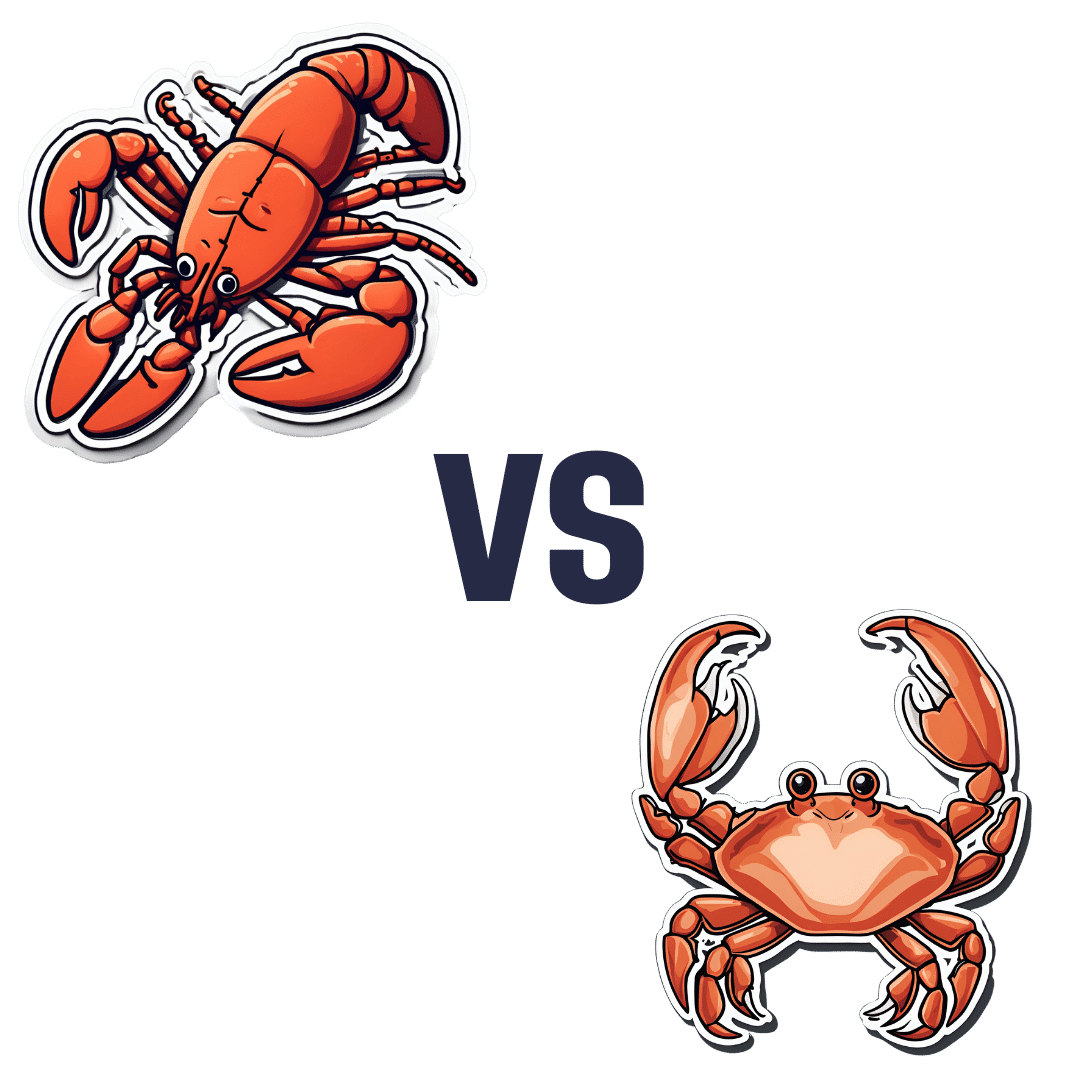
Lobster vs Crab – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing lobster to crab, we picked the crab.
Why?
Generally speaking, most seafood is healthy in moderation (assuming it’s well-prepared, not poisonous, and you don’t have an allergy), and for most people, these two sea creatures are indeed considered a reasonable part of a healthy balanced diet.
In terms of macros, they’re comparable in protein, and technically crab has about 2x the fat, but in both cases it’s next to nothing, so 2x almost nothing is still almost nothing. And, if we break down the lipids profiles, crab has a sufficiently smaller percentage of saturated fat (compared to monounsaturated and polyunsaturated), that crab actually has less saturated fat than lobster. In balance, the category of macros is either a tie or a slight win for crab, depending on your personal priorities.
When it comes to vitamins, crab wins easily with more of vitamins A, B1, B2, B6, B9, B12, and C, in most cases by considerable margins (we’re talking multiples of what lobster has). Lobster, meanwhile, has more of vitamin B3 (tiny margin) and vitamin B5 (pantothenic acid, as in, the vitamin that’s in basically everything edible, and thus almost impossible to be deficient in unless literally starving).
The minerals scene is more balanced; lobster has more calcium, copper, manganese, and selenium, while crab has more iron, magnesium, phosphorus, potassium, and zinc. The margins are comparable from one creature to another, so all in all the 4:5 score means a modest win for crab.
Both of these creatures are good sources of omega-3 fatty acids, but crab is better.
Lobster and crab are both somewhat high in cholesterol, but crab is the relatively lower of the two.
In short: for most people most of the time, both are fine to enjoy in moderation, but if picking one, crab is the healthier by most metrics.
Want to learn more?
You might like to read:
Shrimp vs Caviar – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Top 10 Causes Of High Blood Pressure
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As Dr. Frita Fisher explains, these are actually the top 10 known causes of high blood pressure. Number zero on the list would be “primary hypertension”, which means high blood pressure with no clear underlying cause.
Superficially, this feels a little like the sometime practice of writing the catch-all “heart failure” as the cause of death on a death certificate, because yes, that heart sure did stop beating. But in reality, primary hypertension is most likely often caused by such things as unmanaged chronic stress—something that doesn’t show up on most health screenings.
Dr. Fisher’s Top 10
- Thyroid disease: both hyperthyroidism and hypothyroidism can cause high blood pressure.
- Obstructive sleep apnea: characterized by snoring, daytime sleepiness, and headaches, this condition can lead to hypertension.
- Chronic kidney disease: diseases ranging from diabetic nephropathy to renal vascular disease can cause high blood pressure.
- Elevated cortisol levels: conditions like Cushing’s syndrome or disease, which involve high cortisol levels, can lead to hypertension—as can a lifestyle with a lot of chronic stress, but that’s less readily diagnosed as such than something one can tell from a blood test.
- Elevated aldosterone levels: excess aldosterone from the adrenal glands causes the body to retain salt and water, increasing blood pressure, because more stuff = more pressure.
- Brain tumor: tumors that increase intracranial pressure can cause a rise in blood pressure to ensure adequate brain perfusion. In these cases, the hypertension is keeping you alive—unless it kills you first. If this seems like a strange bodily response, remember that our bodily response to an infection is often fever, to kill off the infection which can’t survive at such high temperatures (but neither can we, so it becomes a game of chicken with our life on the line), so sometimes our body does kill us with one thing while trying to save us from another.
- Coarctation of the aorta: this congenital heart defect results in narrowing of the aorta, leading to hypertension, especially in the upper body.
- Pregnancy: pregnancy can either induce or worsen existing hypertension.
- Obesity: excess weight increases blood flow and pressure on arteries, raising the risk of hypertension and associated conditions, e.g. diabetes etc.
- Drugs: certain medications and recreational drugs (including, counterintuitively, alcohol!) can elevate blood pressure.
For more information on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Hypertension: Factors Far More Relevant Than Salt
Take care!
Share This Post
-
The Most Anti Aging Exercise
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve referenced this (excellent) video before, but never actually put it under the spotlight in one of these features, so here we go!
Deep squats
It’s about deep squats, also called Slav squats, Asian squats, sitting squats, resting squats, or various other names. However, fear not; you don’t need to be Slavic or Asian to do it; you just need to practice.
As for why this is called “anti-aging”, by the way, it’s because being able to get up off the ground is one of the main tests of age-related mobility decline, and if you can deep-squat comfortably, then you can do that easily. And so long as you continue being able to deep-squat comfortably, you’ll continue to be able to get up off the ground easily too, because you have the strength in the right muscles, as well as the suppleness, comfort with range of motion, and balance (those stabilizing muscles are used constantly in a deep squat, whereas Western lifestyle sitting leaves those muscles very neglected and thus atrophied).
Epidemiological note: chairs, couches, and assorted modern conveniences reduce the need for squatting in daily life, leading to stiffness in joints, muscles, tendons, and ligaments. Many adults in developed countries struggle with deep squats due to lack of use, not aging. Which is a problem, because a lack of full range of motion in joints causes wear and tear, leading to chronic pain and degenerative joint diseases. People in countries where squatting is a common resting position have lower incidences of osteoarthritis, for example—contrary to what some might expect, squatting does not harm joints but rather protects them from arthritis and knee pain. Strengthening leg muscles through squatting can alleviate knee pain, whereas knee pain is often worsened by inactivity.
Notwithstanding the thumbnail, which is showing an interim position, one’s feet should be flat on the ground, by the way, and one’s butt should be nearby, just a few inches off the ground (in other words, the position that we see her in for most of this video).
Troubleshooting: if you’re accustomed to sitting in chairs a lot, then this may be uncomfortable at first. Zuzka advises us to go gently, and/but gradually increase our range of motion and (equally importantly) duration in the resting position.
You can use a wall or doorway to partially support you, at first, if you struggle with mobility or balance. Just try to gradually use it less, until you’re comfortable deep-squatting with no support.
Since this is not an intrinsically very exciting exercise, once you build up the duration for which you’re comfortable deep-squatting, it can be good to get in the habit of “sitting” this way (i.e. deep squatting, still butt-off-the-floor, but doing the job of sitting) while doing other things such as working (if you have an appropriate work set-up for that*), reading, or watching TV.
*this is probably easiest with a laptop placed on an object/surface of appropriate height, such as a coffee table or such. As a bonus, having your hands in front of you while working will also bring your center of gravity forwards a bit, making the position easier and more comfortable to maintain. This writer (hi, it’s me) prefers her standing desk for work in general, with a nice ergonomic keyboard and all that, but if using a laptop from time to time, then squatting is a very good option.
In terms of working up duration, if you can only manage seconds to start with, that’s fine. Just do a few more seconds each time, until it’s 30, 60, 120, and so on until it’s 5 minutes, 10, 15, and so on.
You can even start that habit-forming while you’re still in the “seconds at a time” stage! You can deep-squat just for some seconds while you:
- pick up something from the floor
- check on something in the oven
- get something out of the bottom of the fridge
…etc!
For more on all this, plus many visual demonstrations including interim exercises to get you there if it’s difficult for you at first, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Mobility For Now & For Later: Train For The Marathon That Is Your Life!
Take care!
Share This Post
-
Dates vs Grapes – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing dates to grapes, we picked the dates.
Why?
It’s not close:
In terms of macros, dates have 4x the carbs and/but 8x the fiber, making for the lower glycemic index. Also, for what it’s worth, they have nearly 4x the protein, but probably nobody is eating either of these fruits for the protein. In any case, it’s an easy and clear win for dates in the category of macros.
In the category of vitamins, dates have more of vitamins B2, B3, B5, B6, B9, and choline, while grapes have more of vitamins B1, C, E, and K, making for a 6:4 win for dates.
When it comes to minerals, it’s more one-sided: dates have more calcium, copper, iron, magnesium, phosphorus, potassium, selenium, and zinc, while grapes have more manganese. An easy win for dates here.
Of course, enjoy either or both (diversity is good), but if you’re looking for nutrient density, dates are where it’s at.
Want to learn more?
You might like:
Can We Drink To Good Health? ← while there are polyphenols such as resveratrol in red wine that per se would boost heart health, there’s so little per glass that you may need 100–1000 glasses per day to get the dosage that provides benefits in mouse studies.
If you’re not a mouse, you might even need more than that!
To this end, many people prefer resveratrol supplementation ← link is to an example product on Amazon, but there are plenty more so feel free to shop around 😎
Enjoy!
Share This Post
Related Posts
-
Time Smart – by Dr. Ashley Whillans
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this is not: it’s not a productivity book.
What is rather: a book of better wellbeing.
There is a little overlap, insofar as getting “time smart” in the ways that Dr. Whillans recommends will give you more ability to also be more productive—if that’s what you want.
She talks us through time traps and the “time poverty epidemic”, as well as steps to finding time and funding time. Perhaps most critical idea-wise is the chapter on building a “time-affluence habit”, making decisions that prioritize your time-freedom where you can—which in turn will allow you to build yet more. Kind of like compound interest really, but for time.
The writing style is a conversational tone, but peppered with bullet-point lists and charts and the like from time to time, and often with citations to back up claims. It makes for a very readable book, and yet one that’s also inspiring of the confidence that it’s more than just one person’s opinion.
Bottom line: if you sometimes feel like you could do everything you want to if you could just find the time, this book can help you get there.
Click here to check out Time Smart, and live your most satisfying life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Reason You’re Alone
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you are feeling lonely, then there are likely reasons why, as Kurtzgesagt explains:
Why it happens and how to fix it
Many people feel lonely and disconnected, often not knowing how to make new friends. And yet, social connection strongly predicts happiness, while lack of it is linked to diseases and a shorter life.
One mistake that people make is thinking it has to be about shared interests; that can help, but proximity and shared time are much more important.
Another stumbling block for many is that adult responsibilities and distractions (work, kids, technology) often take priority over friendships—but loneliness is surprisingly highest among young people, worsened by the pandemic’s impact on social interactions.
And even when friendships are made, they fade without attention, often accidentally, impacting both people involved. Other friendships can be lost following big life changes such as moving house or the end of a relationship. And for people above a certain advanced age, friendship groups can shrink due to death, if one’s friends are all in the same age group.
But, all is not lost. We can make friends with people of any age, and old friendships can be revived by a simple invitation. We can also take a “build it and they will come” approach, by organizing events and being the one who invites others.
It’s easy to fear rejection—most people do—but it’s worth overcoming for the potential rewards. That said, building friendships requires time, patience, caring about others, and being open about yourself, which can involve a degree of vulnerability too.
In short: be laid-back while still prioritizing friendships, show genuine interest, and stay open to social opportunities.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Beat Loneliness & Isolation
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Art and Science of Connection – by Kasley Killam, MPH
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We can eat well, exercise well, and even sleep well, and we’ll still have a +53% increased all-cause mortality if we lack social connection—even if we technically have support and access to social resources, just not the real human connection itself. And as we get older, it gets increasingly easy to find ourselves isolated.
The author is a social scientist by profession, and it shows. None of what she shares in the book is wishy-washy; it has abundant scientific references coming thick and fast, and a great deal of clarity with regard to terms, something often not found in books of this genre that lean more towards the art than the science.
On which note, for the reader who may be thinking “I am indeed quite alone”, she also offers proven techniques for remedying that; not in the way that many books use the word “proven” to mean “we got some testimonials”, but rather, proven in the sense of “we did science to it and based on these 17 large population-based retrospective cohort studies, we can say with 99% confidence that this is an effective tool to mediate improved social bonds and social health outcomes”.
To this end, it’s a very practical book also, and should bestow upon any isolated reader a sense of confidence that in fact, things can be better. A particular strength is that it also looks at many different scenarios, so for the “what if I…” people with clear reasons why social connection is not abundantly available, yes, she has such cases covered too.
Bottom line: if you’d like to live more healthily for longer, social health is an underrated and oft-forgotten way of greatly increasing those things, by science.
Click here to check out The Art And Science Of Social Connection, and get connected!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: