How Your Sleep Position Changes Dementia Risk
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is not just about sleep duration or even about sleep quality… It really is about which way your body is positioned.
Goodnight, glymphatic system
The association between sleeping position and dementia risk is about glymphatic drainage, which is largely powered by gravity (and thus dependent on which way around your head and neck are oriented), and very important for clearing toxins out of the brain—including beta-amyloid proteins.
This becomes particularly important when the glymphatic system becomes less efficient in midlife, often 15–20 years before cognitive decline symptoms appear.
The video’s thumbnail headline, “SCIENTISTS REVEAL: THE WAY YOUR SLEEP CAN CAUSE DEMENTIA” is overstated and inaccurate, but our adjusted headline “how your sleep position changes dementia risk” is actually representative of the paper on which this video was based; we’ll quote from the paper itself here:
❝This paper concludes that 1. glymphatic clearance plays a major role in Alzheimer’s pathology; 2. the vast majority of waste clearance occurs during sleep; 3. dementias are associated with sleep disruption, alongside an age-related decline in AQP4 polarization; and 4. lifestyle choices such as sleep position, alcohol intake, exercise, omega-3 consumption, intermittent fasting and chronic stress all modulate* glymphatic clearance. Lifestyle choices could therefore alter Alzheimer’s disease risk through improved glymphatic clearance, and could be used as a preventative lifestyle intervention for both healthy brain ageing and Alzheimer’s disease.❞
…and specifically, they found:
❝Glymphatic transport is most efficient in the right lateral sleeping position, with more CSF clearance occurring compared to supine and prone. The average person changes sleeping position 11 times per night, but there was no difference in the number of position changes between neurodegenerative and control groups, making the percentage of time spent in supine position the risk factor, not the number of position changes❞
Read the paper in full here: The Sleeping Brain: Harnessing the Power of the Glymphatic System through Lifestyle Choices
*saying “modulate” here is not as useful as it could be, because they modulate it differently: side-sleeping improves clearance; back sleeping decreases it; front-sleeping isn’t great either. Alcohol intake reduces clearance, exercise (especially cardiovascular exercise) improves it; omega-3 consumption improves it up a degree and does depend on omega-3/6 ratios, intermittent fasting improves it, and chronic stress worsens it.
And for a more pop-science presentation, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Clean Your Brain (Glymphatic Health Primer)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fruit, Fiber, & Leafy Greens… On A Low-FODMAP Diet!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fiber For FODMAP-Avoiders
First, let’s quickly cover: what are FODMAPs?
FODMAPs are fermentable oligosaccharides, disaccharides, monosaccharides, and polyols.
In plainer English: they’re carbohydrates that are resistant to digestion.
This is, for most people most of the time, a good thing, for example:
When Is A Fiber Not A Fiber? When It’s A Resistant Starch.
Not for everyone…
However, if you have inflammatory bowel syndrome (IBS), including ulcerative colitis, Crohn’s disease, or similar, then suddenly a lot of common dietary advice gets flipped on its head:
While digestion-resistant carbohydrates making it to the end parts of our digestive tract are good for our bacteria there, in the case of people with IBS or similar, it can be a bit too good for our bacteria there.
Which can mean gas (a natural by-product of bacterial respiration) accumulation, discomfort, water retention (as the pseudo-fiber draws water in and keeps it), and other related symptoms, causing discomfort, and potentially disease such as diarrhea.
Again: for most people this is not so (usually: quite the opposite; resistant starches improve things down there), but for those for whom it’s a thing, it’s a Big Bad Thing™.
Hold the veg? Hold your horses.
A common knee-jerk reaction is “I will avoid fruit and veg, then”.
Superficially, this can work, as many fruit & veg are high in FODMAPs (as are fermented dairy products, by the way).
However, a diet free from fruit and veg is not going to be healthy in any sustainable fashion.
There are, however, options for low-FODMAP fruit & veg, such as:
Fruits: bananas (if not overripe), kiwi, grapefruit, lemons, limes, melons, oranges, passionfruit, strawberries
Vegetables: alfalfa, bell peppers, bok choy, carrots, celery, cucumbers, eggplant, green beans, kale, lettuce, olives, parsnips, potatoes (and sweet potatoes, yams etc), radishes, spinach, squash, tomatoes*, turnips, zucchini
*our stance: botanically it’s a fruit, but culinarily it’s a vegetable.
For more on the science of this, check out:
Strategies for Producing Low FODMAPs Foodstuffs: Challenges and Perspectives ← table 2 is particularly informative when it comes to the above examples, and table 3 will advise about…
Bonus
Grains: oats, quinoa, rice, tapioca
…and wheat if the conditions in table 3 (linked above) are satisfied
(worth mentioning since grains also get a bad press when it comes to IBS, but that’s mostly because of wheat)
See also: Gluten: What’s The Truth?
Enjoy!
Share This Post
-
The Best 4 Pool Exercises to Strengthen Your Core & Tone Up
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of people don’t love working on their core strength, but exercising in the pool can make it a lot more enjoyable, as well as minimizing risk of injury.
Dr Alyssa Kuhn, arthritis specialist, also advises “being in the water also helps to control for balance and can offload the joints so they aren’t as painful”:
The gentlest exercise
The specific exercises she recommends are:
Wood Chops
Stagger your feet, clasp your hands, and submerge them in the water. Now, move your hands diagonally from one side to the other. This engages your core and balance using water resistance. Perform 10–20 reps per side, exhaling on the hardest part.
Front Kick with Opposite Arm Press
Kick one leg forward while pushing the opposite arm out or overhead—higher kicks increase difficulty by requiring more balance. If balance isn’t sufficient for you yet, hold onto the pool wall if needed. Either way, engage the core to lift the leg. Do 20–30 reps alternating sides.
Wall Push-Ups
Place your hands on the pool wall, shoulder-width apart. Keep feet together and hips slightly tucked for core engagement. Next, move your chest toward the wall and push back while maintaining a straight body—avoid arching your back. Do 10–20 reps.
Arm Circles
Stand with your feet wider than shoulder-width. Clasp your hands, extend your arms, and submerge them in the water. Make large circular motions for resistance training. This can be done with straight or bent arms for different difficulty levels. Do 10–20 circles in each direction.
For more on each of these plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Osteoporosis & Exercises: Which To Do (And Which To Avoid)
Take care!
Share This Post
-
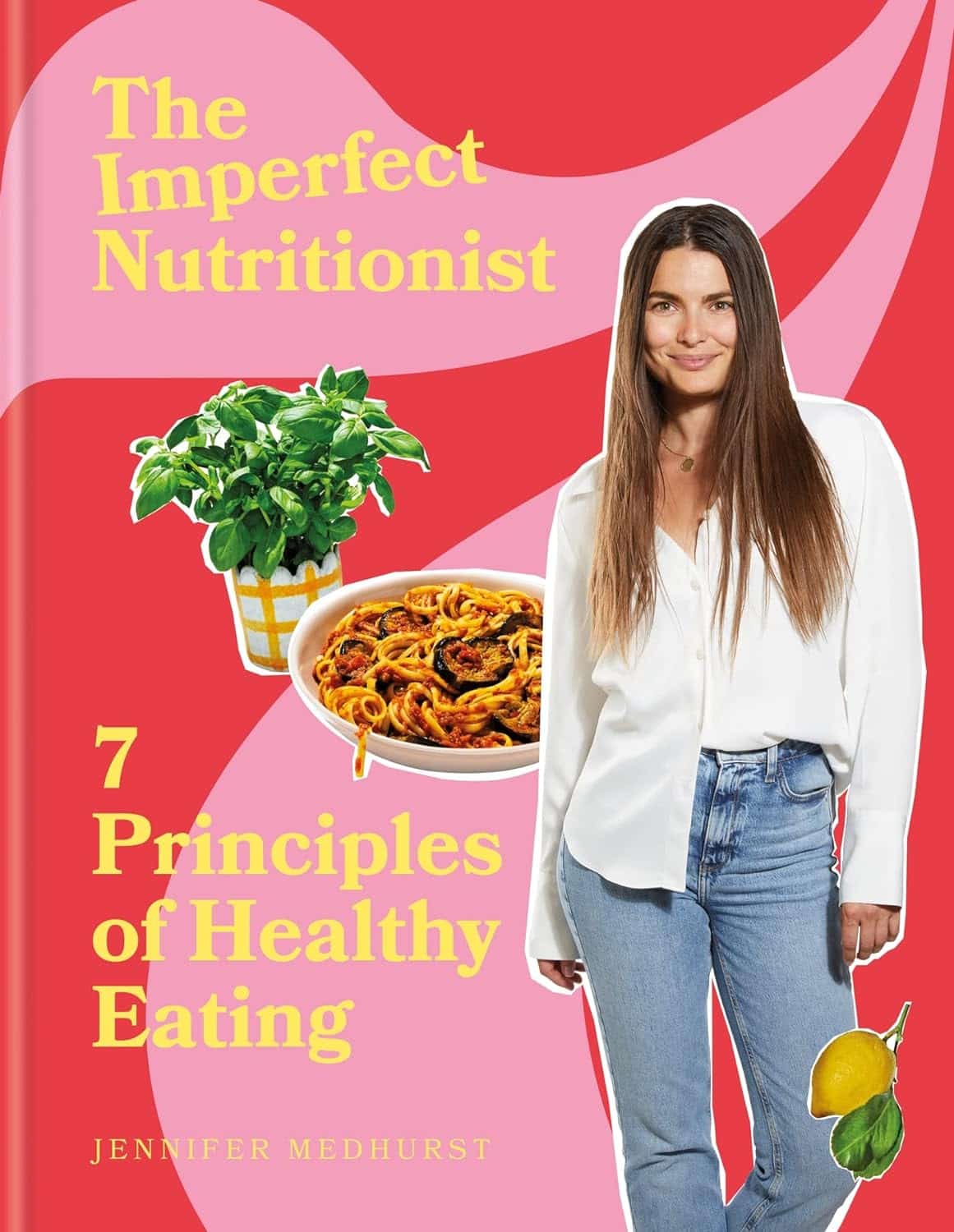
The Imperfect Nutritionist – by Jennifer Medhurst
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The idea of the “imperfect nutritionist” is to note that we’re all different with slightly different needs and sometimes very different preferences (or circumstances!) and having a truly perfect diet is probably a fool’s errand. Should we just give up, then? Not at all:
What we can do, Medhust argues, is find what’s best for us, realistically.
It’s better to have an 80% perfect diet 80% of the time, than to have a totally perfect diet for four and a half meals before running out of steam (and ingredients).
As for the “seven principles” mentioned in the title… we’re not going to keep those a mystery; they are:
- Focusing on wholefood
- Being diverse
- Knowing your fats
- Including fermented, prebiotic and probiotic foods
- Reducing refined carbohydrates
- Being aware of liquids
- Eating mindfully
The first part of the book is a treatise on how to implement those principles in your diet generally; the second part of the book is a recipe collection—70 recipes, with “these ingredients will almost certainly be available at your local supermarket” as a baseline. No instances of “the secret to being a good chef is knowing how to source fresh ingredients; ask your local greengrocer where to find spring-harvested perambulatory truffle-cones” here!
Basically, it focusses on adding healthy foods per your personal preferences and circumstances, and building these up into a repertoire of meals that will keep you and your family happy and healthy.
Pick Up Your Copy Of The Imperfect Nutritionist From Amazon Today!
Share This Post
Related Posts
-
The Smartest Way To Get To 20% Body Fat (Or 10% For Men)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
20% body fat for women, or 10% for men, are suggested in this video as ideal levels of adiposity for most people. While we certainly do have wiggle-room in either direction, going much higher than that can create a metabolic strain, and going much lower than that can cause immune dysfunction, organ damage, brittle bones, and more.
This video assumes you want to get down to those figures. If you want to go up to those figures because you are currently underweight, check out: How To Gain Weight (Healthily!)
Look at the small picture
The main trick, we are told, is to focus on small, incremental changes rather than obsessing over long-term weight loss goals (e.g. 20% body fat for women, 10% for men).
Next, throw out what science shows doesn’t work, such as restrictive or extreme dieting:
- Restrictive dieting doesn’t work as the body will try to save you from starvation by storing extra fat and slowing your metabolism to make your fat reserves last longer
- Extreme dieting doesn’t work because no matter how compelling it is to believe “I’ll just lose it in this extreme way, then maintain my new lower weight”, the vast body of research shows that weight loss in this way will be regained quickly afterwards, and for a significant minority, may even end up putting more back on than was originally lost. In either case, you’ll have put your mind and body through the wringer for no long-term gain.
The recommendation comes in three parts:
- Shift your mindset: detach motivation from timelines and vanity goals; focus instead on lifelong health and sustainable habits.
- Use an analytical approach: apply engineering principles: collect honest data and identify bottlenecks. Track food intake consistently, even during slip-ups, to identify areas for improvement. You remember the whole “it doesn’t count if it’s from someone else’s plate” thing? These days with food trackers, a lot of people fall into “it doesn’t count if I don’t record it”, but a head-in-the-sand approach will not get you where you want to be.
- Tackle bottlenecks incrementally: focus on one small, impactful change at a time (e.g. reducing soda intake). This way, you can build habits gradually to prevent willpower burnout and sustain your progress.
As an example of how this looked for Viva (in the video):
- > 30% body fat stage: she focused on reducing processed foods and portion sizes.
- 29–25% body fat stage: she prioritized nutrient-dense foods and reduced dining out.
- 24–20% body fat stage: she added strength training, improved sleep, and addressed her cravings and energy levels.
In short: look at the small picture; adjust your habits mindfully, keep a track of things, see what needs improvement and improve it, and don’t try to speedrun weight loss; just focus on what you are tangibly doing to keep things heading in the right direction, and you’ll get there 1% at a time.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Lose Weight, But Healthily ← our own guide, which is also consistent with the advice above, and talks about some specific things to pay attention to that weren’t mentioned in the video
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Insider’s Guide To Making Hospital As Comfortable As Possible
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Nobody Likes Surgery, But Here’s How To Make It Much Less Bad
This is Dr. Chris Bonney. He’s an anesthesiologist. If you have a surgery, he wants you to go in feeling calm, and make a quick recovery afterwards, with minimal suffering in between.
Being a patient in a hospital is a bit like being a passenger in an airplane:
- Almost nobody enjoys the thing itself, but we very much want to get to the other side of the experience.
- We have limited freedoms and comforts, and small things can make a big difference between misery and tolerability.
- There are professionals present to look after us, but they are busy and have a lot of other people to tend to too.
So why is it that there are so many resources available full of “tips for travelers” and so few “tips for hospital patients”?
Especially given the relative risks of each, and likelihood, or even near-certainty of coming to at least some harm… One would think “tips for patients” would be more in demand!
Tips for surgery patients, from an insider expert
First, he advises us: empower yourself.
Empowering yourself in this context means:
- Relax—doctors really want you to feel better, quickly. They’re on your side.
- Research—knowledge is power, so research the procedure (and its risks!). Dr. Bonney, himself an anesthesiologist, particularly recommends you learn what specific anesthetic will be used (there are many, and they’re all a bit different!), and what effects (and/or after-effects) that may have.
- Reframe—you’re not just a patient; you’re a customer/client. Many people suffer from MDeity syndrome, and view doctors as authority figures, rather than what they are: service providers.
- Request—if something would make you feel better, ask for it. If it’s information, they will be not only obliged, but also enthusiastic, to give it. If it’s something else, they’ll oblige if they can, and the worst case scenario is something won’t be possible, but you won’t know if you don’t ask.
Next up, help them to help you
There are various ways you can be a useful member of your own care team:
- Go into surgery as healthy as you can. If there’s ever a time to get a little fitter, eat a little healthier, prioritize good quality sleep more, the time approaching your surgery is the time to do this.
- This will help to minimize complications and maximize recovery.
- Take with you any meds you’re taking, or at least have an up-to-date list of what you’re taking. Dr. Bonney has very many times had patients tell him such things as “Well, let me see. I have two little pink ones and a little white one…” and when asked what they’re for they tell him “I have no idea, you’d need to ask my doctor”.
- Help them to help you; have your meds with you, or at least a comprehensive list (including: medication name, dosage, frequency, any special instructions)
- Don’t stop taking your meds unless told to do so. Many people have heard that one should stop taking meds before a surgery, and sometimes that’s true, but often it isn’t. Keep taking them, unless told otherwise.
- If unsure, ask your surgical team in advance (not your own doctor, who will not be as familiar with what will or won’t interfere with a surgery).
Do any preparatory organization well in advance
Consider the following:
- What do you need to take with you? Medications, clothes, toiletries, phone charger, entertainment, headphones, paperwork, cash for the vending machine?
- Will the surgeons need to shave anywhere, and if so, might you prefer doing some other form of depilation (e.g. waxing etc) yourself in advance?
- Is your list of medications ready?
- Who will take you to the hospital and who will bring you back?
- Who will stay with you for the first 24 hours after you’re sent home?
- Is someone available to look after your kids/pets/plants etc?
Be aware of how you do (and don’t) need to fast before surgery
The American Society of Anesthesiologists gives the following fasting guidelines:
- Non-food liquids: fast for at least 2 hours before surgery
- Food liquids or light snacks: fast for at least 6 hours before surgery
- Fried foods, fatty foods, meat: fast for at least 8 hours before surgery
(see the above link for more details)
Dr. Bonney notes that many times he’s had patients who’ve had the worst thirst, or caffeine headache, because of abstaining unnecessarily for the day of the surgery.
Unless told otherwise by your surgical team, you can have black coffee/tea up until two hours before your surgery, and you can and should have water up until two hours before surgery.
Hydration is good for you and you will feel the difference!
Want to know more?
Dr. Bonney has his own website and blog, where he offers lots of advice, including for specific conditions and specific surgeries, with advice for before/during/after your hospital stay.
He also has a book with many more tips like those we shared today:
Calm For Surgery: Supertips For A Smooth Recovery
Take good care of yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Morning Routines That Just FLOW
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Morning Routines That Just FLOW
“If the hardest thing you have to do in your day is eat a frog, eat that frog first!”, they say.
And, broadly speaking, it is indeed good to get anything stressful out of the way early, so that we can relax afterwards. But…
- Are we truly best at frog-eating when blurry-eyed and sleepy?
- Is there a spoonful of sugar that could make the medicine go down better?
- What do we need to turn eating the frog into an enjoyable activity?
Flow
“Flow” is a concept brought to public consciousness by psychologist Mihaly Csikszentmihalyi, and it refers to a state in which we feel good about what we’re doing, and just keep doing, at a peak performance level.
Writer’s note: as a writer, for example…
Sometimes I do not want to write, I pace to and fro near my computer, going on side-quests like getting a coffee or gazing out of the window into my garden. But once I get going, suddenly, something magical happens and before I know it, I have to trim my writing down because I’ve written too much. That magical window of effortless productivity was a state of flow.
Good morning!
What is a good morning, to you? Build that into your morning! Set parameters around it so you don’t get carried away timewise and find yourself in the afternoon (unless that would work for you!), but first thing in the morning is the time to light up each part of your brain with appropriate neurotransmitters.
Getting the brain juices flowing
Cortisol
When we wake up, we (unless we have some neurochemical imbalance, such as untreated depression) get a spike of cortisol. Cortisol is much-maligned and feared, and indeed it can be very much deleterious to the health in cases of chronic stress. But a little spike now and again is actually beneficial for us.
Quick Tip: if you want to artificially stimulate (or enhance) a morning cortisol spike, a cold shower is the way to go. Or even just a face-plunge into a bowl of ice-water (put ice in it, give it a couple of minutes to chill the water, then put your face in for a count of 30 seconds, or less if you can’t hold your breath that long).
Serotonin
Serotonin is generally thought of as “the happy chemical”, and it’s stimulated by blue/white light, and also by seeing greenery.
Quick tip: to artificially stimulate (or enhance) a morning serotonin boost, your best friend is sunlight. Even sun through a partly-clouded sky will tend to outperform artificial lighting, including artificial sunlight lighting. Try to get sun between 08:30 and 09:00, if you can. Best of all, do it in your garden or nearby park, as the greenery will be an extra boost!
Dopamine
Generally thought of as “the reward chemical”, but it’s also critical for a lot of kinds of brainwork, including language processing and problem-solving.
Quick Tip: to artificially stimulate* a dopamine surge to get you going, do something that you and/or your body finds rewarding. Examples include:
- Exercise, especially in a vigorous burst
- A good breakfast, a nice coffee, whatever feels right to you
- An app that has motivational bells and whistles, a streak for you to complete, etc
Note: another very enjoyable activity might come to mind that doesn’t even require you getting out of bed. Be aware, however, gentleman-readers specifically, that if you complete that activity, you’ll get a prolactin spike that will wipe out the dopamine you just worked up (because prolactin is antagonistic to dopamine). So that one’s probably better for a lazy morning when you can go back to sleep, than a day when you want to get up and go! Ladies, this is less of a worry for us as the physiology an orgasm driven by estrogen+progesterone rather than testosterone is different; there will not usually be a prolactin spike following the spike of dopamine; our orgasm-related dopamine spike is followed by a wave of oxytocin instead (“the cuddle chemical”), which is much more pleasant than prolactin.
*there’s no “(or enhance)” for this one; you won’t get dopamine from doing nothing, that’s just not how “the reward chemical” works
Flow-building in a stack
When you’ve just woken up and are in a blurry morning haze, that’s not the time to be figuring out “what should I be doing next?”, so instead:
- Work out the things you want to incorporate into your morning routine
- Put them in the order that will be easiest to perform—some things will go a lot better after others!
- Remember to also include things that are simply necessary—morning bathroom ablutions, for example
The goal here is to have a this-and-this-and-this-and-this list of items that you can go through without any deviations, and get in the habit of “after item 1 I automatically do item 2, after which I automatically do item 3, after which…”
Implement this, and your mornings will become practically automated, but in a joyous, life-enhancing way that sets you up in good order for whatever you want/need to do!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: