use their own senses instead. This is good for the seller in a different way than household food waste is, because it means the seller will have less in-store waste (because they can still sell something that might previously have been labelled as expired).
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: