Kale vs Watercress – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kale to watercress, we picked the kale.
Why?
It was very close! If ever we’ve been tempted to call something a tie, this has been the closest so far.
Their macros are close; watercress has a tiny amount more protein and slightly lower carbs, but these numbers are tiny, so it’s not really a factor. Nevertheless, on macros alone we’d call this a slight nominal win for watercress.
In terms of vitamins, they’re even. Watercress has higher vitamin E and choline (sometimes considered a vitamin), as well as being higher in some B vitamins. Kale has higher vitamins A and K, as well as being higher in some other B vitamins.
In the category of minerals, watercress has higher calcium, magnesium, phosphorus, and potassium, while kale has higher copper, iron, manganese, and zinc. The margins are slightly wider for kale’s more plentiful minerals though, so we’ll call this section a marginal win for kale.
When it comes to polyphenols, kale takes and maintains the lead here, with around 2x the quercetin and 27x the kaempferol. Watercress does have some lignans that kale doesn’t, but ultimately, kale’s strong flavonoid content keeps it in the lead.
So of course: enjoy both if both are available! But if we must pick one, it’s kale.
Want to learn more?
You might like to read:
- Fight Inflammation & Protect Your Brain, With Quercetin
- Spinach vs Kale – Which is Healthier?
- Thai-Style Kale Chips (recipe)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Magnesium Glycinate vs Magnesium Citrate – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing magnesium glycinate to magnesium citrate, we picked the citrate.
Why?
Both are fine sources of magnesium, a nutrient in which it’s very common to be deficient—a lot of people don’t eat many leafy greens, beans, nuts, and so forth that contain it.
A quick word on a third contender we didn’t include here: magnesium oxide is probably the most widely-sold magnesium supplement because it’s cheapest to make. It also has woeful bioavailability, to the point that there seems to be negligible benefit to taking it. So we don’t recommend that.
Magnesium glycinate and magnesium citrate are both absorbed well, but magnesium citrate is the most well-absorbed form of magnesium supplement.
In terms of the relative merits of the glycine or the citric acid (the “other part” of magnesium glycinate and magnesium citrate, respectively), both are also great nutrients, but the amount delivered with the magnesium is quite small in each case, and so there’s nothing here to swing it one way or the other.
For this reason, we went with the magnesium citrate, as the most readily bioavailable!
Want to try them out?
Here they are on Amazon:
Magnesium glycinate | Magnesium citrate
Enjoy!
Share This Post
-
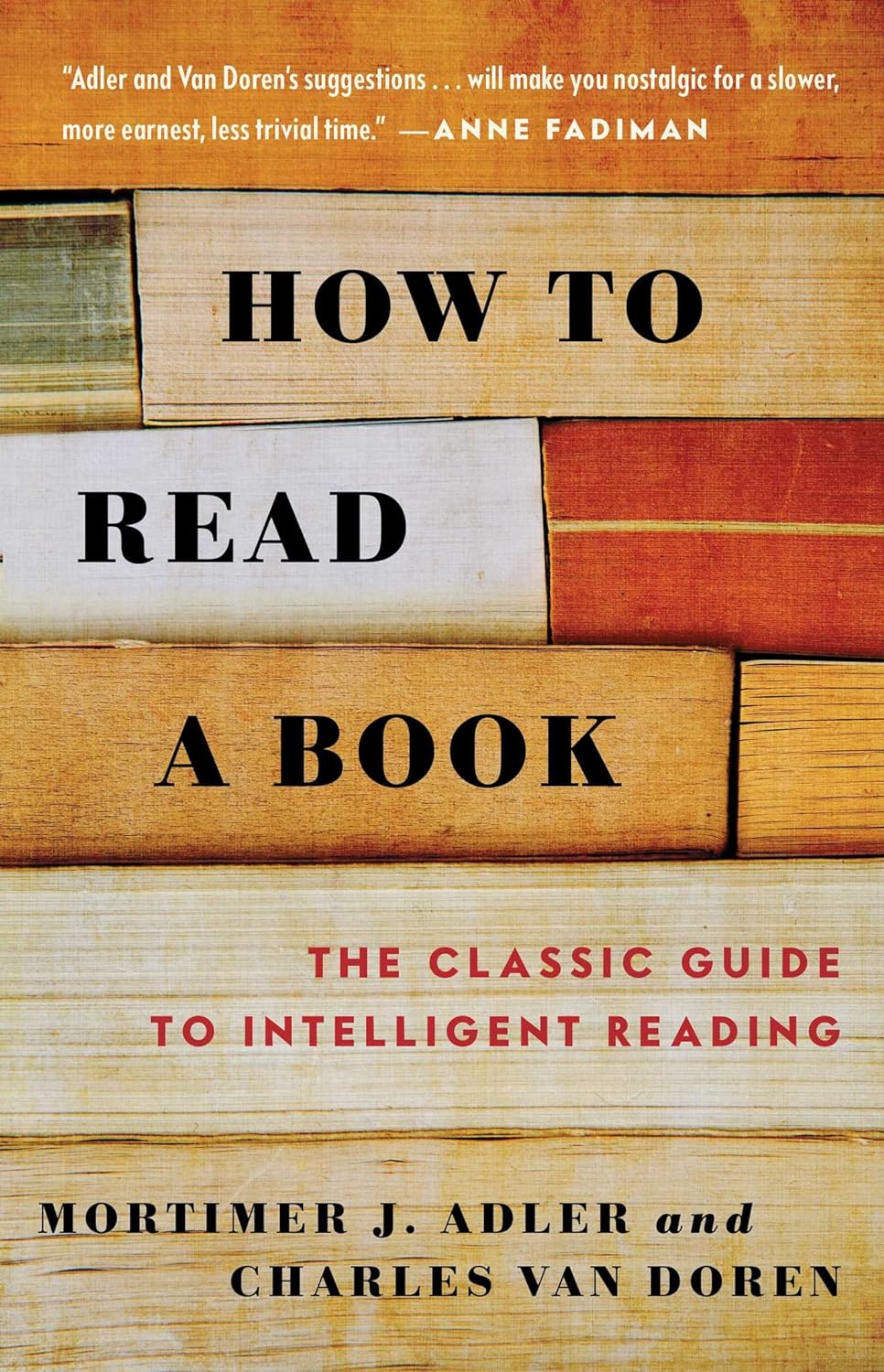
How to Read a Book – by Mortimer J. Adler and Charles Van Doren
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Are you a cover-to-cover person, or a dip-in-and-out person?
Mortimer Adler and Charles van Doren have made a science out of getting the most from reading books.
They help you find what you’re looking for (Maybe you want to find a better understanding of PCOS… maybe you want to find the definition of “heuristics”… maybe you want to find a new business strategy… maybe you want to find a romantic escape… maybe you want to find a deeper appreciation of 19th century poetry, maybe you want to find… etc).
They then help you retain what you read, and make sure that you don’t miss a trick.
Whether you read books so often that optimizing this is of huge value for you, or so rarely that when you do, you want to make it count, this book could make a real difference to your reading experience forever after.
Share This Post
-
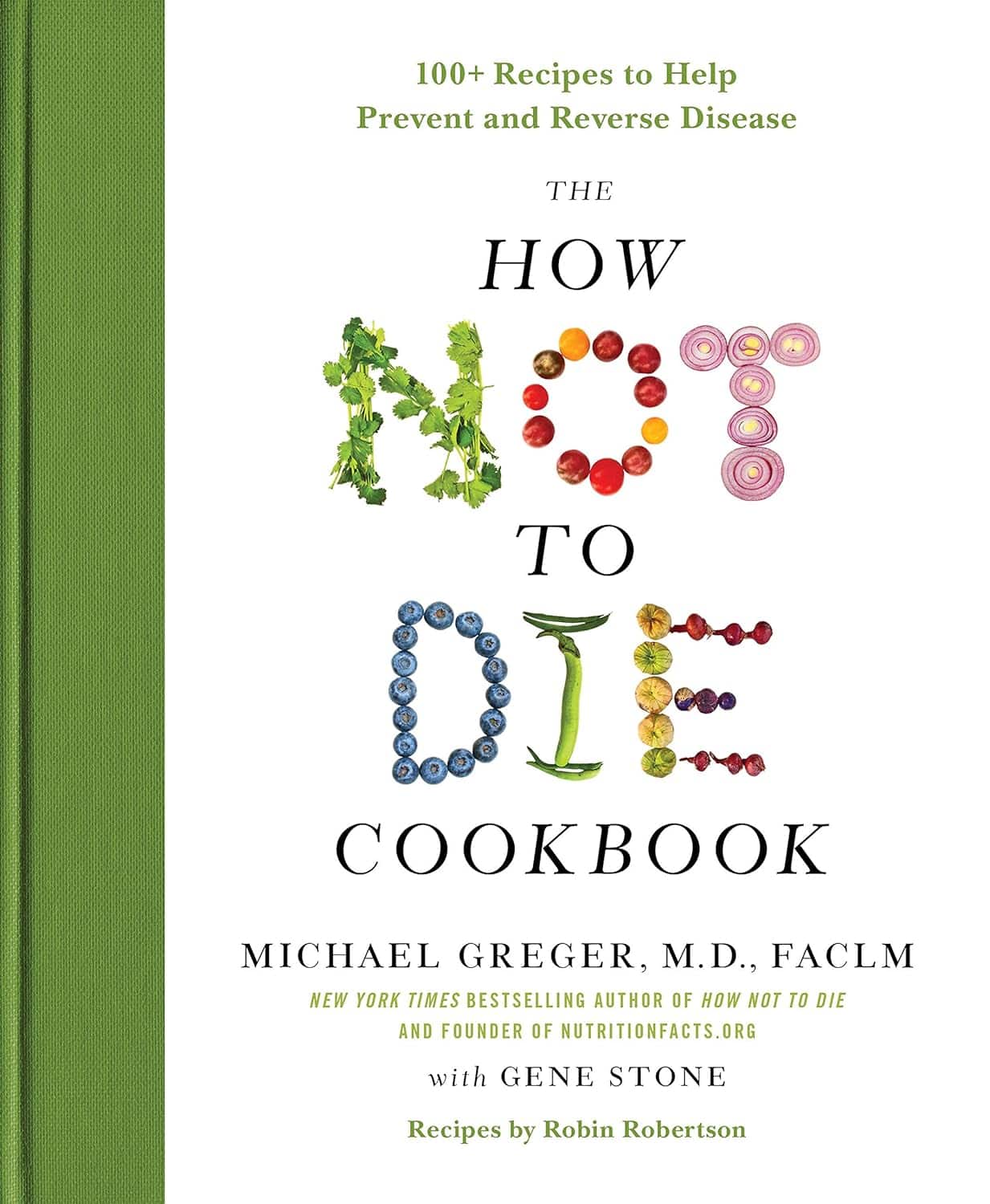
The How Not to Die Cookbook – by Dr. Michael Greger
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed Dr. Greger’s “How Not To Die”, which is excellent and/but very science-dense.
This book is different, in that the science is referenced and explained throughout, but the focus is the recipes, and how to prepare delicious healthy food in accordance with the principles laid out in How Not To Die.
It also follows “Dr Greger’s Daily Dozen“, that is to say, the 12 specific things he advises we make sure to have every day, and thus helps us to include them in an easy, no-fuss fashion.
The recipes themselves are by Robin Robertson, and/but with plenty of notes by Dr Greger; they clearly collaborated closely in creating them.
The ingredients are all things one can find in any well-stocked supermarket, so unless you live in a food desert, you can make these things easily.
And yes, the foods are delicious too.
Bottom line: if you’re interested in cooking according to perhaps the most science-based dietary system out there, then this book is a top-tier choice.
Click here to check out The How Not To Die Cookbook, and live well!
Share This Post
Related Posts
-
Blood-Sugar-Friendly Ice Pops
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This generic food product has so many regional variant names that it’s difficult to get a universal name, but in N. America they’re also known by the genericized brand name of popsicles. Anyway, they’re usually very bad news for blood sugars, being merely frozen juice even if extra sugar wasn’t added. Today’s recipe, on the other hand, makes for a refreshing and nutrient-dense treat that won’t spike your blood glucose!
You will need
- 1 cup fresh blueberries
- 1 can (12oz/400g) coconut milk
- ½ cup yogurt with minimal additives
- 1 tbsp honey (omit if you prefer less sweetness)
- Juice of ¼ lime (increase if you prefer more sourness)
Method
(we suggest you read everything at least once before doing anything)
1) Blend everything
2) Pour into ice pop molds and freeze overnight
3) Serve at your leisure:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Which Sugars Are Healthier, And Which Are Just The Same?
- 10 Ways To Balance Blood Sugars
- Can Saturated Fats Be Healthy? ← the fats in coconut are a good source of medium-chain triglycerides (MCTs), which are easily broken down as a good energy source and (enjoyed in moderation) thus unlikely to cause any cardiovascular problems, as little to nothing (usually: nothing) of it will be stored.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Emperor’s New Klotho, Or Something More?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Unzipping The Genes Of Aging?
Klotho is an enzyme encoded in humans’ genes—specifically, in the KL gene.
It’s found throughout all living parts of the human body (and can even circulate about in its hormonal form, or come to rest in its membranaceous form), and its subgroups are especially found:
- α-klotho: in the brain
- β-klotho: in the liver
- γ-klotho: in the kidneys
Great! Why do we care?
Klotho, its varieties and variants, its presence or absence, are very important in aging.
Almost every biological manifestation of aging in humans has some klotho-related indicator; usually the decrease or mutation of some kind of klotho.
Which way around the cause and effect go has been the subject of much debate and research: do we get old because we don’t have enough klotho, or do we make less klotho because we’re getting old?
Of course, everything has to be tested per variant and per system, so that can take a while (punctuated by research scientists begging for more grants to do the next one). Given that it’s about aging, testing in humans would take an incredibly long while, so most studies so far have been rodent studies.
The general gist of the results of rodent studies is “reduced klotho hastens aging; increased klotho slows it”.
(this can be known by artificially increasing or decreasing the level of klotho expression, again something easier in mice as it is harder to arrange transgenic humans for the studies)
Here’s one example of many, of that vast set of rodent studies:
Suppression of Aging in Mice by the Hormone Klotho
Relevance for Alzheimer’s, and a science-based advice
A few years ago (2020), an Alzheimer’s study was undertaken; they noted that the famous apolipoprotein E4 (apoE4) allele is the strongest genetic risk factor for Alzheimer’s, and that klotho may be another. FGF21 (secreted by the liver, mostly during fasting) binds to its own receptor (FGFR1) and its co-receptor β-klotho. Since this is a known neuroprotective factor, they wondered whether klotho itself may interact with β-amyloid (Aβ), and found:
❝Aβ can enhance the ability of klotho to draw FGF21 to regions of incipient neurodegeneration in AD❞
In other words: β-amyloid, the substance whose accumulation is associated with neurodegeneration in Alzheimer’s disease, is a mediator in klotho bringing a known neuroprotective factor, FGF21, to the areas of neurodegeneration
In fewer words: klotho calls the firefighters to the scene of the fire
Read more: Alignment of Alzheimer’s disease amyloid β-peptide and klotho
The advice based on this? Consider practicing intermittent fasting, if that is viable for you, as it will give your liver more FGF21-secreting time, and the more FGF21, the more firefighters arrive when klotho sounds the alarm.
See also: Intermittent Fasting: What’s the truth?
…and while you’re at it:
Does intermittent fasting have benefits for our brain?
A more recent (2023) study with a slightly different (but connected) purpose, found results consistent with this:
Longevity factor klotho enhances cognition in aged nonhuman primates
…and, for that matter this (2023) study that found:
Associations between klotho and telomere biology in high stress caregivers
…which looks promising, but we’d like to see it repeated with a sounder method (they sorted caregiving into “high-stress” and “low-stress” depending on whether a child was diagnosed with ASD or not, which is by no means a reliable way of sorting this). They did ask for reported subjective stress levels, but to be more objective, we’d like to see clinical markers of stress (e.g. cortisol levels, blood pressure, heart rate changes, etc).
A very recent (April 2024) study found that it has implications for more aspects of aging—and this time, in humans (but using a population-based cohort study, rather than lab conditions):
Can I get it as a supplement?
Not with today’s technology and today’s paucity of clinical trials, you can’t. Maybe in the future!
However… The presence of senescent (old, badly copied, stumbling and staggering onwards when they should have been killed and eaten and recycled already) cells actively reduces klotho levels, which means that taking supplements that are senolytic (i.e., that kill those senescent cells) can increase serum klotho levels:
Orally-active, clinically-translatable senolytics restore α-Klotho in mice and humans
Ok, what can I take for that?
We wrote about a senolytic supplement that you might enjoy, recently:
Fisetin: The Anti-Aging Assassin
Want to know more?
If you have the time, Dr. Peter Attia interviews Dr. Dena Dubal (researcher in several of the above studies) here:
Click Here If The Embedded Video Doesn’t Load Automatically
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
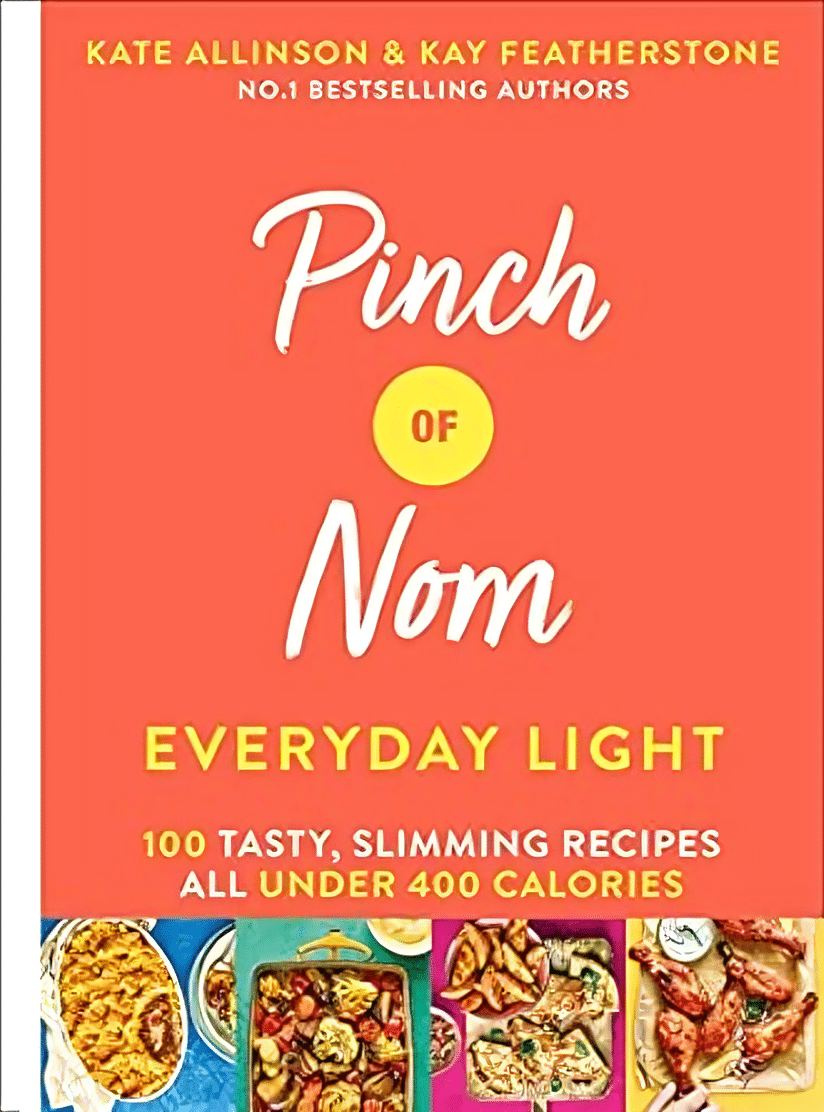
Pinch Of Nom, Everyday Light – by Kay Featherstone and Kate Allinson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One of the biggest problems with “light”, “lean” or “under this many calories” cookbooks tends to be the portion sizes perhaps had sparrows in mind. Not so, here!
Nor do they go for the other usual trick, which is giving us something that’s clearly not a complete meal. All of these recipes are for complete meals, or else come with a suggestion of a simple accompaniment that will still keep the dish under 400kcal.
The recipes are packed with vegetables and protein, perfect for keeping lean while also making sure you’re full until the next meal.
Best of all, they are indeed rich and tasty meals—there’s only so many times one wants salmon with salad, after all. There are healthy-edition junk food options, too! Sausage and egg muffins, fish and chips, pizza-loaded fries, sloppy dogs, firecracker prawns, and more!
Most of the meals are quite quick and easy to make, and use common ingredients.
Nearly half are vegetarian, and gluten-free options involve only direct simple GF substitutions. Similarly, turning a vegetarian meal into a vegan meal is usually not rocket science! Again, quick and easy substitutions, à la “or the plant-based milk of your choice”.
Recipes are presented in the format: ingredients, method, photo. Super simple (and no “chef’s nostalgic anecdote storytime” introductions that take more than, say, a sentence to tell).
All in all, a fabulous addition to anyone’s home kitchen!
Get your copy of “Pinch of Nom—Everyday Light” from Amazon today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: