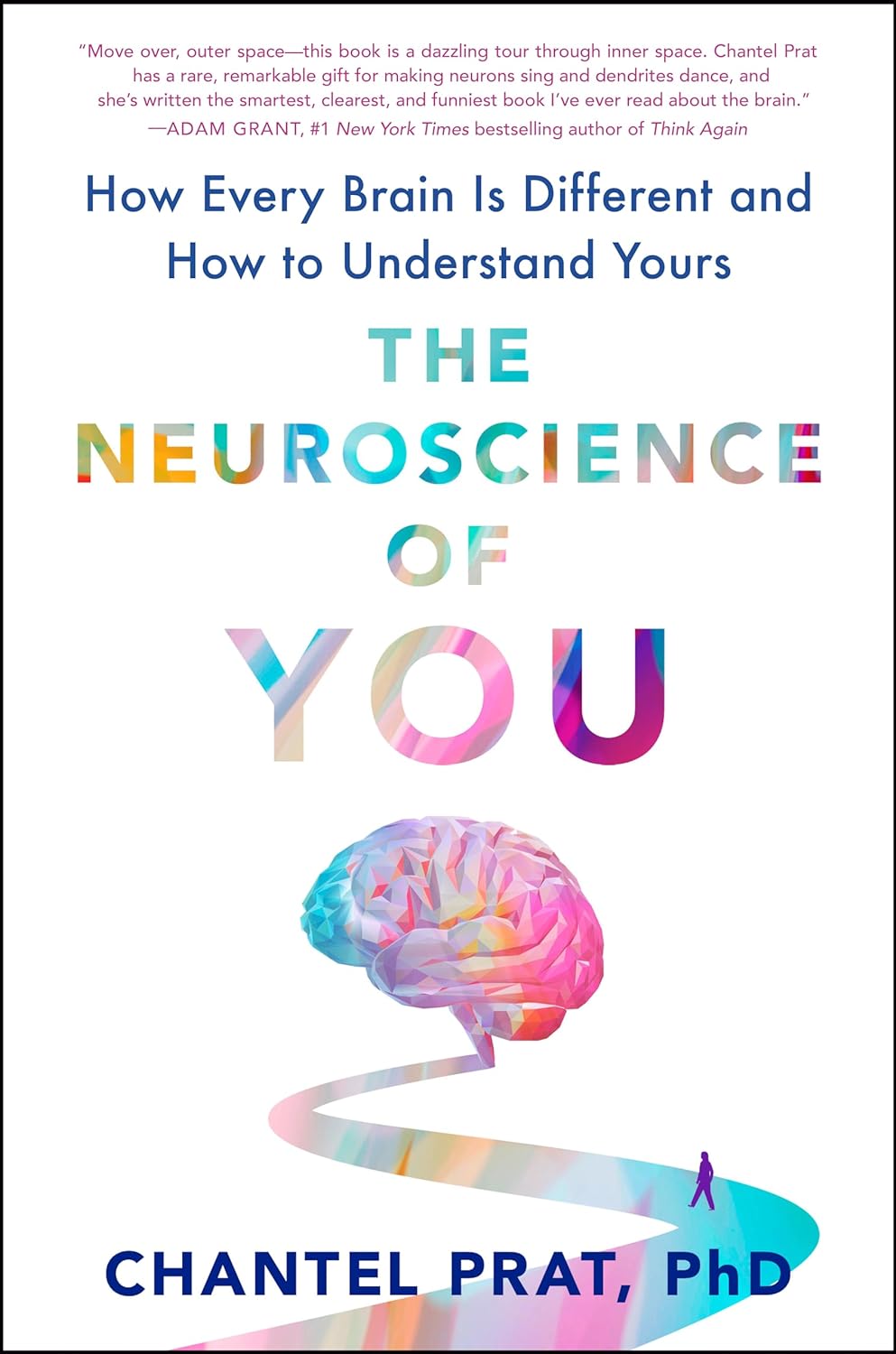
The Neuroscience of You – by Dr. Chantel Prat
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The insides of people are rarely so standardized as one finds in a medical textbook, and that’s just as true of the brain as it is of any other organ—and often more so.
Our brains all look quite different from each other’s. Of course there are similarities; a wobbly mass of white and grey matter with tiny blood vessels running through. The constituent parts are (usually!) all present and correct. But… what is “correct”?
Dr. Chantel Prat takes us on a tour of the anatomical features that we may have grown or shrunken over the course of our life, according to how we’ve used them, or not. She also looks at what’s going on when it comes to the smaller scale—from the neuronal to the neurochemical.
We learn the truth (and myth) when it comes to left- and right-brainedness, and we learn how whether we saw that dress as black and blue or white and gold, depends on our circadian rhythm (and thus whether we have wired ourselves for perceiving colors more or less often under daylight or artificial light). And lots more.
The style throughout is very accessible, for a book that goes beyond most “how the brain works” books.
Bottom line: if you’re interested in the workings of your brain (as opposed to: a standardized Platonic ideal of what a brain might be), then this book will set you on the right track.
Click here to check out The Neuroscience of You, and learn more about what makes you you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Considering taking Wegovy to lose weight? Here are the risks and benefits – and how it differs from Ozempic
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The weight-loss drug Wegovy is now available in Australia.
Wegovy is administered as a once-weekly injection and is approved specifically for weight management. It’s intended to be used in combination with a reduced-energy diet and increased physical activity.
So how does Wegovy work and how much weight can you expect to lose while taking it? And what are the potential risks – and costs – for those who use it?
Let’s look at what the science says.

Halfpoint/Shutterstock What is Wegovy?
Wegovy is a brand name for the medication semaglutide. Semaglutide is a glucagon-like peptide-1 receptor agonist (GLP-1RA). This means it makes your body’s own glucagon-like peptide-1 hormone, called GLP-1 for short, work better.
Normally when you eat, the body releases the GLP-1 hormone which helps signal to your brain that you are full. Semaglutides enhance this effect, leading to a feeling of fullness, even when you haven’t eaten.
Another role of GLP-1 is to stimulate the body to produce more insulin, a hormone which helps lower the level of glucose (sugar) in the blood. That’s why semaglutides have been used for several years to treat type 2 diabetes.

Wegovy is self-injected once a week. S Becker/Shutterstock How does Wegovy differ from Ozempic?
Like Wegovy, Ozempic is a semaglutide. The way Wegovy and Ozempic work in the body are essentially the same. They’re made by the same pharmaceutical company, Novo Nordisk.
But there are two differences:
1) They are approved for two different (but related) reasons.
In Australia (and the United States), Ozempic is approved for use to improve blood glucose levels in adults with type 2 diabetes. By managing blood glucose levels effectively, the medication aims to reduce the risk of major complications, such as heart disease.
Wegovy is approved for use alongside diet and exercise for people with a body mass index (BMI) of 30 or greater, or 27 or greater but with other conditions such as high blood pressure.
Wegovy can also be used in people aged 12 years and older. Like Ozempic, Wegovy aims to reduce the risk of future health complications, including heart disease.
2) They are both injected but come in different strengths.
Ozempic is available in pre-loaded single-dose pens with varying dosages of 0.25 mg, 0.5 mg, 1 mg, or 2 mg per injection. The dose can be slowly increased, up to a maximum of 2 mg per week, if needed.
Wegovy is available in prefilled single-dose pens with doses of 0.25 mg, 0.5 mg, 1 mg, 1.7 mg, or 2.4 mg. The treatment starts with a dose of 0.25 mg once weekly for four weeks, after which the dose is gradually increased until reaching a maintenance dose of 2.4 mg weekly.
While it’s unknown what the impact of Wegovy’s introduction will be on Ozempic’s availability, Ozempic is still anticipated to be in low supply for the remainder of 2024.
Is Wegovy effective for weight loss?
Given Wegovy is a semaglutide, there is very strong evidence it can help people lose weight and maintain this weight loss.
A recent study found that over four years, participants taking Wevovy as indicated experienced an average weight loss of 10.2% body weight and a reduction in waist circumference of 7.7cm.
For those who stop taking the medication, analyses have shown that about two-thirds of weight lost is regained.

Wegovy can help people lose weight and maintain their weight loss – while they take the drug. Mladen Mitrinovic/Shutterstock What are the side effects of Wegovy?
The most common side effects are nausea and vomiting.
However, other serious side effects are also possible because of the whole-of-body impact of the medication. Thyroid tumours and cancer have been detected as a risk in animal studies, yet are rarely seen in human scientific literature.
In the four-year Wegovy trial, 16.6% of participants who received Wegovy (1,461 people) experienced an adverse event that led to them permanently discontinuing their use of the medication. This was higher than the 8.2% of participants (718 people) who received the placebo (with no active ingredient).
Side effects included gastrointestinal disorders (including nausea and vomiting), which affected 10% of people who used Wegovy compared to 2% of people who used the placebo.
Gallbladder-related disorders occurred in 2.8% of people who used Wegovy, and 2.3% of people who received the placebo.
Recently, concerns about suicidal thoughts and behaviours have been raised, after a global analysis reviewed more than 36 million reports of adverse events from semaglutide (Ozempic or Wegovy) since 2000.
There were 107 reports of suicidal thoughts and self-harm among people taking semaglutide, sadly including six actual deaths. When people stopped the medication, 62.5% found the thoughts went away. What we don’t know is whether dose, weight loss, or previous mental health status or use of antidepressants had a role to play.
Finally, concerns are growing about the negative effect of semaglutides on our social and emotional connection with food. Anecdotal and scientific evidence suggests people who use semaglutides significantly reduce their daily dietary intake (as anticipated) by skipping meals and avoiding social occasions – not very enjoyable for people and their loved ones.
How can people access Wegovy?
Wegovy is available for purchase at pharmacists with a prescription from a doctor.
But there is a hefty price tag. Wegovy is not currently subsidised through the Pharmaceutical Benefits Scheme, leaving patients to cover the cost. The current cost is estimated at around A$460 per month dose.
If you’re considering Wegovy, make an appointment with your doctor for individual advice.
Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland and Emily Burch, Accredited Practising Dietitian and Lecturer, Southern Cross University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post

Blood-Sugar-Friendly Ice Pops
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This generic food product has so many regional variant names that it’s difficult to get a universal name, but in N. America they’re also known by the genericized brand name of popsicles. Anyway, they’re usually very bad news for blood sugars, being merely frozen juice even if extra sugar wasn’t added. Today’s recipe, on the other hand, makes for a refreshing and nutrient-dense treat that won’t spike your blood glucose!
You will need
- 1 cup fresh blueberries
- 1 can (12oz/400g) coconut milk
- ½ cup yogurt with minimal additives
- 1 tbsp honey (omit if you prefer less sweetness)
- Juice of ¼ lime (increase if you prefer more sourness)
Method
(we suggest you read everything at least once before doing anything)
1) Blend everything
2) Pour into ice pop molds and freeze overnight
3) Serve at your leisure:

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Which Sugars Are Healthier, And Which Are Just The Same?
- 10 Ways To Balance Blood Sugars
- Can Saturated Fats Be Healthy? ← the fats in coconut are a good source of medium-chain triglycerides (MCTs), which are easily broken down as a good energy source and (enjoyed in moderation) thus unlikely to cause any cardiovascular problems, as little to nothing (usually: nothing) of it will be stored.
Take care!
Share This Post

Why Everyone You Don’t Like Is A Narcissist
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about how psychiatry tends to name disorders after how they affect other people, rather than how they affect the bearer, and this is most exemplified when it comes to personality disorders. For example:
“You have a deep insecurity about never being good enough, and you constantly mess up in your attempt to overcompensate? You may have Evil Bastard Disorder!”
“You have a crippling fear of abandonment and that you are fundamentally unloveable, so you do all you can to try to keep people close? You must have Manipulative Bitch Disorder!”
See also: Miss Diagnosis: Anxiety, ADHD, & Women
Antisocial DiagnosesThese days, it is easy to find on YouTube countless videos of how to spot a narcissist, with a list of key traits that all mysteriously describe exactly the exes of everyone in the comments.
And these days it is mostly “narcissist”, because “psychopath” and “sociopath” have fallen out of popular favor a bit:
- perhaps for coming across as overly sensationalized, and thus lacking credibility
- perhaps because “Narcissistic Personality Disorder (NPD)” exists in the DSM-5 (the US’s latest “Diagnostic and Statistical Manual of Mental Disorders”), while psychopathy and sociopathy are not mentioned as existing.
You may be wondering: what do “psychopathy” and “sociopathy” mean?
And the answer is: they mean whatever the speaker wants them to mean. Their definitions and differences/similarities have been vigorously debated by clinicians and lay enthusiasts alike for long enough that the scientific world has pretty much given up on them and moved on.
Stigma vs pathology
Because of the popular media (and social media) representation of NPD, it is easy to armchair diagnose one’s relative/ex/neighbor/in-law/boss/etc as being a narcissist, because the focus is on “narcissists do these bad things that are mean to people”.
If the focus were instead on “narcissists have cripplingly low self-esteem, and are desperate to not show weakness in a world they have learned is harsh and predatory”, then there may not be so many armchair diagnoses—or at the very least, the labels may be attached with a little more compassion, the same way we might with other mental health issues such as depression.
Not that those with depression get an easy time of it socially either—society’s response is generally some manner of “aren’t you better yet, stop being lazy”—but at the very least, depressed people are not typically viewed with hatred.
A quick aside: if you or someone you know is struggling with depression, here are some things that actually help:
The Mental Health First-Aid You’ll Hopefully Never Need
The disorder is not the problem
Maybe your relative, ex, neighbor, etc really is clinically diagnosable as a narcissist. There are still two important things to bear in mind:
- After centuries of diagnosing people with mental health maladies that we now know don’t exist per se (madness, hysteria, etc), and in recent decades countless revisions to the DSM and similar tomes, thank goodness we now have the final and perfect set of definitions that surely won’t be re-written in the next few years or so ← this is irony; it will absolutely be re-written numerous times yet because of course it’s still not a magically perfect descriptor of the broad spectrum of human nature
- The disorder is not the problem; the way they treat (or have treated) you is the problem.
For example, let’s take a key thing generally attributed to narcissists: a lack of empathy
Now, empathy can be divided into:
- affective empathy: the ability to feel what other people are feeling
- cognitive empathy: the ability to intellectually understand what other people are feeling (akin to sympathy, which is the same but with the requisite of having experienced the thing in question oneself)
A narcissist (as well as various other people without NPD) will typically have negligible affective empathy, and their cognitive empathy may be a little sluggish too.
Sluggish = it may take them a beat longer than most people, to realize what an external signifier of emotions means, or correctly guess how something will be felt by others. This can result in gravely misspeaking (or inappropriately emoting), after failing to adequately quickly “read the room” in terms of what would be a socially appropriate response. To save face, they may then either deny/minimize the thing they just said/did, or double-down on it and go on [what for them feels like] the counterattack.
As to why this shutting off of empathy happens: they have learned that the world is painful, and that people are sources of pain, and so—to avoid further pain—have closed themselves off to that, often at a very early age. This will also apply to themselves; narcissists typically have negligible self-empathy too, which is why they will commonly make self-destructive decisions, even while trying to put themselves first.
Important note on how this impacts other people: the “Golden Rule” of “treat others as you would wish to be treated” becomes intangible, as they have no more knowledge of their own emotional needs than they do of anyone else’s, so cannot make that comparison.
Consider: if instead of being blind to empathy, they were colorblind… You would probably not berate them for buying green apples when you asked for red. They were simply incapable of seeing that, and consequently made a mistake. So it is when it’s a part of the brain that’s not working normally.
So… Since the behavior does adversely affect other people, what can be done about it? Even if “hate them for it and call for their eradication from the face of the Earth” is not a reasonable (or compassionate) option, what is?
Take the bull by the horns
Above all, and despite all appearances, a narcissist’s deepest desire is simply to be accepted as good enough. If you throw them a life-ring in that regard, they will generally take it.
So, communicate (gently, because a perceived attack will trigger defensiveness instead, and possibly a counterattack, neither of which are useful to anyone) what behavior is causing a problem and why, and ask them to do an alternative thing instead.
And, this is important, the alternative thing has to be something they are capable of doing. Not merely something that you feel they should be capable of doing, but that they are actually capable of doing.
- So not: “be a bit more sensitive!” because that is like asking the colorblind person to “be a bit more observant about colors”; they are simply not capable of it and it is folly to expect it of them, because no matter how hard they try, they can’t.
- But rather: “it upsets me when you joke about xyz; I know that probably doesn’t make sense to you and that’s ok, it doesn’t have to. I am asking, however, if you will please simply refrain from joking about xyz. Would you do that for me?”
Presented with such, it’s much more likely that the narcissist will drop their previous attempt to be good enough (by joking, because everyone loves someone with a sense of humor, right?) for a new, different attempt to be good enough (by showing “behold, look, I am a good person and doing the thing you asked, of which I am capable”).
That’s just one example, but the same methodology can be applied to most things.
For tricks pertaining to how to communicate such things without causing undue resistance, see:
Seriously Useful Communication Skills
Take care!
Share This Post
Related Posts

Getting antivirals for COVID too often depends on where you live and how wealthy you are
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Medical experts recommend antivirals for people aged 70 and older who get COVID, and for other groups at risk of severe illness and hospitalisation from COVID.
But many older Australians have missed out on antivirals after getting sick with COVID. It is yet another way the health system is failing the most vulnerable.

CGN089/Shutterstock Who missed out?
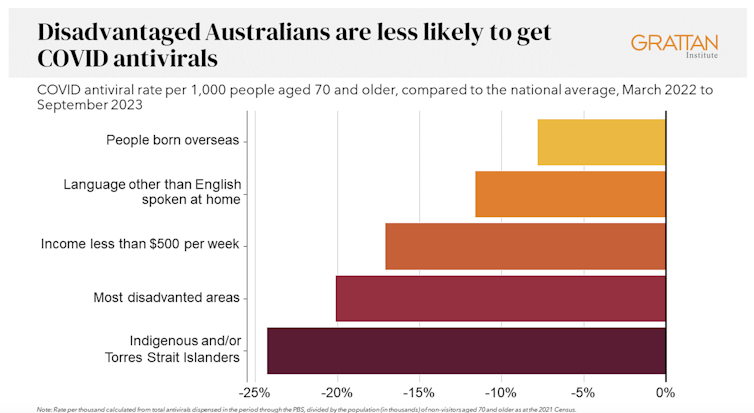
We analysed COVID antiviral uptake between March 2022 and September 2023. We found some groups were more likely to miss out on antivirals including Indigenous people, people from disadvantaged areas, and people from culturally and linguistically diverse backgrounds.
Some of the differences will be due to different rates of infection. But across this 18-month period, many older Australians were infected at least once, and rates of infection were higher in some disadvantaged communities.
How stark are the differences?
Compared to the national average, Indigenous Australians were nearly 25% less likely to get antivirals, older people living in disadvantaged areas were 20% less likely to get them, and people with a culturally or linguistically diverse background were 13% less likely to get a script.
People in remote areas were 37% less likely to get antivirals than people living in major cities. People in outer regional areas were 25% less likely.

Dispensing rates by group. Grattan Institute Even within the same city, the differences are stark. In Sydney, people older than 70 in the affluent eastern suburbs (including Vaucluse, Point Piper and Bondi) were nearly twice as likely to have had an antiviral as those in Fairfield, in Sydney’s south-west.
Older people in leafy inner-eastern Melbourne (including Canterbury, Hawthorn and Kew) were 1.8 times more likely to have had an antiviral as those in Brimbank (which includes Sunshine) in the city’s west.
Why are people missing out?
COVID antivirals should be taken when symptoms first appear. While awareness of COVID antivirals is generally strong, people often don’t realise they would benefit from the medication. They wait until symptoms get worse and it is too late.
Frequent GP visits make a big difference. Our analysis found people 70 and older who see a GP more frequently were much more likely to be dispensed a COVID antiviral.
Regular visits give an opportunity for preventive care and patient education. For example, GPs can provide high-risk patients with “COVID treatment plans” as a reminder to get tested and seek treatment as soon as they are unwell.
Difficulty seeing a GP could help explain low antiviral use in rural areas. Compared to people in major cities, people in small rural towns have about 35% fewer GPs, see their GP about half as often, and are 30% more likely to report waiting too long for an appointment.
Just like for vaccination, a GP’s focus on antivirals probably matters, as does providing care that is accessible to people from different cultural backgrounds.
Care should go those who need it
Since the period we looked at, evidence has emerged that raises doubts about how effective antivirals are, particularly for people at lower risk of severe illness. That means getting vaccinated is more important than getting antivirals.
But all Australians who are eligible for antivirals should have the same chance of getting them.
These drugs have cost more than A$1.7 billion, with the vast majority of that money coming from the federal government. While dispensing rates have fallen, more than 30,000 packs of COVID antivirals were dispensed in August, costing about $35 million.
Such a huge investment shouldn’t be leaving so many people behind. Getting treatment shouldn’t depend on your income, cultural background or where you live. Instead, care should go to those who need it the most.

Getting antivirals shouldn’t depend on who your GP is. National Cancer Institute/Unsplash People born overseas have been 40% more likely to die from COVID than those born here. Indigenous Australians have been 60% more likely to die from COVID than non-Indigenous people. And the most disadvantaged people have been 2.8 times more likely to die from COVID than those in the wealthiest areas.
All those at-risk groups have been more likely to miss out on antivirals.
It’s not just a problem with antivirals. The same groups are also disproportionately missing out on COVID vaccination, compounding their risk of severe illness. The pattern is repeated for other important preventive health care, such as cancer screening.
A 3-step plan to meet patients’ needs
The federal government should do three things to close these gaps in preventive care.
First, the government should make Primary Health Networks (PHNs) responsible for reducing them. PHNs, the regional bodies responsible for improving primary care, should share data with GPs and step in to boost uptake in communities that are missing out.
Second, the government should extend its MyMedicare reforms. MyMedicare gives general practices flexible funding to care for patients who live in residential aged care or who visit hospital frequently. That approach should be expanded to all patients, with more funding for poorer and sicker patients. That will give GP clinics time to advise patients about preventive health, including COVID vaccines and antivirals, before they get sick.
Third, team-based pharmacist prescribing should be introduced. Then pharmacists could quickly dispense antivirals for patients if they have a prior agreement with the patient’s GP. It’s an approach that would also work for medications for chronic diseases, such as cardiovascular disease.
COVID antivirals, unlike vaccines, have been keeping up with new variants without the need for updates. If a new and more harmful variant emerges, or when a new pandemic hits, governments should have these systems in place to make sure everyone who needs treatment can get it fast.
In the meantime, fairer access to care will help close the big and persistent gaps in health between different groups of Australians.
Peter Breadon, Program Director, Health and Aged Care, Grattan Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Oats vs Pearl Barley – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing oats to pearl barley, we picked the oats.
Why?
In terms of macronutrients first, pearl barley has about three times the carbs for only the same amount of protein and fiber—if it had been regular barley rather than pearl parley, it’d have about twice the fiber, but pearl barley has had the fibrous husk removed.
Vitamins really set the two part, though: oats have a lot more (60x more) vitamin A, and notably more of vitamins B1, B2, B3, B5, B6, and B9, as well as 6x more vitamin E. In contrast, pearl barley has a little more vitamin K and choline. An easy win for oats in this section.
In the category of minerals, oats have over 6x more calcium, 3x more iron, and a little more magnesium, manganese, and phosphorus. Meanwhile, pearl barley boats a little more copper, potassium, selenium, and zinc. So, a more moderate win for oats in this category.
They are both very good for the gut, unless you have a gluten intolerance/allergy, in which case, oats are the only answer here since pearl barley, as per barley in general, has gluten as its main protein (oats, meanwhile, do not contain gluten, unless by cross-contamination).
Adding up all the sections, this one’s a clear win for oats.
Want to learn more?
You might like to read:
- Eat More (Of This) For Lower Blood Pressure
- Making Friends With Your Gut (You Can Thank Us Later)
- Gluten: What’s The Truth?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Patient Underwent One Surgery but Was Billed for Two. Even After Being Sued, She Refused To Pay.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Jamie Holmes says a surgery center tried to make her pay for two operations after she underwent only one. She refused to buckle, even after a collection agency sued her last winter.
Holmes, who lives in northwestern Washington state, had surgery in 2019 to have her fallopian tubes tied, a permanent birth-control procedure that her insurance company agreed ahead of time to cover.
During the operation, while Holmes was under anesthesia, the surgeon noticed early signs of endometriosis, a common condition in which fibrous scar tissue grows around the uterus, Holmes said. She said the surgeon later told her he spent about 15 minutes cauterizing the troublesome tissue as a precaution. She recalls him saying he finished the whole operation within the 60 minutes that had been allotted for the tubal ligation procedure alone.
She said the doctor assured her the extra treatment for endometriosis would cost her little, if anything.
Then the bill came.
The Patient: Jamie Holmes, 38, of Lynden, Washington, who was insured by Premera Blue Cross at the time.
Medical Services: A tubal ligation operation, plus treatment of endometriosis found during the surgery.
Service Provider: Pacific Rim Outpatient Surgery Center of Bellingham, Washington, which has since been purchased, closed, and reopened under a new name.
Total Bill: $9,620. Insurance paid $1,262 to the in-network center. After adjusting for prices allowed under the insurer’s contract, the center billed Holmes $2,605. A collection agency later acquired the debt and sued her for $3,792.19, including interest and fees.
What Gives: The surgery center, which provided the facility and support staff for her operation, sent a bill suggesting that Holmes underwent two separate operations, one to have her tubes tied and one to treat endometriosis. It charged $4,810 for each.
Holmes said there were no such problems with the separate bills from the surgeon and anesthesiologist, which the insurer paid.
Holmes figured someone in the center’s billing department mistakenly thought she’d been on the operating table twice. She said she tried to explain it to the staff, to no avail.
She said it was as if she ordered a meal at a fast-food restaurant, was given extra fries, and then was charged for two whole meals. “I didn’t get the extra burger and drink and a toy,” she joked.
Her insurer, Premera Blue Cross, declined to pay for two operations, she said. The surgery center billed Holmes for much of the difference. She refused to pay.
Holmes said she understands the surgery center could have incurred additional costs for the approximately 15 minutes the surgeon spent cauterizing the spots of endometriosis. About $500 would have seemed like a fair charge to her. “I’m not opposed to paying for that,” she said. “I am opposed to paying for a whole bunch of things I didn’t receive.”
The physician-owned surgery center was later purchased and closed by PeaceHealth, a regional health system. But the debt was turned over to a collection agency, SB&C, which filed suit against Holmes in December 2023, seeking $3,792.19, including interest and fees.
The collection agency asked a judge to grant summary judgment, which could have allowed the company to garnish wages from Holmes’ job as a graphic artist and marketing specialist for real estate agents.
Holmes said she filed a written response, then showed up on Zoom and at the courthouse for two hearings, during which she explained her side, without bringing a lawyer. The judge ruled in February that the collection agency was not entitled to summary judgment, because the facts of the case were in dispute.
More From Bill Of The Month
- Her Hearing Implant Was Preapproved. Nonetheless, She Got $139,000 Bills for Months.
- It’s Called an Urgent Care Emergency Center — But Which Is It?
- He Fell Ill on a Cruise. Before He Boarded the Rescue Boat, They Handed Him the Bill.
Representatives of the collection agency and the defunct surgery center declined to comment for this article.
Sabrina Corlette, co-director of Georgetown University’s Center on Health Insurance Reforms, said it was absurd for the surgery center to bill for two operations and then refuse to back down when the situation was explained. “It’s like a Kafka novel,” she said.
Corlette said surgery center staffers should be accustomed to such scenarios. “It is quite common, I would think, for a surgeon to look inside somebody and say, ‘Oh, there’s this other thing going on. I’m going to deal with it while I’ve got the patient on the operating table.’”
It wouldn’t have made medical or financial sense for the surgeon to make Holmes undergo a separate operation for the secondary issue, she said.
Corlette said that if the surgery center was still in business, she would advise the patient to file a complaint with state regulators.
The Resolution: So far, the collection agency has not pressed ahead with its lawsuit by seeking a trial after the judge’s ruling. Holmes said that if the agency continues to sue her over the debt, she might hire a lawyer and sue them back, seeking damages and attorney fees.
She could have arranged to pay off the amount in installments. But she’s standing on principle, she said.
“I just got stonewalled so badly. They treated me like an idiot,” she said. “If they’re going to be petty to me, I’m willing to be petty right back.”
The Takeaway: Don’t be afraid to fight a bogus medical bill, even if the dispute goes to court.
Debt collectors often seek summary judgment, which allows them to garnish wages or take other measures to seize money without going to the trouble of proving in a trial that they are entitled to payments. If the consumers being sued don’t show up to tell their side in court hearings, judges often grant summary judgment to the debt collectors.
However, if the facts of a case are in dispute — for example, because the defendant shows up and argues she owes for just one surgery, not two — the judge may deny summary judgment and send the case to trial. That forces the debt collector to choose: spend more time and money pursuing the debt or drop it.
“You know what? It pays to be stubborn in situations like this,” said Berneta Haynes, a senior attorney for the National Consumer Law Center who reviewed Holmes’ bill for KFF Health News.
Many people don’t go to such hearings, sometimes because they didn’t get enough notice, don’t read English, or don’t have time, she said.
“I think a lot of folks just cave” after they’re sued, Haynes said.
Emily Siner reported the audio story.
After six years, we’ll have a final installment with NPR of our Bill of the Month project in the fall. But Bill of the Month will continue at KFF Health News and elsewhere. We still want to hear about your confusing or outrageous medical bills. Visit Bill of the Month to share your story.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: