I want to eat healthily. So why do I crave sugar, salt and carbs?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We all want to eat healthily, especially as we reset our health goals at the start of a new year. But sometimes these plans are sabotaged by powerful cravings for sweet, salty or carb-heavy foods.
So why do you crave these foods when you’re trying to improve your diet or lose weight? And what can you do about it?
There are many reasons for craving specific foods, but let’s focus on four common ones:
1. Blood sugar crashes
Sugar is a key energy source for all animals, and its taste is one of the most basic sensory experiences. Even without specific sweet taste receptors on the tongue, a strong preference for sugar can develop, indicating a mechanism beyond taste alone.
Neurons responding to sugar are activated when sugar is delivered to the gut. This can increase appetite and make you want to consume more. Giving into cravings also drives an appetite for more sugar.
In the long term, research suggests a high-sugar diet can affect mood, digestion and inflammation in the gut.
While there’s a lot of variation between individuals, regularly eating sugary and high-carb foods can lead to rapid spikes and crashes in blood sugar levels. When your blood sugar drops, your body can respond by craving quick sources of energy, often in the form of sugar and carbs because these deliver the fastest, most easily accessible form of energy.
2. Drops in dopamine and serotonin
Certain neurotransmitters, such as dopamine, are involved in the reward and pleasure centres of the brain. Eating sugary and carb-rich foods can trigger the release of dopamine, creating a pleasurable experience and reinforcing the craving.
Serotonin, the feel-good hormone, suppresses appetite. Natural changes in serotonin can influence daily fluctuations in mood, energy levels and attention. It’s also associated with eating more carb-rich snacks in the afternoon.

Marcus Aurelius/Pexels
Low carb diets may reduce serotonin and lower mood. However, a recent systematic review suggests little association between these diets and risk for anxiety and depression.
Compared to men, women tend to crave more carb rich foods. Feeling irritable, tired, depressed or experiencing carb cravings are part of premenstrual symptoms and could be linked to reduced serotonin levels.
3. Loss of fluids and drops in blood sugar and salt
Sometimes our bodies crave the things they’re missing, such as hydration or even salt. A low-carb diet, for example, depletes insulin levels, decreasing sodium and water retention.
Very low-carb diets, like ketogenic diets, induce “ketosis”, a metabolic state where the body switches to using fat as its primary energy source, moving away from the usual dependence on carbohydrates.
Ketosis is often associated with increased urine production, further contributing to potential fluid loss, electrolyte imbalances and salt cravings.
4. High levels of stress or emotional turmoil
Stress, boredom and emotional turmoil can lead to cravings for comfort foods. This is because stress-related hormones can impact our appetite, satiety (feeling full) and food preferences.
The stress hormone cortisol, in particular, can drive cravings for sweet comfort foods.
A 2001 study of 59 premenopausal women subjected to stress revealed that the stress led to higher calorie consumption.
A more recent study found chronic stress, when paired with high-calorie diet, increases food intake and a preference for sweet foods. This shows the importance of a healthy diet during stress to prevent weight gain.
What can you do about cravings?
Here are four tips to curb cravings:
1) don’t cut out whole food groups. Aim for a well-balanced diet and make sure you include:
- sufficient protein in your meals to help you feel full and reduce the urge to snack on sugary and carb-rich foods. Older adults should aim for 20–40g protein per meal with a particular focus on breakfast and lunch and an overall daily protein intake of at least 0.8g per kg of body weight for muscle health
- fibre-rich foods, such as vegetables and whole grains. These make you feel full and stabilise your blood sugar levels. Examples include broccoli, quinoa, brown rice, oats, beans, lentils and bran cereals. Substitute refined carbs high in sugar like processed snack bars, soft drink or baked goods for more complex ones like whole grain bread or wholewheat muffins, or nut and seed bars or energy bites made with chia seeds and oats
2) manage your stress levels. Practise stress-reduction techniques like meditation, deep breathing, or yoga to manage emotional triggers for cravings. Practising mindful eating, by eating slowly and tuning into bodily sensations, can also reduce daily calorie intake and curb cravings and stress-driven eating
3) get enough sleep. Aim for seven to eight hours of quality sleep per night, with a minimum of seven hours. Lack of sleep can disrupt hormones that regulate hunger and cravings
4) control your portions. If you decide to indulge in a treat, control your portion size to avoid overindulging.
Overcoming cravings for sugar, salt and carbs when trying to eat healthily or lose weight is undoubtedly a formidable challenge. Remember, it’s a journey, and setbacks may occur. Be patient with yourself – your success is not defined by occasional cravings but by your ability to manage and overcome them.
Hayley O’Neill, Assistant Professor, Faculty of Health Sciences and Medicine, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
More research shows COVID-19 vaccines are safe for young adults
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What you need to know
- Myocarditis, or inflammation of the heart muscle, is most commonly caused by a viral infection like COVID-19, not by vaccination.
- In line with previous research, a recent CDC study found no association between COVID-19 vaccination and sudden cardiac death in previously healthy young people.
- A COVID-19 infection is much more likely to cause inflammation of the heart muscle than a COVID-19 vaccine, and those cases are typically more severe.
Since the approval of the first COVID-19 vaccines, anti-vaccine advocates have raised concerns about heart muscle inflammation, also called myocarditis, after vaccination to suggest that vaccines are unsafe. They’ve also used concerns about myocarditis to spread false claims that vaccines cause sudden deaths, which is not true.
Research has consistently shown that cases of myocarditis after vaccination are extremely rare and usually mild, and a new study from the CDC found no association between sudden cardiac death and COVID-19 vaccination in young adults.
Read on to learn more about myocarditis and what the latest research says about COVID-19 vaccine safety.
What is myocarditis?
Myocarditis is inflammation of the myocardium, or the middle muscular layer of the heart wall. This inflammation weakens the heart’s ability to pump blood. Symptoms may include fatigue, shortness of breath, chest pain, rapid or irregular heartbeat, and flu-like symptoms.
Myocarditis may resolve on its own. In rare cases, it may lead to stroke, heart failure, heart attack, or death.
What causes myocarditis?
Myocarditis is typically caused by a viral infection like COVID-19. Bacteria, parasites, fungi, chemicals, and certain medications can also cause myocarditis.
In very rare cases, some people develop myocarditis after receiving a COVID-19 vaccine, but these cases are usually mild and resolve on their own. In contrast, a COVID-19 infection is much more likely to cause myocarditis, and those cases are typically more severe.
Staying up to date on vaccines reduces your risk of developing myocarditis from a COVID-19 infection.
Are COVID-19 vaccines safe for young people?
Yes. COVID-19 vaccines have been rigorously tested and monitored over the past three years and have been determined to be safe for everyone 6 months and older. A recent CDC study found no association between COVID-19 vaccination and sudden cardiac death in previously healthy young adults.
The benefits of vaccination outweigh any potential risks. Staying up to date on COVID-19 vaccines reduces your risk of severe illness, hospitalization, death, long COVID, and COVID-19-related complications, such as myocarditis.
The CDC recommends people 65 and older and immunocompromised people receive an additional dose of the updated COVID-19 vaccine this spring—if at least four months have passed since they received a COVID-19 vaccine.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Share This Post
-
Cancer is increasingly survivable – but it shouldn’t depend on your ability to ‘wrangle’ the health system
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One in three of us will develop cancer at some point in our lives. But survival rates have improved to the point that two-thirds of those diagnosed live more than five years.
This extraordinary shift over the past few decades introduces new challenges. A large and growing proportion of people diagnosed with cancer are living with it, rather than dying of it.
In our recently published research we examined the cancer experiences of 81 New Zealanders (23 Māori and 58 non-Māori).
We found survivorship not only entailed managing the disease, but also “wrangling” a complex health system.
Surviving disease or surviving the system
Our research focused on those who had lived longer than expected (four to 32 years since first diagnosis) with a life-limiting or terminal diagnosis of cancer.
Common to many survivors’ stories was the effort it took to wrangle the system or find others to advocate on their behalf, even to get a formal diagnosis and treatment.
By wrangling we refer to the practices required to traverse complex and sometimes unwelcoming systems. This is an often unnoticed but very real struggle that comes on top of managing the disease itself.
The common focus of the healthcare system is on symptoms, side effects of treatment and other biological aspects of cancer. But formal and informal care often falls by the wayside, despite being key to people’s everyday experiences.
Survival is often linked to someone’s social connections and capacity to access funds. Getty Images The inequities of cancer survivorship are well known. Analyses show postcodes and socioeconomic status play a strong role in the prevalence of cancer and survival.
Less well known, but illustrated in our research, is that survival is also linked to people’s capacity to manage the entire healthcare system. That includes accessing a diagnosis or treatment, or identifying and accessing alternative treatments.
Survivorship is strongly related to material resources, social connections, and understandings of how the health system works and what is available. For instance, one participant who was contemplating travelling overseas to get surgery not available in New Zealand said:
We don’t trust the public system. So thankfully we had private health insurance […] But if we went overseas, health insurance only paid out to $30,000 and I think the surgery was going to be a couple of hundred thousand. I remember Dad saying and crying and just being like, I’ll sell my business […] we’ll all put in money. It was really amazing.
Assets of survivorship
In New Zealand, the government agency Pharmac determines which medications are subsidised. Yet many participants were advised by oncologists or others to “find ways” of taking costly, unsubsidised medicines.
This often meant finding tens of thousands of dollars with no guarantees. Some had the means, but for others it meant drawing on family savings, retirement funds or extending mortgages. This disproportionately favours those with access to assets and influences who survives.
But access to economic capital is only one advantage. People also have cultural resources – often described as cultural capital.
In one case, a participant realised a drug company was likely to apply to have a medicine approved. They asked their private oncologist to lobby on their behalf to obtain the drug through a compassionate access scheme, without having to pay for it.
Others gained community support through fundraising from clubs they belonged to. But some worried about where they would find the money, or did not want to burden their community.
I had my doctor friend and some others that wanted to do some public fundraising. But at the time I said, “Look, most of the people that will be contributing are people from my community who are poor already, so I’m not going to do that option”.
Accessing alternative therapies, almost exclusively self-funded, was another layer of inequity. Some felt forced to negotiate the black market to access substances such as marijuana to treat their cancer or alleviate the side effects of orthodox cancer treatment.
Cultural capital is not a replacement for access to assets, however. Māori survivorship was greatly assisted by accessing cultural resources, but often limited by lack of material assets.
Persistence pays
The last thing we need when faced with the possibility of cancer is to have to push for formal diagnosis and care. Yet this was a common experience.
One participant was told nothing could be found to explain their abdominal pain – only to find later they had pancreatic cancer. Another was told their concerns about breathing problems were a result of anxiety related to a prior mental health history, only to learn later their earlier breast cancer had spread to their lungs.
Persistence is another layer of wrangling and it often causes distress.
Once a diagnosis was given, for many people the public health system kicked in and delivered appropriate treatment. However, experiences were patchy and variable across New Zealand.
Issues included proximity to hospitals, varying degrees of specialisation available, and the requirement of extensive periods away from home and whānau. This reflects an ongoing unevenness and lack of fairness in the current system.
When facing a terminal or life-limiting diagnosis, the capacity to wrangle the system makes a difference. We shouldn’t have to wrangle, but facing this reality is an important first step.
We must ensure it doesn’t become a continuing form of inequity, whereby people with access to material resources and social and cultural connections can survive longer.
Kevin Dew, Professor of Sociology, Te Herenga Waka — Victoria University of Wellington; Alex Broom, Professor of Sociology & Director, Sydney Centre for Healthy Societies, University of Sydney; Chris Cunningham, Professor of Maori & Public Health, Massey University; Elizabeth Dennett, Associate Professor in Surgery, University of Otago; Kerry Chamberlain, Professor of Social and Health Psychology, Massey University, and Richard Egan, Associate Professor in Health Promotion, University of Otago
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
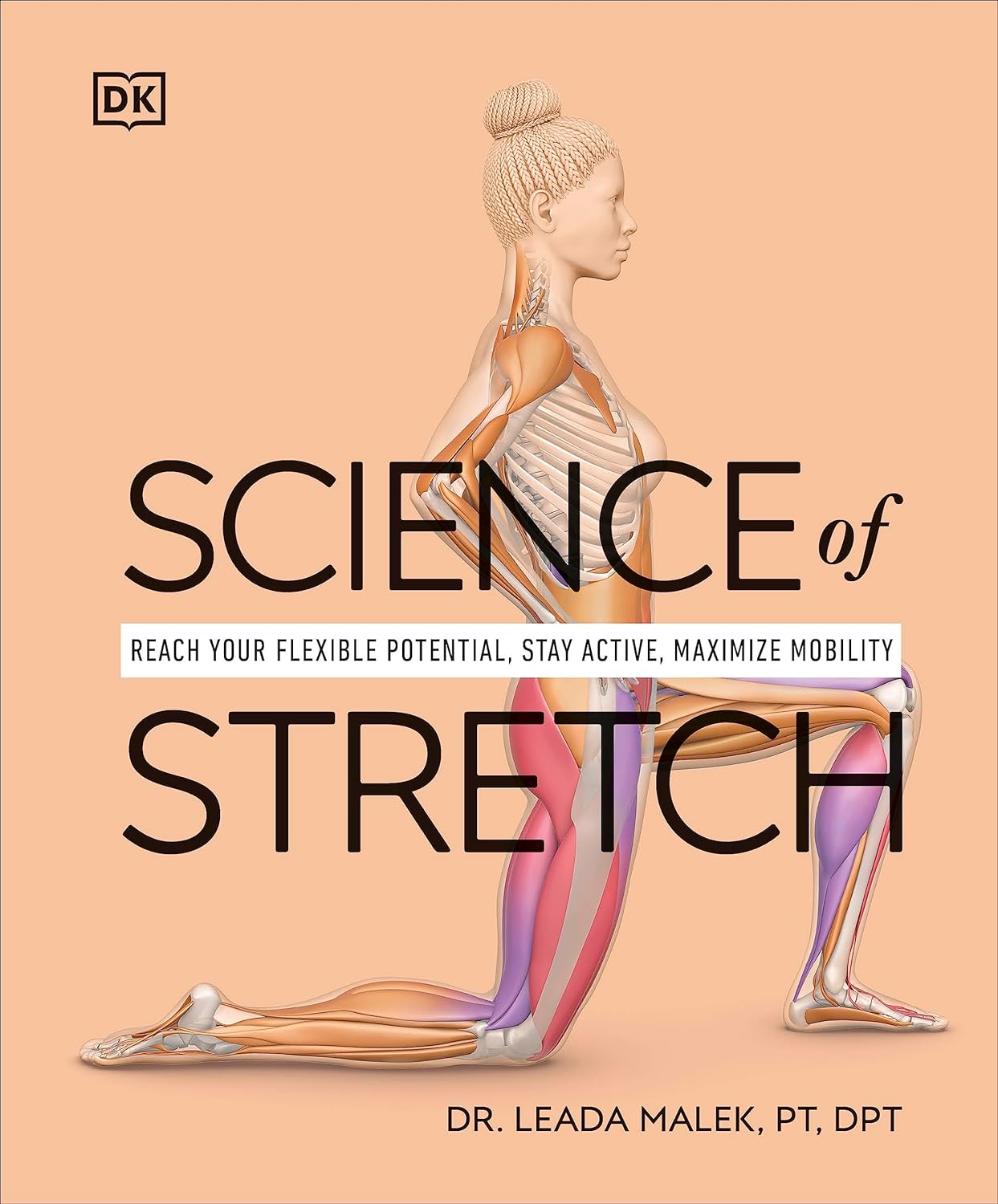
Science of Stretch – by Dr. Leada Malek
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book is part of a “Science of…” series, of which we’ve reviewed some others before (Yoga | HIIT | Pilates), and needless to say, we like them.
You may be wondering: is this just that thing where a brand releases the same content under multiple names to get more sales, and no, it’s not (long-time 10almonds readers will know: if it were, we’d say so!).
While flexibility and mobility are indeed key benefits in yoga and Pilates, they looked into the science of what was going on in yoga asanas and Pilates exercises, stretchy or otherwise, so the stretching element was not nearly so deep as in this book.
In this one, Dr. Malek takes us on a wonderful tour of (relevant) human anatomy and physiology, far deeper than most pop-science books go into when it comes to stretching, so that the reader can really understand every aspect of what’s going on in there.
This is important, because it means busting a lot of myths (instead of busting tendons and ligaments and things), understanding why certain things work and (critically!) why certain things don’t, how certain stretching practices will sabotage our progress, things like that.
It’s also beautifully clearly illustrated! The cover art is a fair representation of the illustrations inside.
Bottom line: if you want to get serious about stretching, this is a top-tier book and you won’t regret it.
Click here to check out Science of Stretching, and learn what you can do and how!
Share This Post
Related Posts
-
Capsaicin For Weight Loss And Against Inflammation
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Capsaicin’s Hot Benefits
Capsaicin, the compound in hot peppers that makes them spicy, is a chemical irritant and a neurotoxin. However, humans being humans, we decided to eat them for fun.
In contrast to many other ways in which humans recreationally enjoy things that are objectively poisonous, consuming capsaicin (in moderation) is considered to have health benefits, such as aiding weight loss (by boosting metabolism) and reducing inflammation.
Let’s see what the science says…
First: is it safe?
Capsaicin is classified as “Generally Recognized As Safe”. That said, the same mechanism that causes them to boost metabolism, does increase blood pressure:
Mechanisms underlying the hypertensive response induced by capsaicin
If you are in good cardiovascular health, this increase should be slight and not pose any threat, unless for example you enter a chili-eating contest when not acclimated to such:
Capsaicin and arterial hypertensive crisis
As ever, if unsure, do check with your doctor first, especially if you are taking any blood pressure medications, or otherwise have known blood pressure issues.
Does it really boost metabolism?
It certainly does; it works by increasing oxygen consumption and raising body temperature, both of which mean more calories will be burned for the same amount of work:
Dietary capsaicin and its anti-obesity potency: from mechanism to clinical implications
This means, of course, that chili peppers enjoy the status of being functionally a “negative calorie” food, and a top-tier one at that:
Chili pepper as a body weight-loss food
Here’s a good quality study that showed a statistically significant* fat loss improvement over placebo:
*To put it in numbers, the benefit was:
- 5.91 percentage points lower body fat percentage than placebo
- 6.68 percentage points greater change in body fat mass than placebo
See also: Difference between percentages and percentage points
For those who prefer big reviews than single studies, we’ve got you covered:
Does it really reduce inflammation?
Counterintuitive as it may seem, yes. By means of reducing oxidative stress. Given that things that reduce oxidative stress tend to reduce inflammation, and in turn tend to reduce assorted disease risks (from diabetes to cancer to Alzheimer’s), this probably has more knock-on benefits too, but we don’t have room to explore all of those today.
Fresh peppers are best for this, but dried peppers (such as when purchased as a ground spice in the supermarket, or when purchased as a capsule-based supplement) still have a very respectable anti-inflammatory effect:
- Capsaicinoids, Polyphenols and Antioxidant Activities of Capsicum annuum: Comparative Study of the Effect of Ripening Stage and Cooking Methods
- A Review on the Effect of Drying on Antioxidant Potential of Fruits and Vegetables
How much should we take?
It’s recommended to start at a low dose and gradually increase it, but 2–6mg of capsaicin per day is the standard range used in studies.
If you’re getting this from peppers, then for example cayenne pepper (a good source of capsaicin) contains around 2.5mg of capsaicin per 1 gram of cayenne.
In the case of capsules, if for example you don’t like eating hot pepper, this will usually mean taking 2–6 capsules per day, depending on dosage.
Make sure to take it with plenty of water!
Where can we get it?
Fresh peppers or ground spice from your local grocery store is fine. Your local health food store probably sells the supplements, too.
If you’d like to buy it online, here is an example product on Amazon.
Note: options on Amazon were more limited than usual, so this product is not vegan, and probably not halal or kosher, as the capsule contains an unspecified gelatin.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
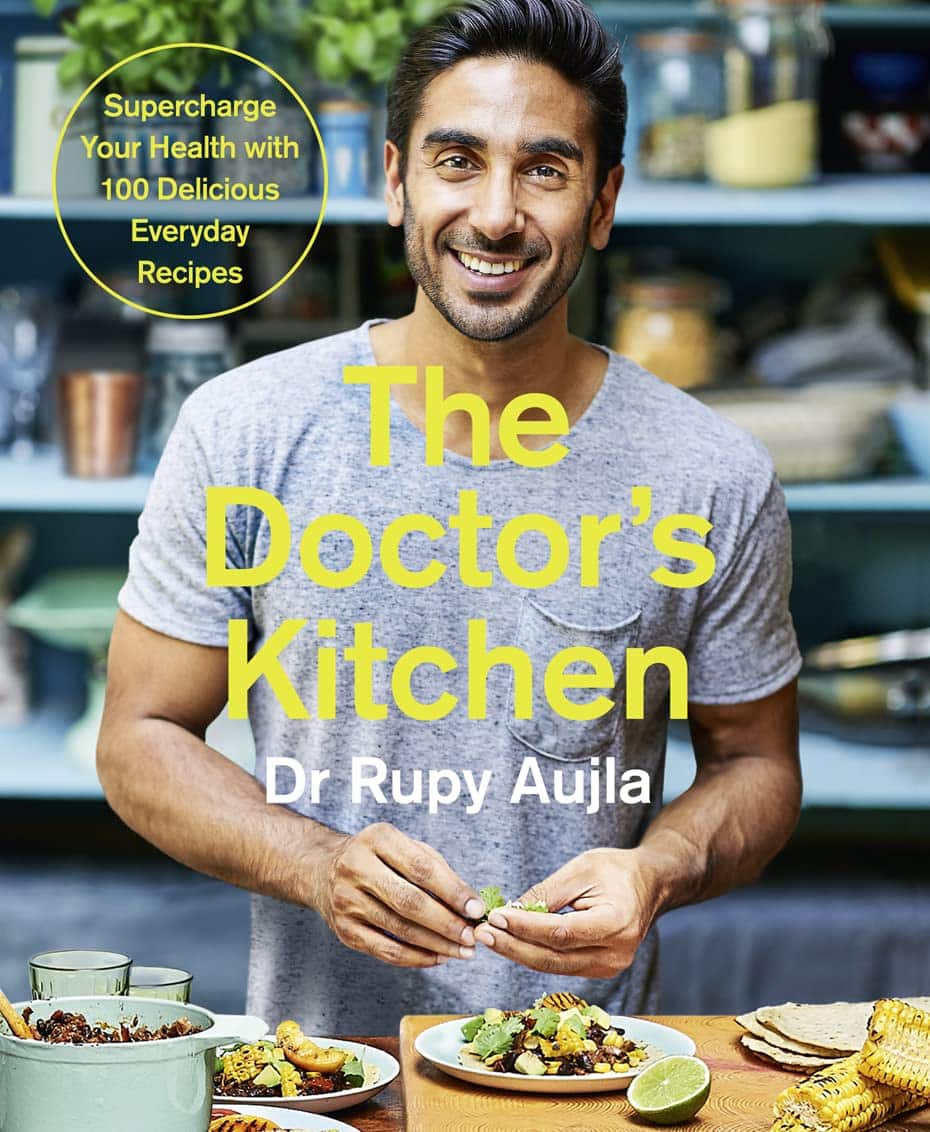
The Doctor’s Kitchen – by Dr. Rupy Aujla
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve featured Dr. Aujla before as an expert-of-the-week, and now it’s time to review a book by him. What’s his deal, and what should you expect?
Dr. Aujla first outlines the case for food as medicine. Not just “eat nutritionally balanced meals”, but literally, “here are the medicinal properties of these plants”. Think of some of the herbs and spices we’ve featured in our Monday Research Reviews, and add in medicinal properties of cancer-fighting cruciferous vegetables, bananas with dopamine and dopamine precursors, berries full of polyphenols, hemp seeds that fight cognitive decline, and so forth.
Most of the book is given over to recipes. They’re plant-centric, but mostly not vegan. They’re consistent with the Mediterranean diet, but mostly Indian. They’re economically mindful (favoring cheap ingredients where reasonable) while giving a nod to where an extra dollar will elevate the meal. They don’t give calorie values etc—this is a feature not a bug, as Dr. Aujla is of the “positive dieting” camp that advocates for us to “count colors, not calories”. Which, we have to admit, makes for very stress-free cooking, too.
Dr. Aujla is himself an Indian Brit, by the way, which gives him two intersecting factors for having a taste for spices. If you don’t share that taste, just go easier on the pepper etc.
As for the medicinal properties we mentioned up top? Four pages of references at the back, for any who are curious to look up the science of them. We at 10almonds do love references!
Bottom line: if you like tasty food and you’re looking for a one-stop, well-rounded, food-as-medicine cookbook, this one is a top-tier choice.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
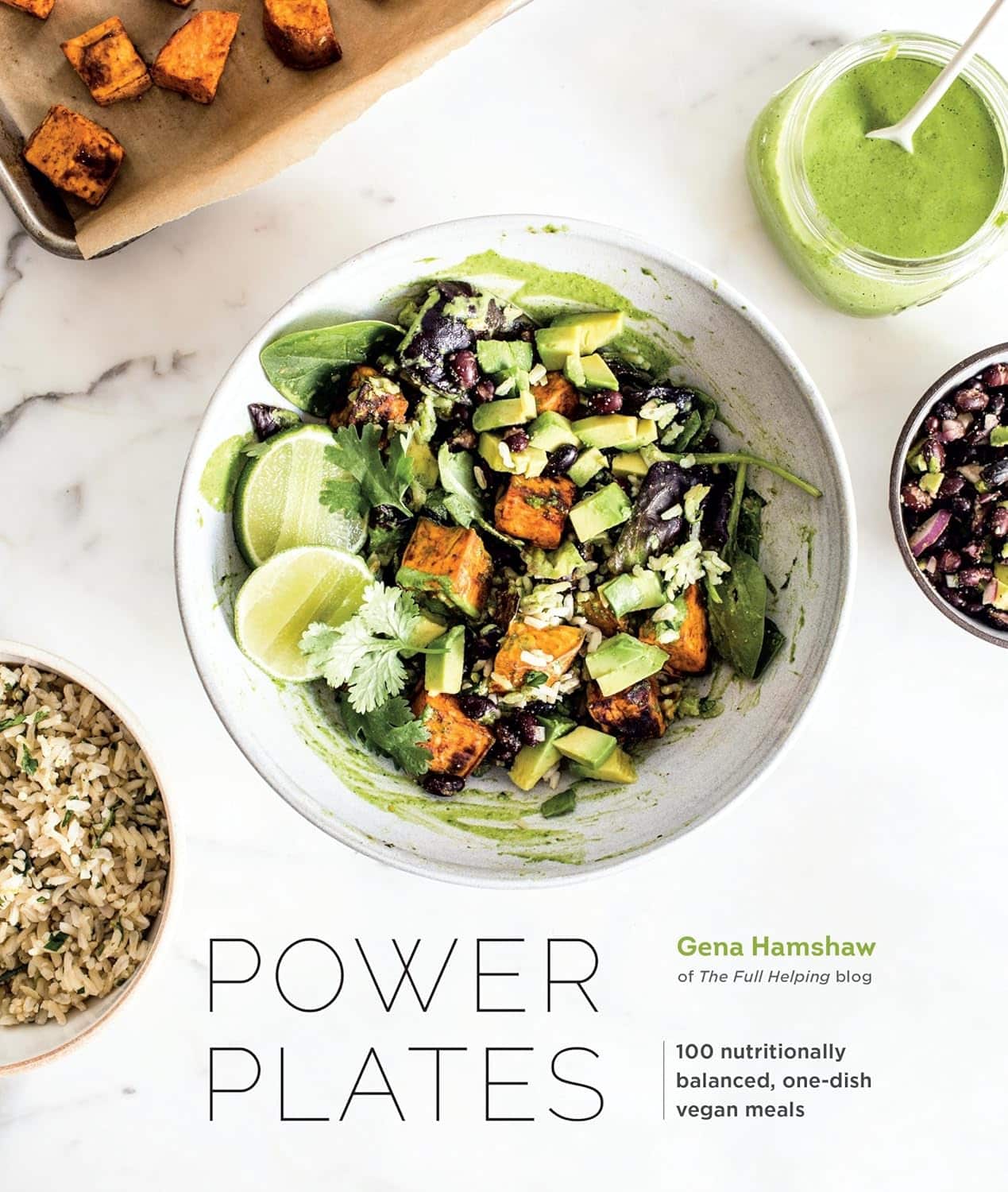
Power Plates – by Gena Hamshaw
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Superfoods are all well and good, but there are only so many ways one can reasonably include watercress before it starts becoming a chore.
Happily, Gena Hamshaw is here with a hundred single-dish vegan meals, that are not only nutritionally balanced as the subtitle promises, but also, as the title suggests, are nutritional powerhouses too.
In the category of criticism, some ingredients are not so universally available as others. For example, depending on where you live, your local supermarket might not have freekeh, gochujang, or pomegranate molasses.
However, most of the recipes have ingredients that are easy enough to source in any medium-sized supermarket, and for the ones that aren’t, we do recommend ordering the ingredient online and trying something you might not otherwise have experienced—that’s an important thing in life, after all!
Bottom line: if you’d like plant-based meals that are packed full of nutrients and are delicious too, this is a top-tier recipe book.
Click here to check out Power Plates, and enjoy a wide variety of plant-based cuisine!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: