I can’t afford olive oil. What else can I use?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you buy your olive oil in bulk, you’ve likely been in for a shock in recent weeks. Major supermarkets have been selling olive oil for up to A$65 for a four-litre tin, and up to $26 for a 750 millilitre bottle.
We’ve been hearing about the health benefits of olive oil for years. And many of us are adding it to salads, or baking and frying with it.
But during a cost-of-living crisis, these high prices can put olive oil out of reach.
Let’s take a look at why olive oil is in demand, why it’s so expensive right now, and what to do until prices come down.

Remind me, why is olive oil so good for you?
Including olive oil in your diet can reduce your risk of developing type 2 diabetes and improve heart health through more favourable blood pressure, inflammation and cholesterol levels.
This is largely because olive oil is high in monounsaturated fatty acids and polyphenols (antioxidants).
Some researchers have suggested you can get these benefits from consuming up to 20 grams a day. That’s equivalent to about five teaspoons of olive oil.
Why is olive oil so expensive right now?
A European heatwave and drought have limited Spanish and Italian producers’ ability to supply olive oil to international markets, including Australia.
This has been coupled with an unusually cold and short growing season for Australian olive oil suppliers.
The lower-than-usual production and supply of olive oil, together with heightened demand from shoppers, means prices have gone up.

How can I make my olive oil go further?
Many households buy olive oil in large quantities because it is cheaper per litre. So, if you have some still in stock, you can make it go further by:
- storing it correctly – make sure the lid is on tightly and it’s kept in a cool, dark place, such as a pantry or cabinet. If stored this way, olive oil can typically last 12–18 months
- using a spray – sprays distribute oil more evenly than pourers, using less olive oil overall. You could buy a spray bottle to fill from a large tin, as needed
- straining or freezing it – if you have leftover olive oil after frying, strain it and reuse it for other fried dishes. You could also freeze this used oil in an airtight container, then thaw and fry with it later, without affecting the oil’s taste and other characteristics. But for dressings, only use fresh oil.
I’ve run out of olive oil. What else can I use?
Here are some healthy and cheaper alternatives to olive oil:
- canola oil is a good alternative for frying. It’s relatively low in saturated fat so is generally considered healthy. Like olive oil, it is high in healthy monounsaturated fats. Cost? Up to $6 for a 750mL bottle (home brand is about half the price)
- sunflower oil is a great alternative to use on salads or for frying. It has a mild flavour that does not overwhelm other ingredients. Some studies suggest using sunflower oil may help reduce your risk of heart disease by lowering LDL (bad) cholesterol and raising HDL (good) cholesterol. Cost? Up to $6.50 for a 750mL bottle (again, home brand is about half the price)
- sesame oil has a nutty flavour. It’s good for Asian dressings, and frying. Light sesame oil is typically used as a neutral cooking oil, while the toasted type is used to flavour sauces. Sesame oil is high in antioxidants and has some anti-inflammatory properties. Sesame oil is generally sold in smaller bottles than canola or sunflower oil. Cost? Up to $5 for a 150mL bottle.

How can I use less oil, generally?
Using less oil in your cooking could keep your meals healthy. Here are some alternatives and cooking techniques:
- use alternatives for baking – unless you are making an olive oil cake, if your recipe calls for a large quantity of oil, try using an alternative such as apple sauce, Greek yoghurt or mashed banana
- use non-stick cookware – using high-quality, non-stick pots and pans reduces the need for oil when cooking, or means you don’t need oil at all
- steam instead – steam vegetables, fish and poultry to retain nutrients and moisture without adding oil
- bake or roast – potatoes, vegetables or chicken can be baked or roasted rather than fried. You can still achieve crispy textures without needing excessive oil
- grill – the natural fats in meat and vegetables can help keep ingredients moist, without using oil
- use stock – instead of sautéing vegetables in oil, try using vegetable broth or stock to add flavour
- try vinegar or citrus – use vinegar or citrus juice (such as lemon or lime) to add flavour to salads, marinades and sauces without relying on oil
- use natural moisture – use the natural moisture in ingredients such as tomatoes, onions and mushrooms to cook dishes without adding extra oil. They release moisture as they cook, helping to prevent sticking.
Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland and Emily Burch, Accredited Practising Dietitian and Lecturer, Southern Cross University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Signs Of Low Estrogen In Women: What Your Skin, Hair, & Nails Are Trying To Tell You
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Skin, hair, and nails are often thought of purely as a beauty thing, but in fact they can be indicative of a lot of other aspects of health. Dr. Andrea Suarez takes us through some of them in this video about the systemic (i.e., whole-body, not just related to sex things) effects of estrogen, and/or a deficiency thereof.
Beyond the cosmetic
Low estrogen levels are usual in women during and after untreated menopause, resulting in various changes in the skin, hair, and nails, that reflect deeper issues, down to bone health, heart health, brain health, and more. Since we can’t see our bones or hearts or brains without scans (or a serious accident/incident), we’re going to focus on the outward signs of estrogen deficiency.
Estrogen helps maintain healthy collagen production, skin elasticity, wound healing, and moisture retention, making it essential for youthful and resilient skin. Declining estrogen levels with menopause lead to a thinner epidermis, decreased collagen production, and more pronounced wrinkles. Skin elasticity also diminishes, which slows the skin’s ability to recover from stretching or deformation. Wound healing also becomes slower, increasing the risk of infections and extended recovery periods after injuries or surgeries—bearing in mind that collagen is needed in everything from our skin to our internal connective tissue (fascia) and joints and bones. So all those things are going to struggle to recover from injury (and surgery is also an injury) without it.
Other visible changes associated with declining estrogen include significant dryness as a result of reduced hyaluronic acid and glycosaminoglycan production, which are essential for moisture retention. The skin becomes more prone to irritation and increased water loss. Additionally, estrogen deficiency results in less resistance to oxidative stress, making the skin more susceptible to damage from environmental factors such as UV radiation and pollution, as well as any from-the-inside pollution that some may have depending on diet and lifestyle.
Acne and enlarged pores are associated with increased testosterone, but testosterone and estrogen are antagonistic in most ways, and in this case a decrease in estrogen will do the same, due increased unopposed androgen signaling affecting the oil glands. The loss of supportive collagen also causes the skin around pores to lose structure, making them appear larger. The reduction in skin hydration further exacerbates the visibility of pores and can contribute to the development of blackheads due to abnormal cell turnover.
Blood vessel issues tend to arise as estrogen levels drop, leading to a reduction in angiogenesis, i.e. the formation and integrity of blood vessels. This results in more fragile and leaky blood vessels, making the skin more prone to bruising, especially on areas frequently exposed to the sun, such as the backs of the hands. This weakened vasculature also further contributes to the slower wound healing that we talked about, due to less efficient delivery of growth factors.
Hair and nail changes often accompany estrogen deficiency. Women may notice hair thinning, increased breakage, and a greater likelihood of androgenic alopecia. The texture of the hair can change, becoming more brittle. Similarly, nails can develop ridges, split more easily, and become more fragile due to reduced collagen and keratin production, which also affects the skin around the nails.
As for what to do about it? Management options for estrogen-deficient skin include:
- Bioidentical hormone replacement therapy (HRT), which can improve skin elasticity, boost collagen production, and reduce dryness and fragility, as well as addressing the many more serious internal things that are caused by the same deficiency as these outward signs.
- Low-dose topical estrogen cream, which can help alleviate skin dryness and increase skin strength, won’t give the systemic benefits (incl. to bones, heart, brain, etc) that only systemic HRT can yield.
- Plant-based phytoestrogens, which are not well-evidenced, but may be better than nothing if nothing is your only other option. However, if you are taking anything other form of estrogen, don’t use phytoestrogens as well, or they will compete for estrogen receptors, and do the job not nearly so well while impeding the bioidentical estrogen from doing its much better job.
And for all at any age, sunscreen continues to be one of the best things to put on one’s skin for general skin health, and this is even more true if running low on estrogen.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
These Signs Often Mean These Nutrient Deficiencies (Do You Have Any?)
Take care!
Share This Post
-
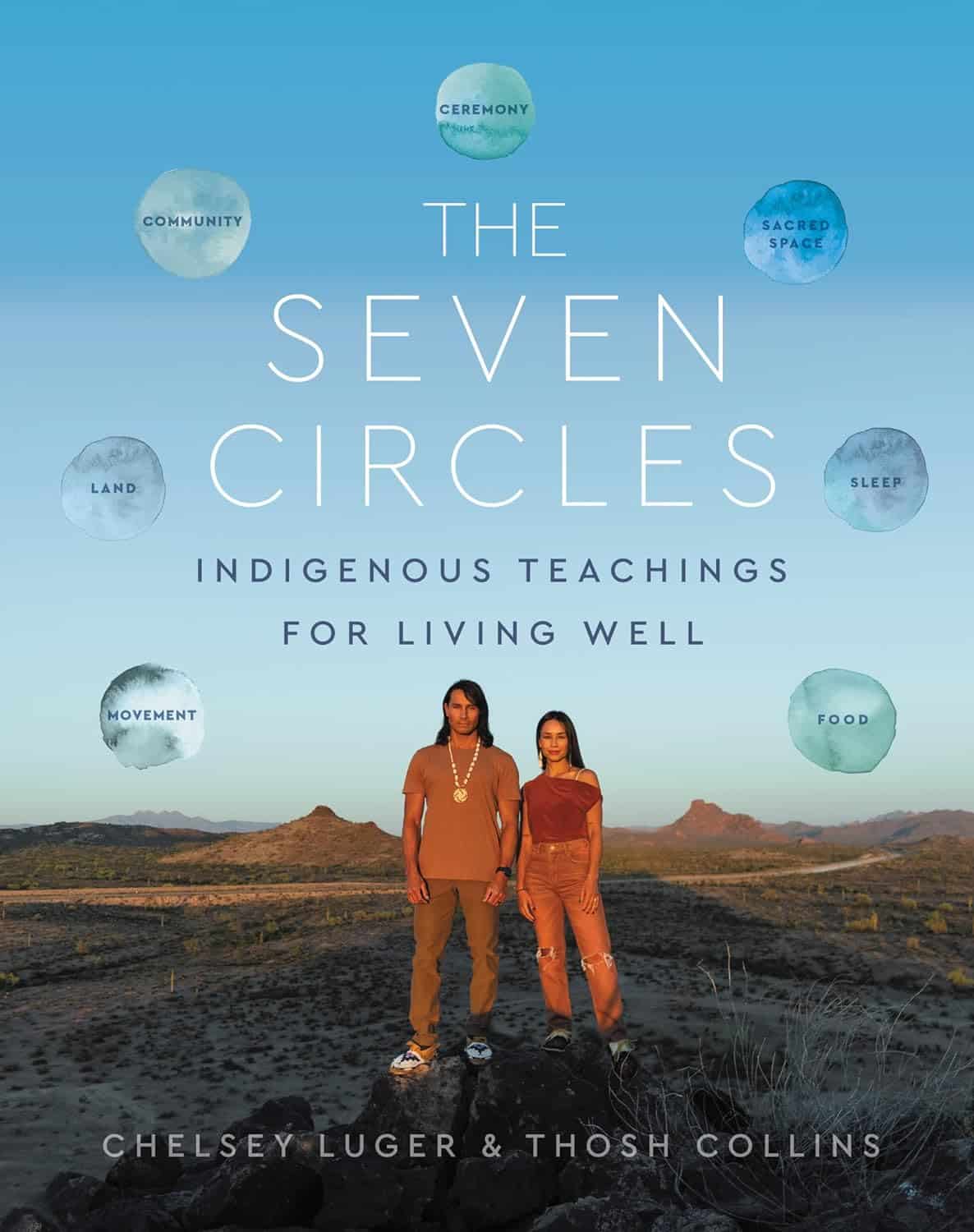
The Seven Circles – by Chelsey Luger & Thosh Collins
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At first glance, this can seem like an unscientific book—you won’t find links to studies in this one, for sure! However, if we take a look at the seven circles in question, they are:
- Food
- Movement
- Sleep
- Ceremony
- Sacred Space
- Land
- Community
Regular 10almonds readers may notice that these seven items contain five of the things strongly associated with the “supercentenarian Blue Zones”. (If you are wondering why Native American reservations are not Blue Zones, the answer there lies less in health science and more in history and sociology, and what things have been done to a given people).
The authors—who are Native American, yes—present in one place a wealth of knowledge and know-how. Not even just from their own knowledge and their own respective tribes, but gathered from other tribes too.
Perhaps the strongest value of this book to the reader is in the explanation of noting the size of each of those circles, how they connect with each other, and providing a whole well-explained system for how we can grow each of them in harmony with each other.
Or to say the same thing in sciencey terms: how to mindfully improve integrated lifestyle factors synergistically for greater efficacy and improved health-adjusted quality-of-life years.
Bottom line: if you’re not averse to something that mostly doesn’t use sciencey terms of have citations to peer-reviewed studies peppered through the text, then this book has wisdom that’s a) older than the pyramids of Giza, yet also b) highly consistent with our current best science of Blue Zone healthy longevity.
Share This Post
-
Dandelion: Time For Evidence On Its Benefits?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In recent decades often considered a weed, now enjoying a resurgence in popularity due its benefits for pollinators, this plant has longer-ago been enjoyed as salad (leaves) or as a drink (roots), and is typically considered to have diuretic and digestion-improving properties. So… Does it?
Diuretic
Probably! Because of the ubiquity of anecdotal evidence, this hasn’t been well-studied, but here’s a small (n=17) study that found that it significantly increased urination:
The diuretic effect in human subjects of an extract of Taraxacum officinale folium over a single day
You may be thinking, “you usually do better than an n=17 study” and yes we do, but there’s an amazing paucity of human research when it comes to dandelions, as you’ll see:
Digestion-improving
There’s a lot of fiber in dandelion greens and roots both, and eating unprocessed or minimally-processed plants is (with obvious exceptions, such as plants that are poisonous) invariably going to improve digestion just by virtue of the fiber content alone.
As for dandelions, the roots are rich in inulin, a great prebiotic fiber that indeed definitely helps:
Effect of inulin in the treatment of irritable bowel syndrome with constipation (Review)
When it comes to studies that are specifically about dandelions, however, we are down to animal studies, such as:
The effect of Taraxacum officinale on gastric emptying and smooth muscle motility in rodents
Note that this is not about the fiber; this is about the plant extract (so, no fiber), and how it gets the intestinal muscles to do their thing with more enthusiasm. Of course you, dear reader, are probably not a rodent, we can’t say for sure that this will have this effect in humans. However, generally speaking, what works for mammals works for mammals, so it probably indeed helps.
For liver health
More about rats and not humans, but again, it’s promising. Dandelion extract appears to protect the liver, reducing the damage in the event of induced liver failure:
In other words: the researchers poisoned the rats, and those who took dandelion extract suffered less liver damage than those who didn’t.
…and more?
It may help improve blood triglycerides and reduce ischemic stroke risk, but most of this research is still in non-human animals:
And while we’re on the topic of blood, it likely has blood-sugar-lowering effects too; once again (you guessed it), mostly non-human animal studies, though, with some in vitro studies:
The Physiological Effects of Dandelion (Taraxacum Officinale) in Type 2 Diabetes
Want to try some?
We don’t sell it, but if you have a garden, that’s a great place to grow this very easy-to-grow plant without having to worry about pesticides etc.
Alternatively, if you’d like to buy it in supplement form, here’s an example product on Amazon 😎
Enjoy!
Share This Post
Related Posts
-
Plant-Based Alternatives for Meat Recipes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝How about providing a plant-based alternative when you post meat-based recipes? I appreciate how much you advocate for veggie diets and think offering an alternative with your recipes would support that❞
Glad you’re enjoying! And yes, we do usually do that. But: pardon, we missed one (the Tuna Steak with Protein Salad) because it’d be more than a simple this-for-that substitution, we didn’t already have an alternative recipe up (as with the salmon recipes such as the Chili Hot-Bedded Salmon and Thai Green Curry Salmon Burgers).
Our recipes, by the way, will tend towards being vegan, vegetarian, or at least pescatarian. This is for several reasons:
- Good science suggests the best diet for general purpose good health is one that is mostly plants, with optional moderate amounts of fermented dairy products, fish, and/or eggs.
- Your writer here (it’s me, hi) has been vegan for many years, transitioning to such via pescatarianism and ovo-lacto vegetarianism, and so the skill of cooking meat is least fresh in my memory, meaning I’d not be confident writing about that, especially as cooking meat has the gravest health consequences for messing it up.
Note on biases: notwithstanding this writer being vegan, we at 10almonds are committed to reporting the science as it stands with no agenda besides good health. Hence, there will continue to be unbiased information about animal products’ health considerations, positive as well as negative.
See also: Do We Need Animal Products To Be Healthy?
…as well as, of course, some animal-based classics from our archives including:
We Are Such Stuff As Fish Are Made Of & Eggs: All Things In Moderation?
Finishing with one for the vegans though, you might enjoy:
Which Plant Milk? We Compare 6 Of The Most Popular
Some previous articles you might enjoy meanwhile:
- Pinpointing The Usefulness Of Acupuncture
- Science-Based Alternative Pain Relief
- Peripheral Neuropathy: How To Avoid It, Manage It, Treat It
- What Does Lion’s Mane Actually Do, Anyway?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The End of Food Allergy – by Dr. Kari Nadeau & Sloan Barnett
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We don’t usually mention author credentials beyond their occupation/title. However, in this case it bears acknowledging at least the first line of the author bio:
❝Kari Nadeau, MD, PhD, is the director of the Sean N. Parker Center for Allergy and Asthma Research at Stanford University and is one of the world’s leading experts on food allergy❞
We mention this, because there’s a lot of quack medicine out there [in general, but especially] when it comes to things such as food allergies. So let’s be clear up front that Dr. Nadeau is actually a world-class professional at the top of her field.
This book is, by the way, about true allergies—not intolerances or sensitivities. It does touch on those latter two, but it’s not the main meat of the book.
In particular, most of the research cited is around peanut allergies, though the usual other common allergens are all discussed too.
The authors’ writing style is that of a science educator (Dr. Nadeau’s co-author, Sloan Barnett, is lawyer and health journalist). We get a clear explanation of the science from real-world to clinic and back again, and are left with a strong understanding, not just a conclusion.
The titular “End of Food Allergy” is a bold implicit claim; does the book deliver? Yes, actually.
The book lays out guidelines for safely avoiding food allergies developing in infants, and yes, really, how to reverse them in adults. But…
Big caveat:
The solution for reversing severe food allergies (e.g. “someone nearby touched a peanut three hours ago and now I’m in anaphylactic shock”), drug-assisted oral immunotherapy, takes 6–24 months of weekly several-hour-long clinic visits, relies on having a nearby clinic offering the service, and absolutely 100% cannot be done at home (on pain of probable death).
Bottom line: it’s by no means a magic bullet, but yes, it does deliver.
Click here to check out The End of Food Allergy to learn more!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Anti-Inflammatory Pineapple Fried Rice
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fried rice is not most people’s go-to when one thinks of health food, but this one is. It’s packed with plenty of nutrients, many of which are anti-inflammatory, but the real star is the pineapple (with its high bromelain content and thus particularly potent benefits).
You will need
- 2½ cups cooked wholegrain basmati rice (you can use our Tasty Versatile Rice recipe if you don’t already have leftovers to use)
- 1 cup pineapple chunks
- ½ red onion, diced
- 1 red bell pepper, diced
- ½ cup sweetcorn
- ½ peas
- 3 green onions, chopped
- 2 serrano peppers, chopped (omit if you don’t care for heat)
- 2 tbsp coconut oil
- 1 tbsp grated fresh ginger
- 1 tbsp black pepper, coarse ground
Method
(we suggest you read everything at least once before doing anything)
1) Fry the red onion, serrano peppers, and ginger in the coconut oil over a medium heat, stirring frequently, for about 3 minutes.
2) Add the pineapple, bell pepper, sweetcorn, peas, and black pepper, stirring frequently, for about another 3 minutes.
3) Add the rice, stirring gently but thoroughly, until fully reheated and mixed in.
4) Serve, garnishing with the green onions.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Eat To Beat Inflammation
- Ginger Does A Lot More Than You Think
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Bromelain vs Inflammation & Much More
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: