I’ve recovered from a cold but I still have a hoarse voice. What should I do?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cold, flu, COVID and RSV have been circulating across Australia this winter. Many of us have caught and recovered from one of these common upper respiratory tract infections.
But for some people their impact is ongoing. Even if your throat isn’t sore anymore, your voice may still be hoarse or croaky.
So what happens to the voice when we get a virus? And what happens after?
Here’s what you should know if your voice is still hoarse for days – or even weeks – after your other symptoms have resolved.
Why does my voice get croaky during a cold?
A healthy voice is normally clear and strong. It’s powered by the lungs, which push air past the vocal cords to make them vibrate. These vibrations are amplified in the throat and mouth, creating the voice we hear.
The vocal cords are two elastic muscles situated in your throat, around the level of your laryngeal prominence, or Adam’s apple. (Although everyone has one, it tends to be more pronounced in males.) The vocal cords are small and delicate – around the size of your fingernail. Any small change in their structure will affect how the voice sounds.
When the vocal cords become inflamed – known as laryngitis – your voice will sound different. Laryngitis is a common part of upper respiratory tract infections, but can also be caused through misuse.
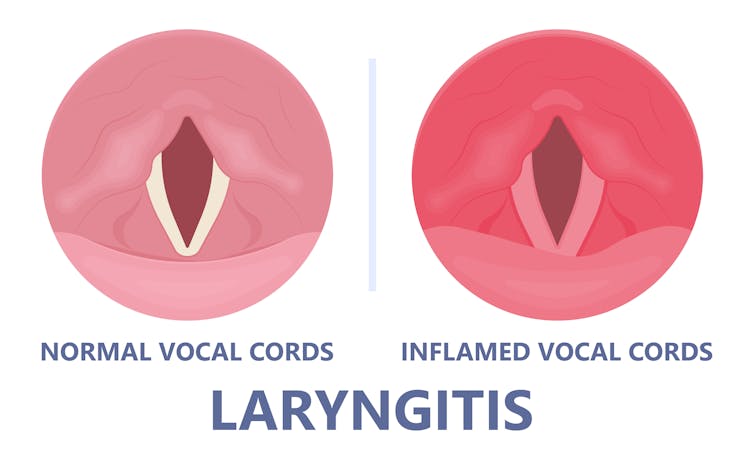
Catching a virus triggers the body’s defence mechanisms. White blood cells are recruited to kill the virus and heal the tissues in the vocal cords. They become inflamed, but also stiffer. It’s harder for them to vibrate, so the voice comes out hoarse and croaky.
In some instances, you may find it hard to speak in a loud voice or have a reduced pitch range, meaning you can’t go as high or loud as normal. You may even “lose” your voice altogether.
Coughing can also make things worse. It is the body’s way of trying to clear the airways of irritation, including your own mucus dripping onto your throat (post-nasal drip). But coughing slams the vocal cords together with force.
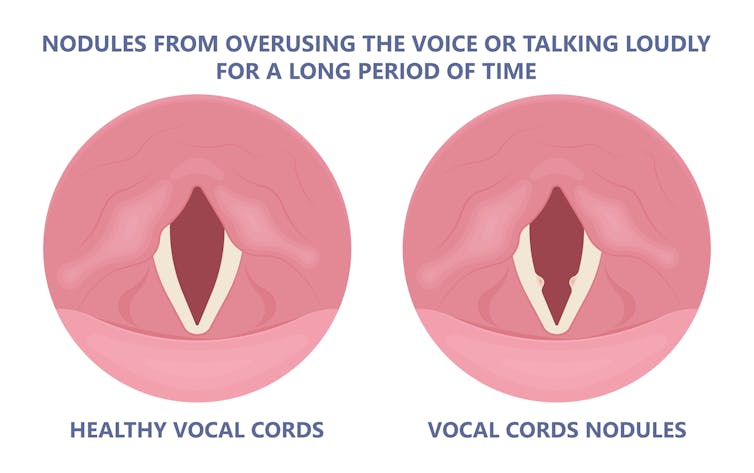
Chronic coughing can lead to persistent inflammation and even thicken the vocal cords. This thickening is the body trying to protect itself, similar to developing a callus when a pair of new shoes rubs.
Thickening on your vocal cords can lead to physical changes in the vocal cords – such as developing a growth or “nodule” – and further deterioration of your voice quality.
How can you care for your voice during infection?
People who use their voices a lot professionally – such as teachers, call centre workers and singers – are often desperate to resume their vocal activities. They are more at risk of forcing their voice before it’s ready.
The good news is most viral infections resolve themselves. Your voice is usually restored within five to ten days of recovering from a cold.
Occasionally, your pharmacist or doctor may prescribe cough suppressants to limit additional damage to the vocal cords (among other reasons) or mucolytics, which break down mucus. But the most effective treatments for viral upper respiratory tract infections are hydration and rest.
Drink plenty of water, avoid alcohol and exposure to cigarette smoke. Inhaling steam by making yourself a cup of hot water will also help clear blocked noses and hydrate your vocal cords.
Rest your voice by talking as little as possible. If you do need to talk, don’t whisper – this strains the muscles.
Instead, consider using “confidential voice”. This is a soft voice – not a whisper – that gently vibrates your vocal cords but puts less strain on your voice than normal speech. Think of the voice you use when communicating with someone close by.
During the first five to ten days of your infection, it is important not to push through. Exerting the voice by talking a lot or loudly will only exacerbate the situation. Once you’ve recovered from your cold, you can speak as you would normally.
What should you do if your voice is still hoarse after recovery?
If your voice hasn’t returned to normal after two to three weeks, you should seek medical attention from your doctor, who may refer you to an ear nose and throat specialist.
If you’ve developed a nodule, the specialist would likely refer you to a speech pathologist who will show you how to take care of your voice. Many nodules can be treated with voice therapy and don’t require surgery.
You may have also developed a habit of straining your vocal cords, if you forced yourself to speak or sing while they were inflamed. This can be a reason why some people continue to have a hoarse voice even when they’ve recovered from the cold.
In those cases, a speech pathologist may play a valuable role. They may teach you to exercises that make voicing more efficient. For example, lip trills (blowing raspberries) are a fun and easy way you can learn to relax the voice. This can help break the habit of straining your voice you may have developed during infection.
Yeptain Leung, Postdoctoral Research and Lecturer of Speech Pathology, School of Health Sciences, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Think Again – by Adam Grant
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Warning: this book may cause some feelings of self-doubt! Ride them out and see where they go, though.
It was Socrates who famously (allegedly) said “ἓν οἶδα ὅτι οὐδὲν οἶδα”—”I know that I know nothing”.
Adam Grant wants us to take this philosophy and apply it usefully to modern life. How?
The main premise is that rethinking our plans, answers and decisions is a good thing… Not a weakness. In contrast, he says, a fixed mindset closes us to opportunities—and better alternatives.
He wants us to be sure that we don’t fall into the trap of the Dunning-Kruger Effect (overestimating our abilities because of being unaware of how little we know), but he also wants us to rethink whole strategies, too. For example:
Grant’s approach to interpersonal conflict is very remniscent of another book we might review sometime, “Aikido in Everyday Life“. The idea here is to not give in to our knee-jerk responses to simply retaliate in kind, but rather to sidestep, pivot, redirect. This is, admittedly, the kind of “rethinking” that one usually has to rethink in advance—it’s too late in the moment! Hence the value of a book.
Nor is the book unduly subjective. “Wishy-washiness” has a bad rep, but Grant gives us plenty in the way of data and examples of how we can, for example, avoid losses by not doubling down on a mistake.
What, then, of strongly-held core principles? Rethinking doesn’t mean we must change our mind—it simply means being open to the possibility in contexts where such makes sense.
Grant borrows, in effect, from:
❝Do the best you can until you know better. Then when you know better… do better!❞
So, not so much undercutting the principles we hold dear, and instead rather making sure they stand on firm foundations.
All in all, a thought-provokingly inspiring read!
Share This Post
-
Gut Renovation – by Dr. Roshini Raj, with Sheila Buff
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Unless we actually feel something going on down there, gut health is an oft-neglected part of overall health—which is unfortunate, because invisible as it may often be, it affects so much.
Gastroenterologist Dr. Roshini Raj gives us all the need-to-know information, explanations of why things happen the way they do with regard to the gut, and tips, tricks, and hacks to improve matters.
She also does some mythbusting along the way, and advises about what things don’t make a huge difference, including what medications don’t have a lot of evidence for their usefulness.
The style is easy-reading pop-science, with plenty of high-quality medical content.
Reading between the lines, a lot of the book as it stands was probably written by the co-author, Sheila Buff, who is a professional ghostwriter and specializes in working closely with doctors to produce works that are readable and informative to the layperson while still being full of the doctor’s knowledge and expertise. So a reasonable scenario is that Dr. Raj gave her extensive notes, she took it from there, passed it back to her for medical corrections, and they had a little back and forth until it was done. Whatever their setup, the end result was definitely good!
Bottom line: if you’d like a guide to gut health that’s practical and easy to read, while being quite comprehensive and certainly a lot more than “eat probiotics and fiber”, then this book is a fine choice.
Share This Post
-
‘I can’t quite shut it off’: Prevalence of insomnia a growing concern for women
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Tasha Werner, 43, gets up at 3:30 a.m. twice a week for her part-time job at a fitness centre in Calgary. After a five-hour shift, she is back home by 9 a.m. to homeschool her two children, aged 9 and 12. The hardest part of her position – stay-at-home mom, homeschool teacher and part-time worker – is the downtime “lost from my life,” says Werner.
A study by Howard M. Kravitz, a psychiatrist in Chicago, showed that up to 60 per cent of women experience sleep disorders due to hormonal changes linked to menopause. But there is an increasing prevalence of insomnia symptoms in women that may be attributed, in part, to societal changes.
“We live in a world that didn’t exist a generation ago. Now everyone is trying to figure it out,” says Michael Grandner, director of the Sleep and Health Research Program at the University of Arizona.
While women are no longer expected to stay at home, many who are employed outside the home also have the primary responsibility for family matters. And women aged 40 to 60 commonly fall within the “sandwich generation,” caring for both children and parents.
As women juggle their responsibilities, these duties can take a toll, both emotionally and practically.
Both Werner and her husband were raised in traditional homes; their mothers stayed at home to oversee childcare, cooking, grocery shopping and household duties. Initially, Werner and her husband followed a similar path, mirroring their parents’ lives as homemakers. “I think we just fell into what we were used to,” says Werner.
However, a notable shift in their family dynamics occurred once she started working outside the home.
Her children’s physical needs and illnesses have had major consequences on her sleep. If one of the children is sick with the flu, that’s “a week of not a lot of sleep during the night,” she says, “because that’s my job.” Many nights, she finds herself waking up between 1 a.m. and 3 a.m., worrying about how the kids are doing academically or behaviourally.
“We face a specific set of anxieties and a different set of pressures than men,” says Emma Kobil, who has been a therapist in Denver, Colo., for 15 years and is now an insomnia coach. There is so much pressure to be everything as a woman – to be an amazing homemaker and worker while maintaining a hot-rocking body and having a cool personality, to “be the cool mom but also the CEO, to follow your dreams and be the boss b****,” says Kobil.
And there’s an appeal to that concept. Daughters grow up viewing their moms as superwomen juggling responsibilities. But what isn’t always obvious are the challenges women face while managing their lives and the health issues they may encounter.
A study revealed that women are 41 per cent more at risk of insomnia than men.
A thorough study revealed that women are 41 per cent more at risk of insomnia than men. Beyond menopausal hormonal shifts, societal pressures, maternal concerns and the challenge of balancing multiple roles contribute to women’s increased susceptibility to insomnia.
Cyndi Aarrestad, 57, lives on a farm in Saskatchewan with her husband, Denis. Now an empty nester, Aarrestad fills her time working on the farm, keeping house, volunteering at her church and managing her small woodworking business. And she struggles with sleep.
Despite implementing some remedies, including stretching, drinking calming teas and rubbing her feet before bed, Aarrestad says achieving restful sleep has remained elusive for the past decade.
Two primary factors contribute to her sleep challenges — her inability to quiet her mind and hormonal hot flashes due to menopause. Faced with family and outside commitments, Aarrestad finds it challenging to escape night time’s mental chatter. “It’s a mom thing for me … I can’t quite shut it off.” Even as her children transitioned to young adulthood and moved out, the worries persisted, highlighting the lasting concerns moms have about their kids’ jobs, relationships and overall well-being.
Therapist Kobil says that every woman she’s ever worked with experiences this pressure to do everything, to be perfect. These women feel like they’re not measuring up. They’re encouraged to take on other people’s burdens; to be the confidante and the saviour in many ways; to sacrifice themselves. Sleep disruptions simply reflect the consequences of this pressure.
“They’re trying to fit 20 hours in a 24-hour day, and it doesn’t work,” says Grandner, the sleep specialist.
Grandner says that consistently sleeping six hours or less as an adult makes one 55 per cent more likely to become obese, 20 per cent more likely to develop high blood pressure, and 30 per cent more likely to develop Type 2 diabetes if you didn’t have it already. This lack of sleep makes you more likely to catch the flu. It makes vaccines less effective, and it increases your likelihood of developing depression and anxiety.
When is the time to change? Yesterday. Grandner warns that the sleep sacrifices made at a young age impact health later. But it’s never too late to make changes, he says, and “you do the best with what you’ve got.”
Kobil suggests a practical approach for women struggling with sleep. She emphasizes understanding that sleeplessness isn’t a threat and encourages a shift in mindset about being awake. Instead of fighting sleeplessness, she advises treating oneself kindly, recognizing the difficulty.
Kobil recommends creating a simple playbook with comforting activities for awake moments during the night. Just as you would comfort a child who’s afraid, she suggests being gentle with yourself, gradually changing the perception of wakefulness into a positive experience.
This article is republished from HealthyDebate under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
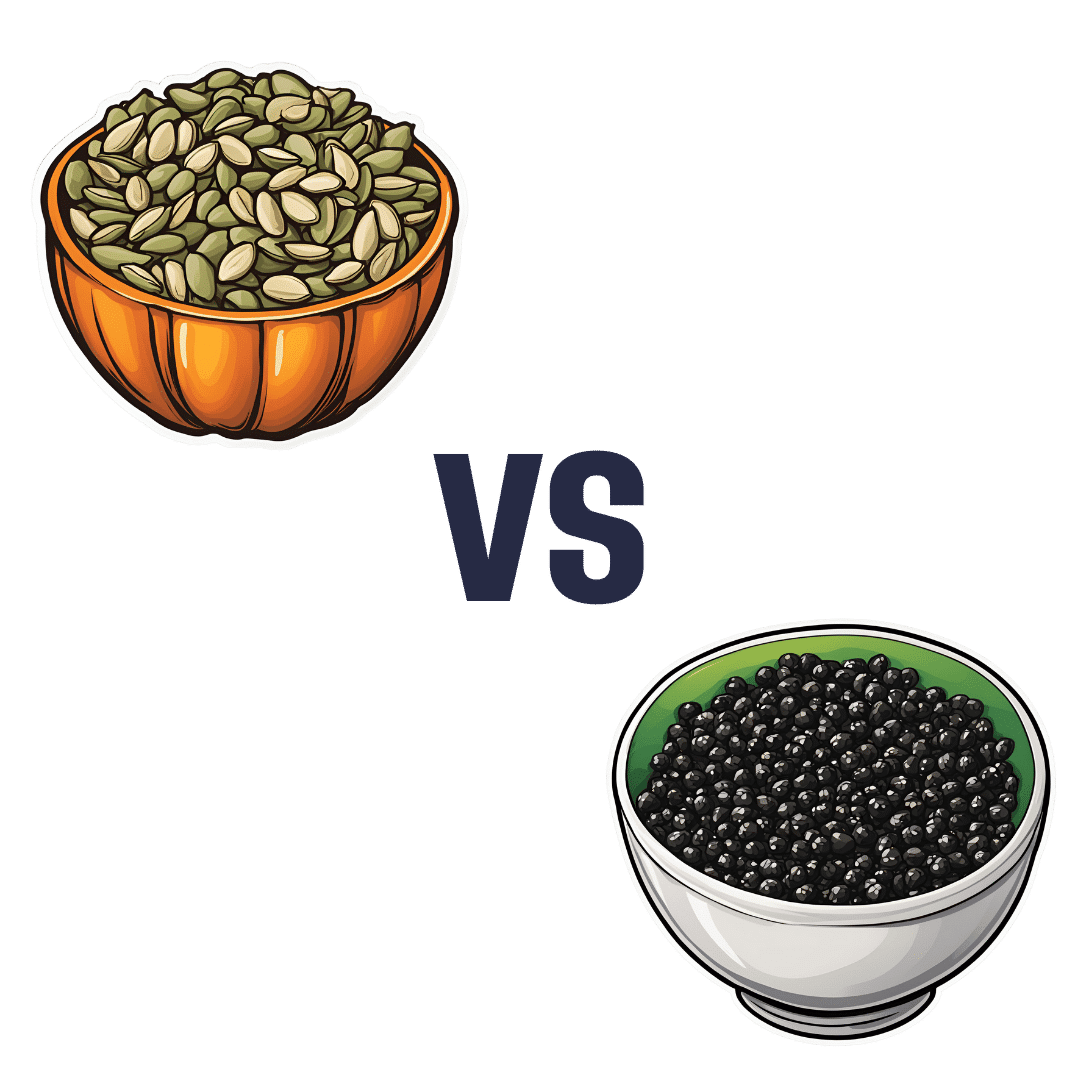
Pumpkin Seeds vs Watermelon Seeds – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pumpkin seeds to watermelon seeds, we picked the watermelon.
Why?
Starting with the macros: pumpkin seeds have a lot more carbs, while watermelon seeds have a lot more protein, despite pumpkin seeds being famous for such. They’re about equal on fiber. In terms of fats, watermelon seeds are higher in fats, and yes, these are healthy fats, mostly polyunsaturated.
When it comes to vitamins, pumpkin seeds are marginally higher in vitamins A and C, while watermelon seeds are a lot higher in vitamins B1, B2, B3, B5, B6, and B9. An easy win for watermelon seeds here.
In the category of minerals, despite being famous for zinc, pumpkin seeds are higher only in potassium, while watermelon seeds are higher in iron, magnesium, manganese, and phosphorus; the two seeds are equal on calcium, copper, and zinc. Another win for watermelon seeds.
In short, enjoy both, but watermelon has more to offer. Of course, if buying just the seeds and not the whole fruit, it’s generally easier to find pumpkin seeds than watermelon seeds, so do bear in mind that pumpkin seeds’ second place isn’t that bad here—it’s just a case of a very nutritious food looking bad by standing next to an even better one.
Want to learn more?
You might like to read:
Seed Saving Secrets – by Alice Mirren
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Progesterone Menopausal HRT: When, Why, And How To Benefit
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Progesterone doesn’t get talked about as much as other sex hormones, so what’s its deal? Dr. Heather Hirsch explains:
Menopausal progesterone
Dr. Hirsch considers progesterone essential for menopausal women who are taking estrogen and have an intact uterus, to keep conditions at bay such as endometriosis or even uterine cancer.
However, she advises it is not critical in those without a uterus, unless there was a previous case of one of the above conditions.
10almonds addition: on the other hand, progesterone can still be beneficial from a metabolic and body composition standpoint, so do speak with your endocrinologist about it.
As an extra bonus: while not soporific (it won’t make you sleepy), taking progesterone at night will improve the quality of your sleep once you do sleep, so that’s a worthwhile thing for many!
Dr. Hirsch also discusses the merits of continuous vs cyclic use; continuous maintains the above sleep benefits, for example, while cyclic use can help stabilize menstrual patterns in late perimenopause and early menopause.
For more on these things, plus discussion of different types of progesterone, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- What Does “Balance Your Hormones” Even Mean?
- What You Should Have Been Told About The Menopause Beforehand
- HRT: Bioidentical vs Animal – A Tale Of Two Approaches
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
World Menopause Day Health News Round-Up
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In order to provide variety in this week’s round-up, not all of this is menopause-related, but it is all important:
Menopause & CVD
Untreated menopause is associated with higher incidence of heart disease, and higher mortality. People often forget about how much estrogen does for us (well, for those of us with a physiology running on estrogen, anyway; gentlemen, your testosterone is fine for you), and think it is “just” a sex hormone, but it’s a lot more.
Read in full: Menopause transition linked to increased heart disease risk
Related: What Menopause Does To The Heart
Extraterrestrial medical technology
The much lower gravity in Earth orbit has allowed for tissue engineering techniques that Earth’s normal gravity imposes limitations on. This is big news, because it means that rather than replacing a whole liver, tissue implants could be grafted, allowing the extant liver to repair itself (something livers are famously good at, but they need enough undamaged base material to work with).
Read in full: How liver tissue from the International Space Station may transform tissue engineering
Related: How To Unfatty A Fatty Liver
One thing and then another
As if endometriosis weren’t unpleasant enough in and of itself, the endothelial dysfunction inherent to it also raises cardiovascular disease risk. This is important, because while endometriosis has (like many maladies predominantly affecting women) generally been shrugged off by the medical world as an unhappy inconvenience but not life-threatening, now we know it comes with extra existential risks too:
Read in full: Understanding cardiovascular risks in endometriosis patients
Related: What You Need To Know About Endometriosis
Push-button meditation
Unlike mindfulness meditation, listening to music is a very passive experience, and thus requires less effort from the user. And yet, it has been associated with lower perceived pain levels, lower self-reported anxiety levels, less opioid use, and measurably lower heart-rate.
Read in full: Listening to music may speed up recovery from surgery, research suggests
Related: Nobody Likes Surgery, But Here’s How To Make It Much Less Bad
Cholesterol in menopause: quality over quantity
Much like previous research has shown that the quantity of LDL is not nearly so predictive of health outcomes in women as it is in men, this study into HDL and menopausal women shows that quantity of HDL does not matter nearly so much as the quality of it.
Read in full: HDL quality, not quantity, contribute to the first sign of Alzheimer’s disease in women
Related: Statins: His & Hers? ← consistent with the above, statins (to lower LDL cholesterol) generally help more for men and produce more adverse side effects for women. So again, a case of “the actual amount of cholesterol isn’t so important for women as for men”.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: