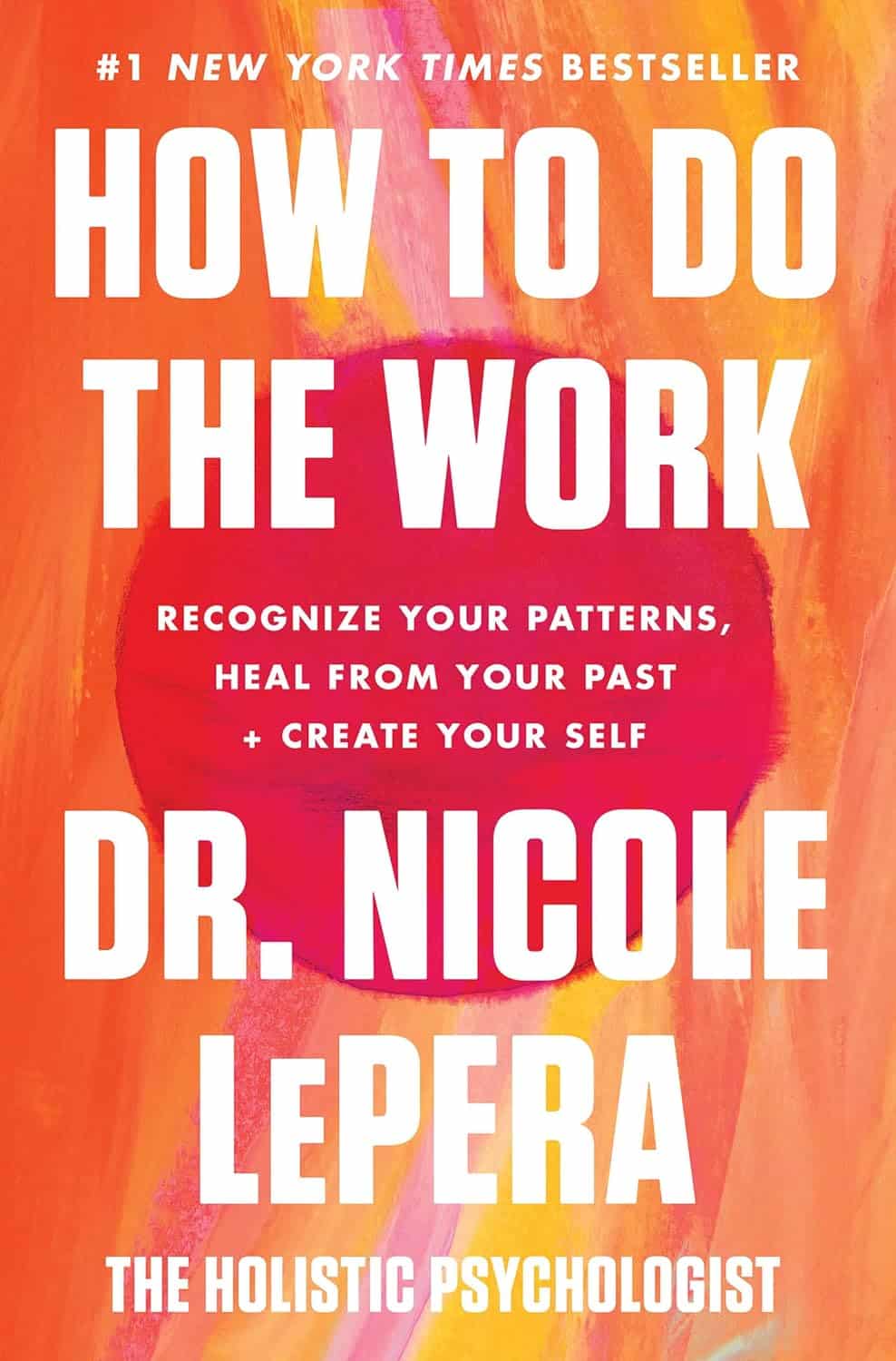
How to Do the Work – by Dr. Nicole LaPera
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We have reviewed some self-therapy books before, and they chiefly have focused on CBT and mindfulness, which are great. This one’s different.
Dr. Nicole LaPera has a bolder vision for what we can do for ourselves. Rather than giving us some worksheets for unraveling cognitive distortions or clearing up automatic negative thoughts, she bids us treat the cause, rather than the symptom.
For most of us, this will be the life we have led. Now, we cannot change the parenting style(s) we received (or didn’t), get a redo on childhood, avoid mistakes we made in our adolescence, or face adult life with the benefit of experience we gained right after we needed it most. But we can still work on those things if we just know how.
The subtitle of this book promsies that the reader can/will “recognise your patterns, heal from your past, and create your self”.
That’s accurate, for the content of the book and the advice it gives.
Dr. LaPera’s focus is on being our own best healer, and reparenting our own inner child. Giving each of us the confidence in ourself; the love and care and/but also firm-if-necessary direction that a (good) parent gives a child, and the trust that a secure child will have in the parent looking after them. Doing this for ourselves, Dr. LaPera holds, allows us to heal from traumas we went through when we perhaps didn’t quite have that, and show up for ourselves in a way that we might not have thought about before.
If the book has a weak point, it’s that many of the examples given are from Dr. LaPera’s own life and experience, so how relatable the specific examples will be to any given reader may vary. But, the principles and advices stand the same regardless.
Bottom line: if you’d like to try self-therapy on a deeper level than CBT worksheets, this book is an excellent primer.
Click here to check out How To Do The Work, and empower yourself to indeed do the work!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Hormone Therapy That Reduces Breast Cancer Risk & More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Hormone Balancing Act
We’ve written before about menopausal HRT:
What You Should Have Been Told About Menopause Beforehand
…and even specifically about the considerations when it comes to breast cancer risk:
Menopausal Hormone Replacement Therapy
this really does bear reading, by the way—scroll down to the bit about breast cancer risk, because it’s not a simple increased/decreased risk; it can go either way, and which way it goes will depend on various factors including your medical history and what HRT, if any, you are taking.
Hormone Modulating Therapy
Hormone modulating therapy, henceforth HMT, is something a little different.
Instead of replacing hormones, as hormone replacement therapy does, guess what hormone modulating therapy does instead? That’s right…
MHT can modulate hormones by various means, but the one we’re going to talk about today does it by blocking estrogen receptors,
Isn’t that the opposite of what we want?
You would think so, but since for many people with an increased breast cancer risk, the presence of estrogen increases that risk, which leaves menopausal (peri- or post) people in an unfortunate situation, having to choose between increased breast cancer risk (with estrogen), or osteoporosis and increased dementia risk, amongst other problems (without).
However, the key here (in fact, that’s a very good analogy) is in how the blocker works. Hormones and their receptors are like keys and locks, meaning that the wrong-shaped hormone won’t accidentally trigger it. And when the right-shaped hormone comes along, it gets activated and the message (in this case, “do estrogenic stuff here!” gets conveyed). A blocker is sufficiently similar to fit into the receptor, without being so similar as to otherwise act as the hormone.
In this case, it has been found that HMT blocking estrogen receptors was sufficient to alleviate the breast cancer risk, while also being associated with a 7% lower risk of developing Alzheimer’s disease or related dementias, with that risk reduction being even greater for some demographics depending on race and age. Black women in the 65–74 age bracket enjoyed a 24% relative risk reduction, with white women of the same age getting an 11% relative risk reduction. Black women enjoyed the same benefits after that age, whereas white women starting it at that age did not get the same benefits. The conclusion drawn from this is that it’s good to start this at 65 if relevant and practicable, especially if white, because the protective effect is strongest when gained aged 65–69.
Here’s a pop-science article that goes into the details more deeply than we have room for here:
Hormone therapy for breast cancer linked with lower dementia risk
And here’s the paper itself; we highly recommend reading at least the abstract, because it goes into the numbers in much more detail than we reasonably can here. It’s a huge cohort study of 18,808 women aged 65 years or older, so this is highly relevant data:
Want to learn more?
If you’d like a much deeper understanding of breast cancer risk management, including in the context of hormone therapy, you might like this excellent book that we reviewed recently:
The Smart Woman’s Guide to Breast Cancer – by Dr. Jenn Simmons
Take care!
Share This Post
-
Knit for Health & Wellness – by Betsan Corkhill
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Betsan Corkhill, a physiotherapist, has more than just physiotherapy in mind when it comes to the therapeutic potential of knitting (although yes, also physiotherapy!), and much of this book is about the more psychological benefits that go way beyond “it’s a relaxing pastime”.
She makes the case for how knitting (much like good mental health) requires planning, action, organization, persistence, focus, problem-solving, and flexibility—and thus the hobby develops and maintains all the appropriate faculties for those things, which will then be things you get to keep in the rest of your life, too.
Fun fact: knitting, along with other similar needlecrafts, was the forerunner technology for modern computer programming! And indeed, early computers, the kind with hole-punch data streams, used very similar pattern-storing methods to knitting patterns.
So, for something often thought of as a fairly mindless activity for those not in the know, knitting has a lot to offer for what’s between your ears, as well as potentially something for keeping your ears warm later.
One thing this book’s not, by the way: a “how to” guide for learning to knit. It assumes you either have that knowledge already, or will gain it elsewhere (there are many tutorials online).
Bottom line: if you’re in the market for a new hobby that’s good for your brain, this book will give you great motivation to give knitting a go!
Click here to check out Knit For Health & Wellness, and get knitting!
Share This Post
-
One More Resource Against Osteoporosis!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Your Bones Were Made For Moving Too!
We know that to look after bone health, resistance training is generally what’s indicated. Indeed, we mentioned it yesterday, and we’ve talked about it before:
Resistance Is Useful! (Especially As We Get Older)
We also know that if you have osteoporosis already, some exercises are a better or worse idea than others:
Osteoporosis & Exercises: Which To Do (And Which To Avoid)
However! New research suggests that also getting in your recommended 150 minutes per week of moderate exercise slows bone density loss.
The study by Dr. Tiina Savikangas et al. looked at 299 people in their 70s (just over half being women) and found that, over the course of a year, bone mineral density loss was inversely correlated with moderate exercise as recorded by an accelerometer (as found in most fitness-tracking wearables and smartphones).
In other words: those who got more minutes of exercise, kept more bone mineral density.
As well as monitoring bone mineral density, the study also looked at cross-sectional area, but that remained stable throughout.
As for how much is needed:
❝Even short bursts of activity can be significant for the skeleton, so we also looked at movement in terms of the number and intensity of individual impacts. For example, walking and running cause impacts of different intensities.
We found that impacts that were comparable to at least brisk walking were associated with better preservation of bone mineral density.❞
Read more: Impacts during everyday physical activity can slow bone loss ← pop-science source, interviewing the lead researcher
On which note, we’ve a small bone to pick…
As a small correction, the pop-science source says that the subjects’ ages ranged from 70 to 85 years; the paper, meanwhile, clearly shows that the age-range was 74.4±3.9 years (shown in the “Results” table), rounded to 74.4 ± 4 years, in the abstract. So, certainly no participant was older than 78 years and four months.
Why this matters: the age range itself may be critical or it might not, but what is important is that this highlights how we shouldn’t just believe figures cited in pop-science articles, and it’s always good to click through to the source!
This paper is a particularly fascinating read if you have time, because—unlike a lot of studies—they really took great care to note what exactly can and cannot be inferred from the data, and how and why.
Especially noteworthy was the diligence with which they either controlled for, or recognized that they could not control for, far more variables than most studies even bother to mention.
This kind of transparency is critical for good science, and we’d love to see more of it!
Want to apply this to your life?
Tracking minutes-of-movement is one of the things that fitness trackers are best at, so connect your favourite app (one of these days we’ll do a fitness tracker comparison article) and get moving!
And as for the other things that fitness trackers do? As it turns out, they do have their strengths and weaknesses, which are good to bear in mind:
Take care!
Share This Post
Related Posts
-
Our ‘food environments’ affect what we eat. Here’s how you can change yours to support healthier eating
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In January, many people are setting new year’s resolutions around healthy eating. Achieving these is often challenging – it can be difficult to change our eating habits. But healthy diets can enhance physical and mental health, so improving what we eat is a worthwhile goal.
One reason it’s difficult to change our eating habits relates to our “food environments”. This term describes:
The collective physical, economic, policy and sociocultural surroundings, opportunities and conditions that influence people’s food and beverage choices and nutritional status.
Our current food environments are designed in ways that often make it easier to choose unhealthy foods than healthy ones. But it’s possible to change certain aspects of our personal food environments, making eating healthier a little easier.
Unhealthy food environments
It’s not difficult to find fast-food restaurants in Australian cities. Meanwhile, there are junk foods at supermarket checkouts, service stations and sporting venues. Takeaway and packaged foods and drinks routinely come in large portion sizes and are often considered tastier than healthy options.
Our food environments also provide us with various prompts to eat unhealthy foods via the media and advertising, alongside health and nutrition claims and appealing marketing images on food packaging.
At the supermarket, unhealthy foods are often promoted through prominent displays and price discounts.
We’re also exposed to various situations in our everyday lives that can make healthy eating challenging. For example, social occasions or work functions might see large amounts of unhealthy food on offer.
Not everyone is affected in the same way
People differ in the degree to which their food consumption is influenced by their food environments.
This can be due to biological factors (for example, genetics and hormones), psychological characteristics (such as decision making processes or personality traits) and prior experiences with food (for example, learned associations between foods and particular situations or emotions).
People who are more susceptible will likely eat more and eat more unhealthy foods than those who are more immune to the effects of food environments and situations.
Those who are more susceptible may pay greater attention to food cues such as advertisements and cooking smells, and feel a stronger desire to eat when exposed to these cues. Meanwhile, they may pay less attention to internal cues signalling hunger and fullness. These differences are due to a combination of biological and psychological characteristics.
These people might also be more likely to experience physiological reactions to food cues including changes in heart rate and increased salivation.
It’s common to eat junk food in front of the TV.
PR Image Factory/ShutterstockOther situational cues can also prompt eating for some people, depending on what they’ve learned about eating. Some of us tend to eat when we’re tired or in a bad mood, having learned over time eating provides comfort in these situations.
Other people will tend to eat in situations such as in the car during the commute home from work (possibly passing multiple fast-food outlets along the way), or at certain times of day such as after dinner, or when others around them are eating, having learned associations between these situations and eating.
Being in front of a TV or other screen can also prompt people to eat, eat unhealthy foods, or eat more than intended.
Making changes
While it’s not possible to change wider food environments or individual characteristics that affect susceptibility to food cues, you can try to tune into how and when you’re affected by food cues. Then you can restructure some aspects of your personal food environments, which can help if you’re working towards healthier eating goals.
Although both meals and snacks are important for overall diet quality, snacks are often unplanned, which means food environments and situations may have a greater impact on what we snack on.
Foods consumed as snacks are often sugary drinks, confectionery, chips and cakes. However, snacks can also be healthy (for example, fruits, nuts and seeds).
Try removing unhealthy foods, particularly packaged snacks, from the house, or not buying them in the first place. This means temptations are removed, which can be especially helpful for those who may be more susceptible to their food environment.
Planning social events around non-food activities can help reduce social influences on eating. For example, why not catch up with friends for a walk instead of lunch at a fast-food restaurant.
Creating certain rules and habits can reduce cues for eating. For example, not eating at your desk, in the car, or in front of the TV will, over time, lessen the effects of these situations as cues for eating.
You could also try keeping a food diary to identify what moods and emotions trigger eating. Once you’ve identified these triggers, develop a plan to help break these habits. Strategies may include doing another activity you enjoy such as going for a short walk or listening to music – anything that can help manage the mood or emotion where you would have typically reached for the fridge.
Write (and stick to) a grocery list and avoid shopping for food when hungry. Plan and prepare meals and snacks ahead of time so eating decisions are made in advance of situations where you might feel especially hungry or tired or be influenced by your food environment.
Georgie Russell, Senior Lecturer, Institute for Physical Activity and Nutrition (IPAN), Deakin University and Rebecca Leech, NHMRC Emerging Leadership Fellow, School of Exercise and Nutrition Sciences, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
HRT: Bioidentical vs Animal
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
HRT: A Tale Of Two Approaches
In yesterday’s newsletter, we asked you for your assessment of menopausal hormone replacement therapy (HRT).
- A little over a third said “It can be medically beneficial, but has some minor drawbacks”
- A little under a third said “It helps, but at the cost of increased cancer risk; not worth it”
- Almost as many said “It’s a wondrous cure-all that makes you happier, healthier, and smell nice too”
- Four said “It is a dangerous scam and a sham; “au naturel” is the way to go”
So what does the science say?
Which HRT?
One subscriber who voted for “It’s a wondrous cure-all that makes you healthier, happier, and smell nice too” wrote to add:
❝My answer is based on biodentical hormone replacement therapy. Your survey did not specify.❞
And that’s an important distinction! We did indeed mean bioidentical HRT, because, being completely honest here, this European writer had no idea that Premarin etc were still in such wide circulation in the US.
So to quickly clear up any confusion:
- Bioidentical hormones: these are (as the name suggests) identical on a molecular level to the kind produced by humans.
- Conjugated Equine Estrogens: such as Premarin, come from animals. Indeed, the name “Premarin” comes from “pregnant mare urine”, the substance used to make it.
There are also hormone analogs, such as medroxyprogesterone acetate, which is a progestin and not the same thing as progesterone. Hormone analogs such as the aforementioned MPA are again, a predominantly-American thing—though they did test it first in third-world countries, after testing it on animals and finding it gave them various kinds of cancer (breast, cervical, ovarian, uterine).
A quick jumping-off point if you’re interested in that:
Depot medroxyprogesterone acetate and the risk of breast and gynecologic cancer
this is about its use as a contraceptive (so, much lower doses needed), but it is the same thing sometimes given in the US as part of menopausal HRT. You will note that the date on that research is 1996; DMPA is not exactly cutting-edge and was first widely used in the 1950s.
Similarly, CEEs (like Premarin) have been used since the 1930s, while estradiol (bioidentical estrogen) has been in use since the 1970s.
In short: we recommend being wary of those older kinds and mostly won’t be talking about them here.
Bioidentical hormones are safer: True or False?
True! This is an open-and-shut case:
❝Physiological data and clinical outcomes demonstrate that bioidentical hormones are associated with lower risks, including the risk of breast cancer and cardiovascular disease, and are more efficacious than their synthetic and animal-derived counterparts.
Until evidence is found to the contrary, bioidentical hormones remain the preferred method of HRT. ❞
Further research since that review has further backed up its findings.
Source: Are Bioidentical Hormones Safer or More Efficacious than Other Commonly Used Versions in HRT?
So simply, if you’re going on HRT (estrogen and/or progesterone), you might want to check it’s the bioidentical kind.
HRT can increase the risk of breast cancer: True or False?
Contingently True, but for most people, there is no significant increase in risk.
First: again, we’re talking bioidentical hormones, and in this case, estradiol. Older animal-derived attempts had much higher risks with much lesser efficaciousness.
There have been so many studies on this (alas, none that have been publicised enough to undo the bad PR in the wake of old-fashioned HRT from before the 70s), but here’s a systematic review that highlights some very important things:
❝Estradiol-only therapy carries no risk for breast cancer, while the breast cancer risk varies according to the type of progestogen.
Estradiol therapy combined with medroxyprogesterone, norethisterone and levonorgestrel related to an increased risk of breast cancer, estradiol therapy combined with dydrogesterone and progesterone carries no risk❞
In fewer words:
- Estradiol by itself: no increased risk of breast cancer
- Estradiol with MDPA or other progestogens that aren’t really progesterone: increased risk of breast cancer
- Estradiol with actual progesterone: back to no increased risk of breast cancer
So again, you might want to make sure you are getting actual bioidentical hormones, and not something else!
However! If you are aware that you already have an increased risk of breast cancer (e.g. family history, you’ve had it before, you know you have certain genes for it, etc), then you should certainly discuss that with your doctor, because your personal circumstances may be different:
❝Tailored HRT may be used without strong evidence of a deleterious effect after ovarian cancer, endometrial cancer, most other gynecological cancers, bowel cancer, melanoma, a family history of breast cancer, benign breast disease, in carriers of BRACA mutations, after breast cancer if adjuvant therapy is not being used, past thromboembolism, varicose veins, fibroids and past endometriosis.
Relative contraindications are existing cardiovascular and cerebrovascular disease and breast cancer being treated with adjuvant therapies❞
Source: HRT in difficult circumstances: are there any absolute contraindications?
HRT makes you happier, healthier, and smell nice too: True or False?
Contingently True, assuming you do want its effects, which generally means the restoration of much of the youthful vitality you enjoyed pre-menopause.
The “and smell nice too” was partly rhetorical, but also partly literal: our scent is largely informed by our hormones, and higher estrogen results in a sweeter scent; lower estrogen results in a more bitter scent. Not generally considered an important health matter, but it’s a thing, so hey.
More often, people take menopausal HRT for more energy, stronger bones (reduced osteoporosis risk), healthier heart (reduced CVD risk), improved sexual health, better mood, healthier skin and hair, and general avoidance of menopause symptoms:
Read more: Skin, hair and beyond: the impact of menopause
We’d need another whole main feature to discuss all the benefits properly; today we’re just mythbusting.
HRT does have some drawbacks: True or False?
True, and/but how serious they are (beyond the aforementioned consideration in the case of an already-increased risk of breast cancer) is a matter of opinion.
For example, it is common to get a reprise of monthly cramps and/or mood swings, depending on how one is taking the HRT and other factors (e.g. your own personal physiology and genetic predispositions). For most people, these will even out over time.
It’s also even common to get a reprise of (much slighter than before) monthly bleeding, unless you have for example had a hysterectomy (no uterus = no bleeding). Again, this will usually settle down in a matter of months.
If you experience anything more alarming than that, then indeed check with your doctor.
HRT is a dangerous scam and sham: True or False?
False, simply. As described above, for most people they’re quite safe. Again, talking bioidentical hormones.
The other kind are in the most neutral sense a sham (i.e. they are literally sham hormones), though they’re not without their merits and for many people they may be better than nothing.
As for being a scam, biodentical hormones are widely prescribed in the many countries that have universal healthcare and/or a single-payer healthcare system, where there would be no profit motive (and considerable cost) in doing so.
They’re prescribed because they are effective and thus reduce healthcare spending in other areas (such as treating osteoporosis or CVD after the fact) and improve Health Related Quality of Life, and by extension, health-adjusted life-years, which is one of the top-used metrics for such systems.
See for example:
Our apologies, gentlemen
We wanted to also talk about testosterone therapy for the andropause, but we’ve run out of room today (because of covering the important distinction of bioidentical vs old-fashioned HRT)!
To make it up to you, we’ll do a full main feature on it (it’s an interesting topic) in the near future, so watch this space
Ladies, we’ll also at some point cover the pros and cons of different means of administration, e.g. pills, transdermal gel, injections, patches, pessaries, etc—which often have big differences.
That’ll be in a while though, because we try to vary our topics, so we can’t talk about menopausal HRT all the time, fascinating and important a topic it is.
Meanwhile… take care, all!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Keep Warm (Without Sweat Patches!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I saw an advert on the subway for a pillow spray that guarantees a perfect night’s sleep. What does the science say about smells/sleep?❞
That is certainly a bold claim! Unless it’s contingent, e.g. “…or your money back”. Because otherwise, it absolutely cannot guarantee that.
There is some merit:
❝Odors can modulate the latency to sleep onset, as well as the quality and duration of sleep. Olfactory modulation of sleep may be mediated by direct synaptic interaction between the olfactory system and sleep control nuclei, and/or indirectly through odor modulation of arousal and respiration.
Such modulation appears most heavily influenced by past associations and expectations about the odor, beyond any potential direct physicochemical effect❞
Source: Reciprocal relationships between sleep and smell
Translating that from sciencese:
Sometimes we find pleasant smells relaxing, and placebo effect also helps.
That “any potential direct physiochemical effect”, though, when it does occur, is things like this…
Read: Odor blocking of stress hormone responses
…but that’s a mouse study, and those odors may only work to block three specific mouse stress responses to three specific stressors: physical restraint, predator odor, and male–male confrontation.
In other words: if, perchance, those three things are not what’s stressing you in bed at night (we won’t make assumptions), and/or you are not a mouse, it may not help.
(and this, dear readers, is why we must read articles, and not just headlines!)
But! If you are going to go for a pillow fragrance, something well-associated with being relaxing and soporific, such as lavender, is the way to go:
- Effects of aromatherapy on sleep quality and anxiety of patients
- Effects of Aromatherapy on the Anxiety, Vital Signs, and Sleep Quality of Percutaneous Coronary Intervention Patients in Intensive Care Units
- Effect of lavender aromatherapy on vital signs and perceived quality of sleep in the intermediate care unit: a pilot study
tl;dr = patients found lavender fragrances relaxing, experienced less anxiety, got better sleep (significantly or insignificantly, depending on the study) and enjoyed lower blood pressure (significantly or insignificantly, depending on the study).
PS: this writer uses a pillow spray like this one
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: