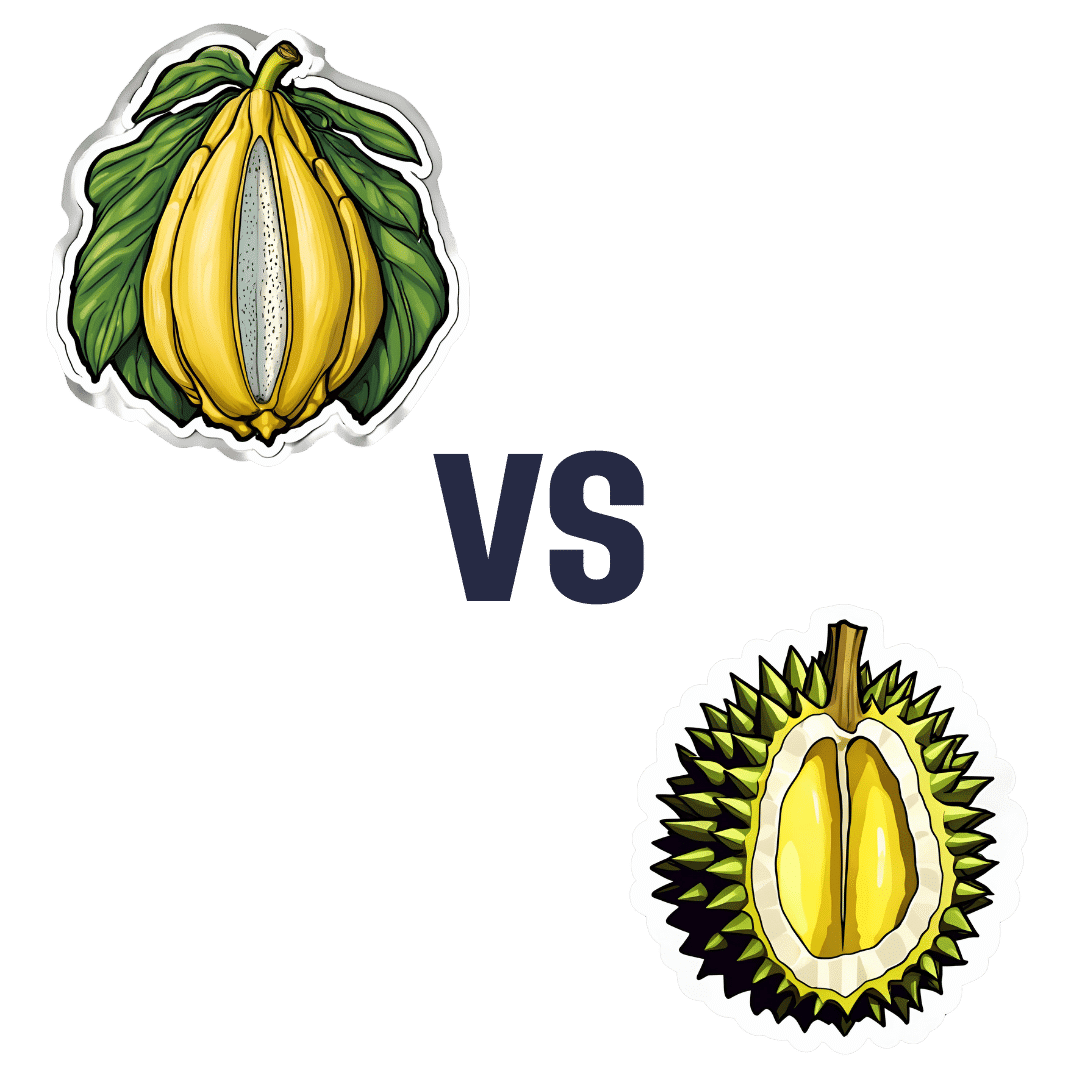
Jackfruit vs Durian – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing jackfruit to durian, we picked the durian.
Why?
Durian may look and smell like it has come directly from Hell, but there’s a lot of goodness in there!
First, let’s talk macros: jackfruit and durian are both unusually high in protein, for fruits. That said, jackfruit does have slightly more protein—but durian has more than 2x the fiber, for only slightly more carbs, so we call this section a win for durian.
Like most fruits, these two are an abundance source of vitamins; jackfruit has more of vitamins A and E, while durian has more of vitamins B1, B2, B3, B9, and C. Another win for durian.
When it comes to minerals, jackfruit has more calcium, while durian has more copper, iron, manganese, phosphorus, and zinc. We don’t usually measure this one as there’s not much in most foods (unless added in artificially), but durian is also high in sulfur, specifically in “volatile sulfur compounds”, which account for some of its smell, and are—notwithstanding the alarming name—harmless. In any case, mineral content is another win for durian.
These three things add up to one big win for durian.
There is one thing to watch out for, though: durian inhibits aldehyde dehydrogenase, which the body uses to metabolize alcohol. So, we recommend you don’t drink-and-durian, as it can increase the risk of alcohol poisoning, and even if alcohol consumption is moderate, it’ll simply stay in your system for longer, doing more damage while it’s there. Of course, it is best to simply avoid drinking alcohol regardless, durian or no durian, but the above is good to know for those who do imbibe.
A final word on durians: if you haven’t had it before, or had it and it was terrible, then know: much like a banana or an avocado, durian has a rather brief “ideal ripeness” phase for eating. It should be of moderate firmness; neither tough nor squishy. It should not have discolored spikes, nor should it have little holes in, nor be leaking fluid, and it should not smell of sweat and vinegar, although it should smell like sulfurous eggs, onions, and cheese. Basically, if it smells like a cheese-and-onion omelette made in Hell, it’s probably good. If it smells like something that died and then was kept warm in someone’s armpit for a day, it’s probably not. The best way to have a good first experience with a durian is to enjoy one with someone who knows and enjoys durians, as they will be able to pick one that’s right, and will know if it’s not (durian-sellers may not necessarily have your best interests at heart, and may seek to palm off over-ripe durians on people who don’t know better).
Enjoy!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Easing Election Stress & Anxiety
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At the time of writing, the US is about to have a presidential election. Most of our readers are Americans, and in any case, what the US does tends to affect most of the world, so certainly many readers in other countries will be experiencing stress and anxiety about it too.
We’re a health science publication, not a political outlet, so we’ll refrain from commenting on any candidates or campaign policies, and we’d also like to be clear we are not urging you to any particular action politically—our focus today is simply about mental health.
First, CBT what can be CBT’d
Cognitive Behavioral Therapy (CBT) is far from a panacea, but it’s often a very good starting point. And when it seems the stakes are high, it’s easy to fall into such cognitive distortions as “crystal ball” and “catastrophization”, that is to say, predicting the future and feeling the impact of that (probably undesired version of the) future, and also feeling like it will be the end of the world.
Recognizing these processes and how they work, is the first step to managing our feelings about them.
Learn more: The Art of Being Unflappable (Tricks For Daily Life)
Next, DBT what can be DBT’d
A lot of CBT hinges on the assumption that our assumptions are incorrect. For example, that our friend does not secretly despise us, that our spouse is not about to leave us, that the symptoms we are experiencing are not cancer, and in this case, that the election outcome will not go badly, and if it does, the consequences will be less severe than imagined.
But… What if our concerns are, in fact, fully justified? Here’s where Dialectic Behavior Therapy (DBT) comes in, and with it, what therapists call “radical acceptance”.
In other words, we accept up front the idea that maybe it’s going to be terrible and that will truly suck, and then either:
- there’s nothing we can reasonably do about it now (so worrying just means you’ll suffer twice), or
- there is something we can reasonably do about it now (so we can go do that thing)
After doing the thing (if appropriate), defer processing the outcome of the election until after the election. There is no point in wasting energy to worry before then. In a broadly two-party system where things are usually close between those two largest parties, there’s something close to a 50% chance of an outcome that’s, at least, not the worst you feared.
Learn more: CBT, DBT, & Radical Acceptance
Lastly, empower yourself with Behavioral Activation (BA)
Whatever the outcome of any given election, the world will keep turning, and the individual battles about any given law or policy or such will continue to go on. That’s not to say an election won’t change things—it will—but there will always still be stuff to do on a grassroots level to make the world a better place, no matter what politician has been elected.
Being involved in doing things on a community level will not only help banish any feelings of despair (and if you got the election outcome you wanted, it’ll help you feel involved), but also, it can give you a sense of control, and can even form a part of the “ikigai” that is often talked about as one of the pillars of healthy longevity.
Learn more: What’s Your Ikigai?
And if you like videos, then enjoy this one (narrated by the ever soothing-voiced Alain de Botton):
Watch now: How To Escape From A Despairing Mood (4:46) ← it also has a text version if you prefer that
Take care!
Share This Post
-
Canned Tuna vs Canned Sardines – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing canned tuna to canned sardines, we picked the sardines.
Why?
This comparison is unfair, but practical—because both are sold next to each other in the supermarket and often used for similar things.
It’s unfair because in a can of tuna, there is tuna meat, whereas in a can of sardines, there is sardine meat, skin, and bones.
Consequently, sardines outperform tuna in almost everything, because a lot of nutrients are in the skin and bones.
To be completely unambiguous:
Sardines have more vitamins and minerals by far (special shout-out to calcium, of which sardines contain 6000% more), and more choline (which is sometimes reckoned as a vitamin, sometimes not).
Tuna does have marginally more protein, and less fat. If you are trying to limit your cholesterol intake, then that could be an argument for choosing tuna over sardines.
All in all: the sardines are more nutrient dense by far, are good sources of vitamins and minerals that tuna contains less of (and in many cases only trace amounts of), and for most people this will more than offset the difference in cholesterol, especially if having not more than one can per day.
About that skin and bones…
That’s where the real benefit for your joints lies, by the way!
See: We Are Such Stuff As Fish Are Made Of
Enjoy!
Share This Post
-
11 Things That Can Change Your Eye Color
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Eye color is generally considered so static that iris scans are considered a reasonable security method. However, it can indeed change—mostly for reasons you won’t want, though:
Ringing the changes
Putting aside any wishes of being a manga protagonist with violet eyes, here are the self-changing options:
- Aging in babies: babies are often born with lighter eyes, which can darken as melanocytes develop during the first few months of life. This is similar to how a small child’s blonde hair can often be much darker by the time puberty hits!
- Aging in adults: eyes may continue to darken until adulthood, while aging into the elderly years can cause them to lighten due to conditions like arcus senilis
- Horner’s syndrome: a nerve disorder that can cause the eyes to become lighter due to loss of pigment
- Fuchs heterochromic iridocyclitis: an inflammation of the iris that leads to lighter eyes over time
- Pigment dispersion syndrome: the iris rubs against eye fibers, leading to pigment loss and lighter eyes
- Kayser-Fleischer rings: excess copper deposits on the cornea, often due to Wilson’s disease, causing larger-than-usual brown or grayish rings around the iris
- Iris melanoma: a rare cancer that can darken the iris, often presenting as brown spots
- Cancer treatments: chemotherapy for retinoblastoma in children can result in lighter eye color and heterochromia
- Medications: prostaglandin-based glaucoma treatments can darken the iris, with up to 23% of patients seeing this effect
- Vitiligo: an autoimmune disorder that destroys melanocytes, mostly noticed in the skin, but also causing patchy loss of pigment in the iris
- Emotional and pupil size changes: emotions and trauma can affect pupil size, making eyes appear darker or lighter temporarily by altering how much of the iris is visible
For more about all these, and some notes about more voluntary changes (if you have certain kinds of eye surgery), enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Understanding And Slowing The Progression Of Cataracts
Take care!
Share This Post
Related Posts
-
Ruminating vs Processing
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to traumatic experiences, there are two common pieces of advice for being able to move forwards functionally:
- Process whatever thoughts and feelings you need to process
- Do not ruminate
The latter can seem, at first glance, a lot like the former. So, how to tell them apart, and how to do one without the other?
Getting tense
One major difference between the two is the tense in which our mental activity takes place:
- processing starts with the traumatic event (or perhaps even the events leading up to the traumatic event), analyses what happened and if possible why, and then asks the question “ok, what now?” and begins work on laying out a path for the future.
- rumination starts with the traumatic event (or perhaps even the events leading up to the traumatic event), analyses what happened and if why, oh why oh why, “I was such an idiot, if only I had…” and gets trapped in a fairly tight (and destructive*) cycle of blame and shame/anger, never straying far from the events in question.
*this may be directly self-destructive, but it can also sometimes be only indirectly self-destructive, for example if the blame and anger is consciously placed with someone else.
This idea fits in, by the way, with Dr. Elisabeth Kübler-Ross’s “five stages of grief” model; rumination here represents the stages “bargaining”, “despair”, and “anger”, while emotional processing here represents the stage “acceptance”. Thus, it may be that rumination does have a place in the overall process—just don’t get stuck there!
For more on healthily processing grief specifically:
What Grief Does To The Body (And How To Manage It)
Grief, by the way, can be about more than the loss of a loved one; a very similar process can play out with many other kinds of unwanted life changes too.
What are the results?
Another way to tell them apart is to look at the results of each. If you come out of a long rumination session feeling worse than when you started, it’s highly unlikely that you just stopped too soon and were on the verge of some great breakthrough. It’s possible! But not likely.
- Processing may be uncomfortable at first, and if it’s something you’ve ignored for a long time, that could be very uncomfortable at first, but there should quite soon be some “light at the end of the tunnel”. Perhaps not even because a solution seems near, but because your mind and body recognize “aha, we are doing something about it now, and thus may find a better way forward”.
- Rumination tends to intensify and prolong uncomfortable emotions, increases stress and anxiety, and likely disrupts sleep. At best, it may serve as a tipping point to seek therapy or even just recognize “I should figure out a way to deal with this, because this isn’t doing me any good”. At worst, it may serve as a tipping point to depression, and/or substance abuse, and/or suicidality.
See also: How To Stay Alive (When You Really Don’t Want To) ← which also has a link back to our article on managing depression, by the way!
Did you choose it, really?
A third way to tell them apart is the level of conscious decision that went into doing it.
- Processing is almost always something that one decides “ok, let’s figure this out”, and sits down to figure it out.
- Rumination tends to be about as voluntary as social media doomscrolling. Technically we may have decided to begin it (we also might not have made any conscious decision, and just acted on impulse), but let’s face it, our hands weren’t at the wheel for long, at all.
A good way to make sure that it is a conscious process, is to schedule time for it in advance, and then do it only during that time. If thoughts about it come up at other times, tell yourself “no, leave that for later”, and then deal with it when (and only when) the planned timeslot arrives.
It’s up to you and your schedule what time you pick, but if you’re unsure, consider an hour in the early evening. That means that the business of the day is behind you, but it’s also not right before bed, so you should have some decompression time as a buffer. So for example, perhaps after dinner you might set a timer* for an hour, and sit down to journal, brainstorm, or just plain think, about the matter that needs processing.
*electronic timers can be quite jarring, and may distract you while waiting for the beeps. So, consider investing in a relaxing sand timer like this one instead.
Is there any way to make rumination less bad?
As we mentioned up top, there’s a case to be made for “rumination is an early part of the process that gets us where we need to go, and may not be skippable, or may not be advisable to skip”.
So, if you are going to ruminate, then firstly, we recommend again bordering it timewise (with a timer as above) and having a plan to pull yourself out when you’re done rather than getting stuck there (such as: The Off-Button For Your Brain: How To Stop Negative Thought Spirals).
And secondly, you might want to consider the following technique, which allows one to let one’s brain know that the thing we’re thinking about / imagining is now to be filed away safely; not lost or erased, but sent to the same place that nightmares go after we wake up:
A Surprisingly Powerful Tool: Eye Movement Desensitization & Reprocessing (EMDR)
What if I actually do want to forget?
That’s not usually recommendable; consider talking it through with a therapist first. However, for your interest, there is a way:
The Dark Side Of Memory (And How To Forget)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Secret To Better Squats: Foot, Knee, & Ankle Mobility
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve talked before about how Slav squats, Asian squats, deep squats, sitting squats, or various other things they might by called (these are all different names for the same thing), are one of the most anti-aging exercises, if not outright the most anti-aging exercise. Yet, how to get good at them?
“Just squat more” is fine advice and will get you there eventually, but there are ways to shorten the time it takes, by unlocking whatever part(s) might be holding you back:
Piece by piece
The key to improving the whole is to not neglect any of the parts—so here they are:
- Foot rolls: roll your foot onto its outer and inner edges to stretch; repeat for both legs.
- Toe lifts: lift your toes up and down while keeping your legs straight.
- Toe curls: curl your toes to engage foot muscles.
- Foot circles: rotate your feet in circles; repeat for both legs.
- Heel raises: stand tall, raise your heels off the ground, and engage your core.
- Tibialis anterior exercise: lean against a wall or similar, and lift your toes off ground to strengthen your tibialis anterior (important and oft-forgotten muscle, responsible for more than people think!)
- Heel drops: perform dynamic heel drops with your feet back, to stretch your ankles.
- Hamstring curls & leg extension: curl your leg back toward your glutes, and then extend it forwards; alternate legs.
- Dynamic calf stretch: bend and straighten your knees alternately in a forward lunge position.
- Squat to heel raise: perform squats with your heels lifting off the floor and your arms raised.
- Banded ankle dorsiflexion: use a yoga strap or towel to stretch your feet, calves, and hamstrings.
- Seated feet circles: extend your legs and rotate your feet in outward and inward circles.
- Dorsiflexion/plantar flexion: alternate one foot up and the other down dynamically.
- Seated knee flexion & extension: alternate lifting your knees and extending your legs, while seated.
Note: “seated” in all cases means on the floor, not a chair!
For more on all of these plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
What Nobody Teaches You About Strengthening Your Knees ← about that tibialis anterior muscle and what it means for your knees
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
5 Minute Posture Improvement Routine!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
McKay Lang walks us through it:
Step by Step
Breathing exercise:
- Place your hands on your lower abdomen.
- Take three deep breaths, focusing on body tension in the shoulders and neck… And release.
Shoulder squeeze:
- With your hands on your hips, inhale and squeeze your shoulders upwards.
- Hold your breath for 3–4 seconds, then exhale.
- Repeat two more times, holding the squeeze a little longer each time.
Upper shoulder massage:
- Massage your upper shoulder muscles to release tension stored there.
Overhead arm stretch:
- Raise your arms above your head, clasping each elbow with the opposite hand.
- Inhale deeply, stretch upwards, then exhale and release.
- Repeat, alternating elbows.
Neck and head push:
- Place your palms on the back of the head, and push your head into your hands (and vice versa, because of Newton’s Third Law of Motion).
- Do the same sideways (one side and then the other), to engage the other neck muscles.
Cool down:
- Gently unclasp your hands, bring your head upright, and massage your muscles. And breathe.
For variations and a visual demonstration of all, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
6 Ways To Look After Your Back
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: