How to Fall Back Asleep After Waking Up in the Middle of the Night
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Michael Bruce, the Sleep Doctor, addresses a common concern: waking up in the middle of the night and struggling to fall back asleep.
Understanding the Wake-Up
Firstly, why are we waking up during the night?
Waking up between 2 AM and 3 AM is said to be normal, and linked to your core body temperature. As your body core temperature drops, to trigger melatonin release, and then rises again, you get into a lighter stage of sleep. This lighter stage of sleep makes you more prone to waking up.
Note, there are also some medical conditions (such as sleep apnea) that can cause you to wake up during the night.
But, what can we do about it? Aside from constantly shifting sleeping position (Should I be sleeping on my back? On my left? Right?)
Avoid the Clock
The first step is to resist the urge to check the time. It’s easy to be tempted to have a look at the clock, however, doing so can increase anxiety, making it harder to fall back asleep. As Dr. Bruce says, sleep is like love—the less you chase it, the more it comes.
It may be useful to point your alarm clock (if you still have one of those) the opposite direction to your bed.
Embracing Non-Sleep Deep Rest (NSDR)
Whilst this may not help you fall back asleep, it’s worth pointing out that just lying quietly in the dark without moving still offers rejuvenation. This revujenating stage is called Non-Sleep Deep Rest (otherwise known as NSDR)
If you’re not familiar with NSDR, check out our overview of Andrew Huberman’s opinions on NSDR here.
So, you can reassure yourself that whilst you may not be asleep, you are still resting.
Keep Your Heart Rate Down
To fall back asleep, it’s best if your heart rate is below 60 bpm. So, Dr. Bruce advises avoiding void getting up unnecessarily, as moving around can elevate your heart rate.
On a similar vain, he introduces the 4-7-8 breathing technique, which is designed to lower your heart rate. The technique is simple:
- Breathe in for 4 seconds.
- Hold for 7 seconds.
- Exhale for 8 seconds.
Repeat this cycle gently to calm your body and mind.
As per any of our Video Breakdowns, we only try to capture the most important pieces of information in text; the rest can be garnered from the video itself:
Wishing you a thorough night’s rest!
Do you know any other good videos on sleep? Send them to us via email!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Radiant Rebellion – by Karen Walrond
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In health terms, we are often about fighting aging here. But to be more specific, what we’re fighting in those cases is not truly aging itself, so much as age-related decline.
Karen Walrond makes a case that we’ve made from the very start of 10almonds (but she wrote a whole book about it), that there’s merit in looking at what we can and can’t control about aging, doing what we reasonably can, and embracing what we can’t.
And yes, embracing, not merely accepting. This is not a downer of a book; it’s a call to revolution. It asks us to be proud of our grey hairs, to see our smile-lines around our eyes as the sign of a lived-in body, and even to embrace some of the unavoidable “actual decline” things as part of the journey of life. Maybe we’re not as strong as we used to be and now need a grippety-doodah to open jars; not everyone gets to live long enough to experience that! How lucky we are.
Perhaps most importantly, she bids us be the change we want to see in the world, and inspire others with our choices and actions, and shake off ageist biases for good.
Bottom line: if you want to foster a better attitude to aging not only for yourself, but also those around you, then this is a top-tier book for that.
Click here to check out Radiant Rebellion, and reclaim aging!
Share This Post
-
Grain Brain – by Dr. David Perlmutter
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you’re a regular 10almonds reader, you probably know that refined flour, and processed food in general, is not great for the health. So, what does this book offer more?
Dr. Perlmutter sets out the case against (as the subtitle suggests) wheat, carbs, and sugar. Yes, including wholegrain wheat, and including starchy vegetables such as potatoes and parsnips. Fruit does also come under scrutiny, a clear distinction is made between whole fruits and juices. In the latter case, the lack of fiber (along with the more readily absorbable liquid state) allows for those sugars to zip straight into our blood.
The book includes lots of stats and facts, and many study citations, along with infographics and clear explanations.
If the book has a weakness, it’s when it forgets to clarify something that was obvious to the author. For example, when he talks about our ancestors’ diets being 75% fat and 5% carbs, he neglects to mention that this is 75% by calorie count, not by mass or volume. This makes a huge difference! It’s the difference between a fat-guzzling engine, and someone who eats mostly fruit and oily nuts but also some very high-fat meat/organs.
The book’s strengths, on the other hand, are found in its explanation, backed by good science, of what wheat, along with excessive carbohydrates (especially sugar) can do to our body, including (and most focusedly, hence the title) our brain, leading the way to not just obvious metabolic disorders like diabetes, but also inflammatory diseases like Alzheimer’s.
Bottom line: you don’t have to completely revamp your diet if it’s working for you, but data is data, and this book has lots, making it well-worth a read.
Click here to check out Grain Brain, and learn about how to avoid inflaming yours!
Share This Post
-
Putting a Halt to Feeling Lost, Anxious, Stressed & Unhappy
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Starting From the Middle
Today’s video (below) dives straight into the heart of the issue, examining the victim mindset, with Dr. Gabor Maté immediately, and quite vulnerably, sharing his personal experiences conquering feelings of despair and anxiety.
As one of the comments on the video says, Dr. Maté is a “person who teaches about something because they experience it themselves”. And it shows through his approach.
With raw honesty, Dr. Maté empathizes with those grappling with inner turmoil, offering hope by emphasizing the power of healing in the present moment.
What is His Method?
Explained simply, Dr. Maté urges individuals to seek trauma-informed care and therapies that address underlying wounds; he emphasizes the pitfalls of relying solely on medication, and instead highlights the idea that triggers can be seen as opportunities for self-reflection and growth. He urges individuals to approach their triggers with compassionate curiosity rather than self-judgment.
In short, Dr Maté’s empathetic approach immediately calms the viewer, whilst providing knowledge crucial to self-improvement.
Let this video act as a reminder that we should take our mental health as seriously as our general health.
How was the video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Share This Post
Related Posts
-
Water Water Everywhere, But Which Is Best To Drink?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Well Well Well…
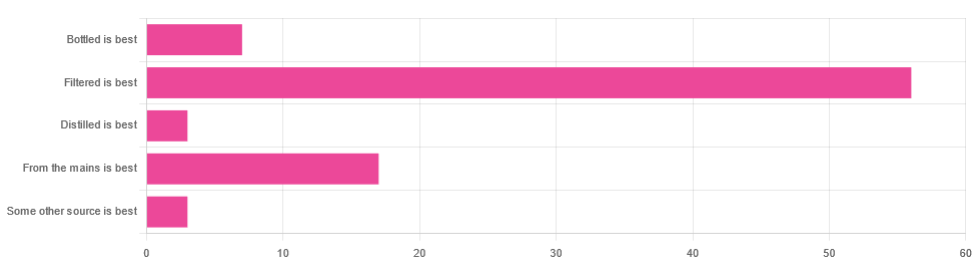
In Tuesday’s newsletter, we asked you for your (health-related) opinion on drinking water—with the understanding that this may vary from place to place. We got the above-depicted, below-described, set of responses:
- About 65% said “Filtered is best”
- About 20% said “From the mains is best”
- About 8% said “Bottled is best”
- About 3% said “Distilled is best”
- About 3% said “Some other source is best”
Of those who said “some other source is best”, one clarified that their preferred source was well water.
So what does the science say?
Fluoridated water is bad for you: True or False?
False, assuming a normal level of consumption. Rather than take up more space today though, we’ll link to what we previously wrote on this topic:
You may be wondering: but what if my level of consumption is higher than normal?
Let’s quickly look at some stats:
- The maximum permitted safety level varies from place to place, but is (for example) 2mg/l in the US, 1.5mg/l in Canada & the UK.
- The minimum recommended amount also varies from place to place, but is (for example) 0.7mg/l in Canada and the US, and 1mg/l in the UK.
It doesn’t take grabbing a calculator to realize that if you drink twice as much water as someone else, then depending on where you are, water fluoridated to the minimum may give you more than the recommended maximum.
However… Those safety margins are set so much lower than the actual toxicity levels of fluoride, that it doesn’t make a difference.
For example: your writer here takes a medication that has the side effect of causing dryness of the mouth, and consequently she drinks at least 3l of water per day in a climate that could not be described as hot (except perhaps for about 2 weeks of the year). She weighs 72kg (that’s about 158 pounds), and the toxicity of fluoride (for ill symptoms, not death) is 0.2mg/kg. So, she’d need 14.4mg of fluoride, which even if the water fluoridation here were 2mg/l (it’s not; it’s lower here, but let’s go with the highest figure to make a point), would require drinking more than 7l of water faster than the body can process it.
For more about the numbers, check out:
Acute Fluoride Poisoning from a Public Water System
Bottled water is the best: True or False?
False, if we consider “best” to be “healthiest”, which in turn we consider to be “most nutrients, with highest safety”.
Bottled water generally does have higher levels of minerals than most local mains supply water does. That’s good!
But you know what else is generally has? Microplastics and nanoplastics. That’s bad!
We don’t like to be alarmist in tone; it’s not what we’re about here, but the stats on bottled water are simply not good; see:
We Are Such Stuff As Bottles Are Made Of
You may be wondering: “but what about bottled water that comes in glass bottles?”
Indeed, water that comes in glass bottles can be expected to have lower levels of plastic than water that comes in plastic bottles, for obvious reasons.
However, we invite you to consider how likely you believe it to be that the water wasn’t stored in plastic while being processed, shipped and stored, before being portioned into its final store-ready glass bottles for end-consumer use.
Distilled water is the best: True or False?
False, generally, with caveats:
Distilled water is surely the safest water anywhere, because you know that you’ve removed any nasties.
However, it’s also devoid of nutrients, because you also removed any minerals it contained. Indeed, if you use a still, you’ll be accustomed to the build-up of these minerals (generally simplified and referenced as “limescale”, but it’s a whole collection of minerals).
Furthermore, that loss of nutrients can be more than just a “something good is missing”, because having removed certain ions, that water could now potentially strip minerals from your teeth. In practice, however, you’d probably have to swill it excessively to cause this damage.
Nevertheless, if you have the misfortune of living somewhere like Flint, Michigan, then a water still may be a fair necessity of life. In other places, it can simply be useful to have in case of emergency, of course.
Here’s an example product on Amazon if you’d like to invest in a water still for such cases.
PS: distilled water is also tasteless, and is generally considered bad, tastewise, for making tea and coffee. So we really don’t recommend distilling your water unless you have a good reason to do so.
Filtered water is the best: True or False?
True for most people in most places.
Let’s put it this way: it can’t logically be worse than whatever source of water you put into it…
Provided you change the filter regularly, of course.
Otherwise, after overusing a filter, at best it won’t be working, and at worst it’ll be adding in bacteria that have multiplied in the filter over however long you left it there.
You may be wondering: can water filters remove microplastics, and can they remove minerals?
The answer in both cases is: sometimes.
- For microplastics it depends on the filter size and the microplastic size (see our previous article for details on that).
- For minerals, it depends on the filter type. Check out:
The H2O Chronicles | 5 Water Filters That Remove Minerals
One other thing to think about: while most water filtration jugs are made of PFAS-free BPA-free plastics for obvious reasons, for greater peace of mind, you might consider investing in a glass filtration jug, like this one ← this is just one example product on Amazon; by all means shop around and find one you like
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
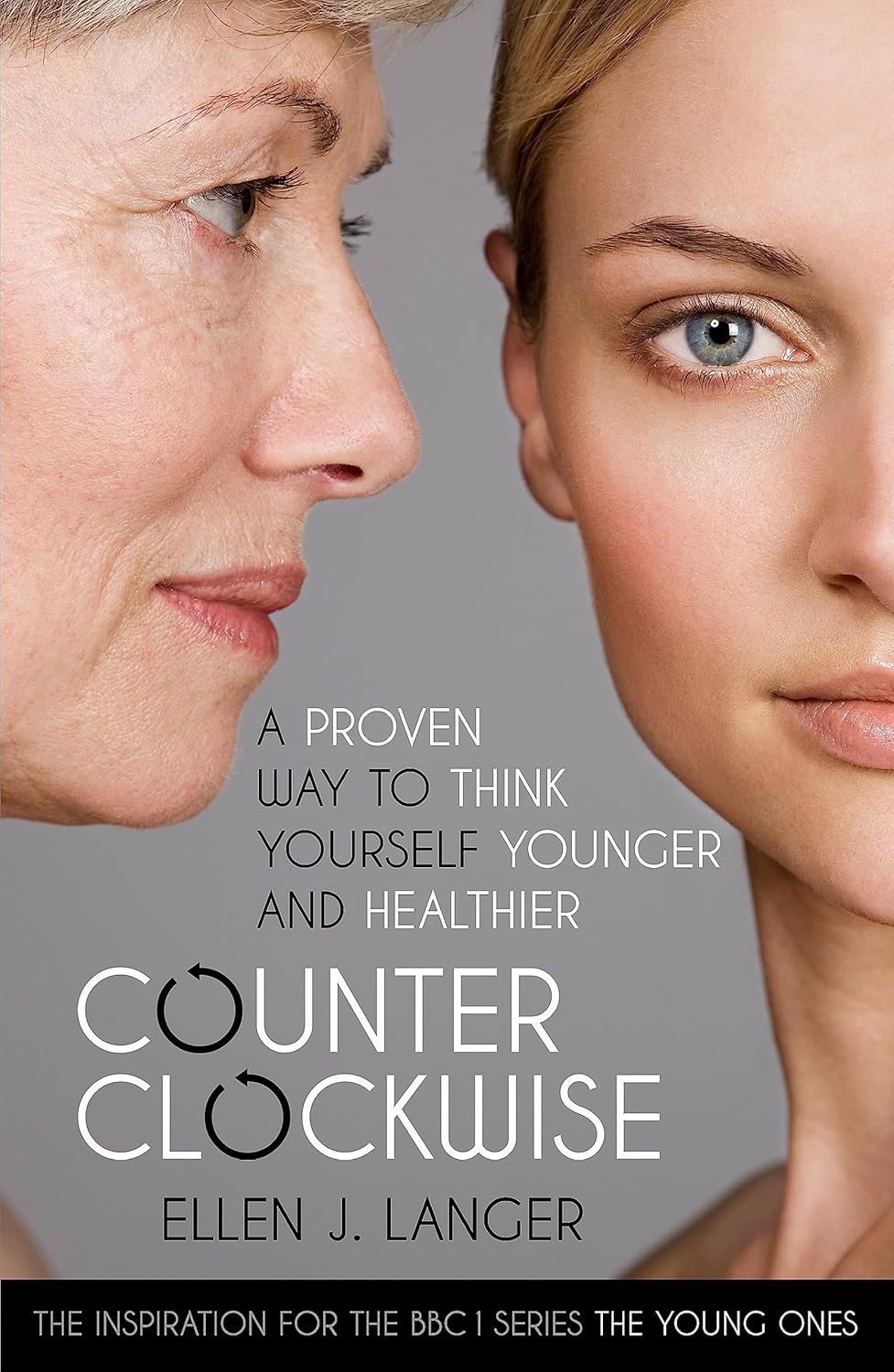
Counterclockwise – by Dr. Ellen Langer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written previously about Dr. Langer’s famous “Counterclockwise” study that saw reversals in biological markers of aging after a one-week intervention that consisted only of a (albeit rather intensive) mental reframe with regard to their age.
This book, as you might expect from the title, refers to that experiment a lot—but it doesn’t stop there. While the Counterclockwise experiment remains Dr. Langer’s most well-known, it’s not her most recent, and she draws from a wealth of research (her own and that of her colleagues in the field) to show the extent and limit of psychosomatic effect on aging.
Note:
- psychosomatic effect does not mean: “imagining it”
- psychosomatic effect means: “your brain regulates almost everything else in your body, directly or indirectly, including your autonomic functions, which includes immune function, tissue replacement, and more”
And as for when it comes to aging? Aging, like cancer, is in large part a problem of immune dysfunction; in both cases cells (be they senescent or cancerous, respectively) are not being killed when they are supposed to be, and in both cases, better instructions will improve the matter.
Many larger-scale markers of aging, such as mobility, are a case of the body only being able to do what the tissues allow, and the tissues are being constantly rebuilt (for better or for worse) according to autonomically-implemented specifications, and cells’ ability to carry out those orders.
Beyond the cellular physiology, this book discusses (a lot) the brain-down mechanisms by which the most powerful organ in our body can tell the rest of the body how old to be.
Dr. Langer also discusses the matter of “priming”, that is to say, how external factors prime us to believe certain things about our age and, with it, our health. These things can include popular media, conversations with friends and family, and healthcare providers’ framing of certain issues.
For example, a person just under a certain age and a person just over a certain age could both go to the doctor with the same complaint—a pain in a certain joint, let’s say. The doctor may refer the slightly younger patient for an x-ray because “let’s see what’s going on here”, and prescribe the slightly older patient some painkillers because “this is perfectly normal at your age”. One resultant problem is obvious: a difference in the standard of care. But the other resultant problem is less obvious: the older patient has now been primed to believe, by a confident authority figure, “it is natural for my body to be in a state of decline now, and this is what to expect”.
Thus, Dr. Langer prescribes mindfulness, not in the mindfulness meditation sense (though sure, do that too), but rather in the sense of consciously interacting with the world and making our own decisions about our own health and, yes, our own age. Because after all, our body neither knows nor cares how many times it has flown around the sun, and merely responds to physiological stimuli—including those we can influence with psychological reframing.
The book is not, per se, a “how-to” guide, rather it is an explanatory treatise, but it contains more than enough information to put it into practice, and indeed, she does also provide some exercises to do along the way.
The style is… Vivacious, without being especially upbeat. Dr. Langer is enthused about her work, yes, but she’s also angry at how many people are having their health sabotaged on the daily, and calls for a more health-first approach (as opposed to illness-first).
Bottom line: this is the book on our brain’s power over aging, so if that topic interests you, this book absolutely belongs on your bookshelf. Well, in your hands, and then on the bookshelf, and then back in your hands from time to time.
Click here to check out Counterclockwise, and age counterclockwise as her experimental subjects did!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Peanuts vs Hazelnuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing peanuts to hazelnuts, we picked the hazelnuts.
Why?
It was close!
In terms of macros, peanuts have more protein while hazelnuts have more fiber and fat; the fat is healthy (mostly monounsaturated, some polyunsaturated, and very little saturated; less saturated fat than peanuts), so all in all, we’ll call this category a modest, subjective win for hazelnuts (since it depends on what we consider most important).
In the category of vitamins, peanuts have more of vitamins B2, B3, B5, B9, and choline, while hazelnuts have more of vitamins A, B1, B6, C, E, and K, making this one a marginal win for hazelnuts.
When it comes to minerals, peanuts have more magnesium, phosphorus, selenium, and zinc, while hazelnuts have more calcium, copper, iron, and manganese, so we’re calling it a tie on minerals.
Adding up the sections makes for a very close win for hazelnuts, but by all means enjoy both (unless you are allergic, of course)!
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: