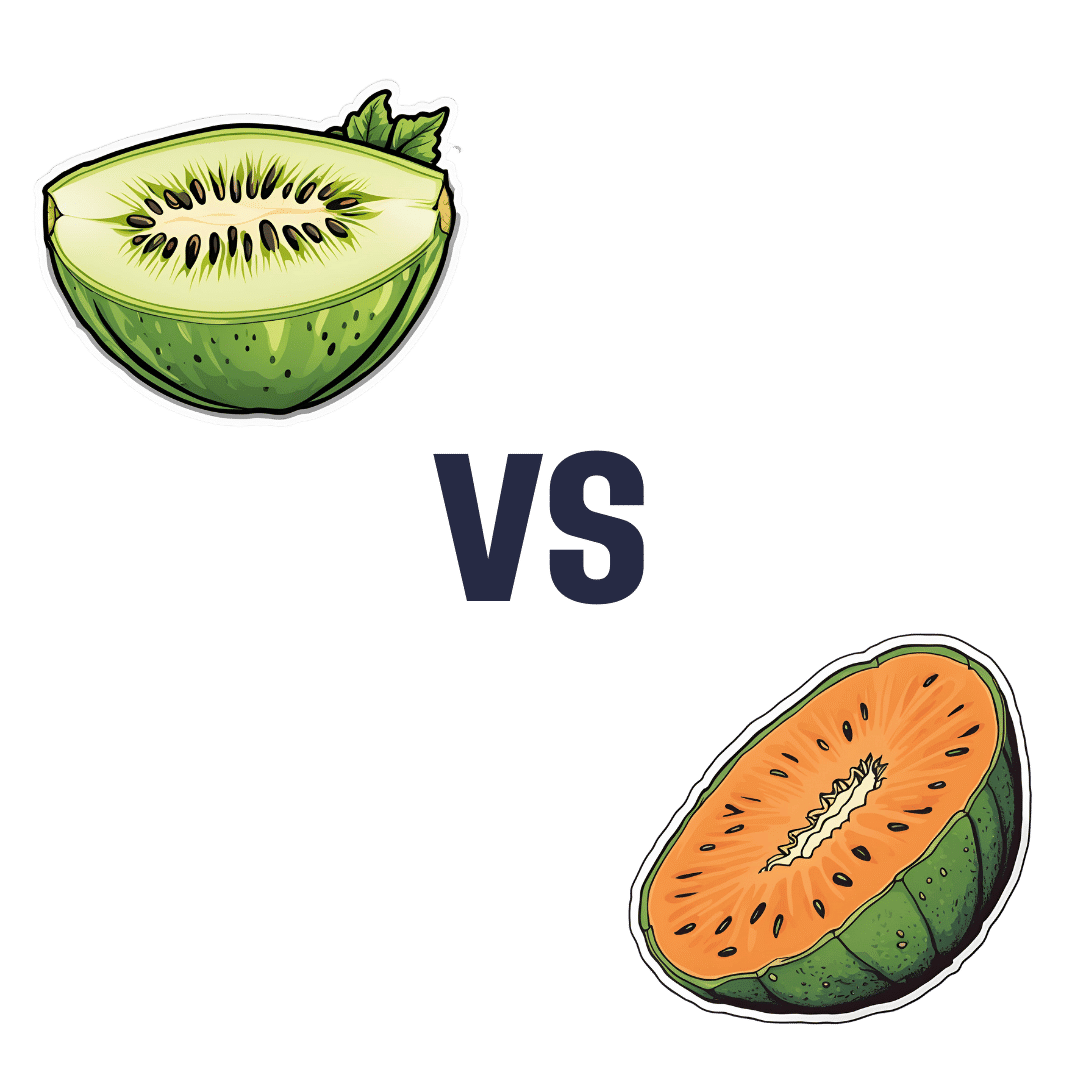
Honeydew vs Cantaloupe – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing honeydew to cantaloupe, we picked the cantaloupe.
Why?
In terms of macros, there’s not a lot between them—they’re both mostly water. Nominally, honeydew has more carbs while cantaloupe has more fiber and protein, but the differences are very small. So, a very slight win for cantaloupe.
Looking at vitamins: honeydew has slightly more of vitamins B5 and B6 (so, the vitamins that are in pretty much everything), while cantaloupe has a more of vitamins A, B1, B2, B3, C, and E (especially notably 67x more vitamin A, whence its color). A more convincing win for cantaloupe.
The minerals category is even more polarized: honeydew has more selenium (and for what it’s worth, more sodium too, though that’s not usually a plus for most of us in the industrialized world), while cantaloupe has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and zinc. An overwhelming win for cantaloupe.
No surprises: adding up the slight win for cantaloupe, the convincing win for cantaloupe, and the overwhelming win for cantaloupe, makes cantaloupe the overall best pick here.
Enjoy!
Want to learn more?
You might like to read:
From Apples to Bees, and High-Fructose Cs: Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
ADHD For Smart Ass Women – by Tracy Otsuka
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed books about ADHD in adults before, what makes this one different? It’s the wholly female focus. Which is not to say some things won’t apply to men too, they will.
But while most books assume a male default unless it’s “bikini zone” health issues, this one is written by a woman for women focusing on the (biological and social) differences in ADHD for us.
A strength of the book is that it neither seeks to:
- over-medicalize things in a way that any deviation from the norm is inherently bad and must be fixed, nor
- pretend that everything’s a bonus, that we are superpowered and beautiful and perfect and capable and have no faults that might ever need addressing actually
…instead, it gives a good explanation of the ins and outs of ADHD in women, the strengths and weaknesses that this brings, and good solid advice on how to play to the strengths and reduce (or at least work around) the weaknesses.
Bottom line: this book has been described as “ADHD 2.0 (a very popular book that we’ve reviewed previously), but for women”, and it deserves that.
Click here to check out ADHD for Smart Ass Women, and fall in love with your neurodivergent brain!
Share This Post
-
The Circadian Diabetes Code – by Dr. Satchin Panda
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We have previously reviewed Dr. Panda’s “The Circadian Code” which pertains to the circadian rhythms (yes, plural) in general; this one uses much of the same research, but with a strong focus on the implications for blood sugar management.
It’s first a primer in diabetes (and prediabetes, and, in contrast, what things should look like if healthy). You’ll understand about glucose metabolism and glycogen and insulin and more; you’ll understand what blood sugar readings mean, and you’ll know what an Hb1AC count actually is and what it should look like too, things like that.
After that, it’s indeed about what the subtitle promises: the right times to eat (and what to eat), when to exercise (and how, at which time), and how to optimize your sleep in the context of circadian rhythm and blood sugar management.
You may be wondering: why does circadian rhythm matter for blood sugars? And the answer is explained at some length in the first part of the book, but to oversimplify greatly: your body needs energy all the time, no matter when it was that you last ate. Thus, it has to organize its energy reserves to that at all times you can 1) function, on a cellular level 2) maintain a steady balance of sugar in your blood despite using it at slightly higher or lower levels at different times of day. Because the basal metabolic rate accounts for most of our energy use, the body has to plan for a base rate of so much energy per day, and to do that, it needs to know what a day is. Dr. Panda explains this in detail (the marvels of PER proteins and all that), but basically, that’s the relevance of circadian rhythm.
However, it’s not all theory and biochemistry; there is also a 12-week program to reverse prediabetes and type 2 diabetes (it will not, of course, reverse Type 1 Diabetes, sorry—but the program will still be beneficial even in that case, since more even blood sugars means fewer woes).
They style is friendly and clear, explaining the science simply, yet without patronizing the reader. References are given, with claims sourced in an extensive bibliography.
Bottom line: if you or a loved one have diabetes or prediabetes, or just have a strong desire to avoid getting such and generally keep your metabolic health in good order, this book will definitely help.
Click here to check out The Diabetes Code, and enjoy better blood sugar health than ever!
Share This Post
-
Junk Food Turns Public Villain as Power Shifts in Washington
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The new Trump administration could be coming for your snacks.
For years, the federal government has steered clear of regulating junk food, fast food, and ultra-processed food.
Now attitudes are changing. Some members of President-elect Donald Trump’s inner circle are gearing up to battle “Big Food,” or the companies that make most of the food and beverages consumed in the United States. Nominees for top health agencies are taking aim at ultra-processed foods that account for an estimated 70% of the nation’s food supply. Based on recent statements, a variety of potential politically charged policy options to regulate ultra-processed food may land on the Trump team menu, including warning labels, changes to agribusiness subsidies, and limits on which products consumers can buy with government food aid.
The push to reform the American diet is being driven largely by conservatives who have taken up the cause that has long been a darling of the left. Trump supporters such as Robert F. Kennedy Jr., whose controversial nomination to lead the Department of Health and Human Services still faces Senate confirmation, are embracing a concept that champions natural foods and alternative medicine. It’s a movement they’ve dubbed “MAHA,” or Make America Healthy Again. Their interest has created momentum because their goals have fairly broad bipartisan support even amid a bitterly divided Congress in which lawmakers from both sides of the aisle focused on the issue last year.
It’s likely to be a pitched battle because the food industry wields immense political influence and has successfully thwarted previous efforts to regulate its products or marketing. The category of “food processing and sales companies,” which includes Tyson Foods and Nestle SA, tallied $26.7 million in spending on lobbying in 2024, according to OpenSecrets. That’s up from almost $10 million in 1998.
“They have been absolutely instrumental and highly, highly successful at delaying any regulatory effectiveness in America,” said Laura Schmidt, a health policy professor at the University of California-San Francisco. “It really does feel like there needs to be a moment of reckoning here where people start asking the question, ‘Why do we have to live like this?’”
“Ultra-processed food” is a widely used term that means different things to different people and is used to describe items ranging from sodas to many frozen meals. These products often contain added fats, starches, and sugars, among other things. Researchers say consumption of ultra-processed foods is linked — in varying levels of intensity — to chronic conditions like diabetes, cancer, mental health problems, and early death.
Nutrition and health leaders are optimistic that a reckoning is already underway. Kennedy has pledged to remove processed foods from school lunches, restrict certain food additives such as dyes in cereal, and shift federal agricultural subsidies away from commodity crops widely used in ultra-processed foods.
The intensifying focus in Washington has triggered a new level of interest on the legal front as lawyers explore cases to take on major foodmakers for selling products they say result in chronic disease.
Bryce Martinez, now 18, filed a lawsuit in December against almost a dozen foodmakers such as Kraft Heinz, The Coca-Cola Co., and Nestle USA. He developed diabetes and non-alcoholic fatty liver disease by age 16, and is seeking to hold them accountable for his illnesses. According to the suit, filed in the Philadelphia Court of Common Pleas, the companies knew or should have known ultra-processed foods were harmful and addictive.
The lawsuit noted that Martinez grew up eating heavily advertised, brand-name foods that are staples of the American diet — sugary soft drinks, Cheerios and Lucky Charms, Skittles and Snickers, frozen and packaged dinners, just to name a few.
Nestle, Coca-Cola, and Kraft Heinz didn’t return emails seeking comment for this article. The Consumer Brands Association, a trade association for makers of consumer packaged goods, disputed the allegations.
“Attempting to classify foods as unhealthy simply because they are processed, or demonizing food by ignoring its full nutrient content, misleads consumers and exacerbates health disparities,” said Sarah Gallo, senior vice president of product policy, in a statement.
Other law firms are on the hunt for children or adults who believe they were harmed by consuming ultra-processed foods, increasing the likelihood of lawsuits.
One Indiana personal injury firm says on its website that “we are actively investigating ultra processed food (UPF) cases.” Trial attorneys in Texas also are looking into possible legal action against the federal regulators they say have failed to police ultra-processed foods.
“If you or your child have suffered health problems that your doctor has linked directly to the consumption of ultra-processed foods, we want to hear your story,” they say on their website.
Meanwhile, the FDA on Jan. 14 announced it is proposing to require a front-of-package label to appear on most packaged foods to make information about a food’s saturated fat, sodium, and added sugar content easily visible to consumers.
And on Capitol Hill, Sens. Bernie Sanders (I-Vt.), Ron Johnson (R-Wis.), and Cory Booker (D-N.J.) are sounding the alarm over ultra-processed food. Sanders introduced legislation in 2024 that could lead to a federal ban on junk food advertising to children, a national education campaign, and labels on ultra-processed foods that say the products aren’t recommended for children. Booker cosigned the legislation along with Sens. Peter Welch (D-Vt.) and John Hickenlooper (D-Colo.).
The Senate Committee on Health, Education, Labor and Pensions held a December hearing examining links between ultra-processed food and chronic disease during which FDA Commissioner Robert Califf called for more funding for research.
Food companies have tapped into “the same neural circuits that are involved in opioid addiction,” Califf said at the hearing.
Sanders, who presided over the hearing, said there’s “growing evidence” that “these foods are deliberately designed to be addictive,” and he asserted that ultra-processed foods have driven epidemics of diabetes and obesity, and hundreds of billions of dollars in medical expenses.
Research on food and addiction “has accumulated to the point where it’s reached a critical mass,” said Kelly Brownell, an emeritus professor at Stanford who is one of the editors of a scholarly handbook on the subject.
Attacks from three sides — lawyers, Congress, and the incoming Trump administration, all seemingly interested in taking up the fight — could lead to enough pressure to challenge Big Food and possibly spur better health outcomes in the U.S., which has the lowest life expectancy among high-income countries.
“Maybe getting rid of highly processed foods in some things could actually flip the switch pretty quickly in changing the percentage of the American public that are obese,” said Robert Redfield, a virologist who led the Centers for Disease Control and Prevention during the previous Trump administration, in remarks at a December event hosted by the Heritage Foundation, a conservative think tank.
Claims that Big Food knowingly manufactured and sold addictive and harmful products resemble the claims leveled against Big Tobacco before the landmark $206 billion settlement was reached in 1998.
“These companies allegedly use the tobacco industry’s playbook to target children, especially Black and Hispanic children, with integrated marketing tie-ins with cartoons, toys, and games, along with social media advertising,” Rene Rocha, one of the lawyers at Morgan & Morgan representing Martinez, told KFF Health News.
The 148-page Martinez lawsuit against foodmakers draws from documents made public in litigation against tobacco companies that owned some of the biggest brands in the food industry.
Similar allegations were made against opioid manufacturers, distributors, and retailers before they agreed to pay tens of billions of dollars in a 2021 settlement with states.
The FDA ultimately put restrictions on the labeling and marketing of tobacco, and the opioid epidemic led to legislation that increased access to lifesaving medications to treat addiction.
But the Trump administration’s zeal in taking on Big Food may face unique challenges.
The ability of the FDA to impose regulation is hampered in part by funding. While the agency’s drug division collects industry user fees, its division of food relies on a more limited budget determined by Congress.
Change can take time because the agency moves at what some critics call a glacial pace. Last year, the FDA revoked a regulation allowing brominated vegetable oil in food products. The agency determined in 1970 that the additive was not generally recognized as safe.
Efforts to curtail the marketing of ultra-processed food could spur lawsuits alleging that any restrictions violate commercial speech protected by the First Amendment. And Kennedy — if he is confirmed as HHS secretary — may struggle to get support from a Republican-led Congress that champions less federal regulation and a president-elect who during his previous term served fast food in the White House.
“The question is, will RFK be able to make a difference?” said David L. Katz, a doctor who founded True Health Initiative, a nonprofit group that combats public health misinformation. “No prior administration has done much in this space, and RFK is linked to a particularly anti-regulatory administration.”
Meanwhile, the U.S. population is recognized as among the most obese in the world and has the highest rate of people with multiple chronic conditions among high-income countries.
“There is a big grassroots effort out there because of how sick we are,” said Jerold Mande, who served as deputy undersecretary for food safety at the Department of Agriculture from 2009 to 2011. “A big part of it is people shouldn’t be this sick this young in their lives. You’re lucky if you get to 18 without a chronic disease. It’s remarkable.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
Brain Wash – by Dr. David Perlmutter, Dr. Austin Perlmutter, and Kristen Loberg
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may be familiar with the lead author of this book, Dr. David Perlmutter, as a big name in the world of preventative healthcare. A lot of his work has focused specifically on carbohydrate metabolism, and he is as associated with grains and he is with brains. This book focuses on the latter.
Dr. Perlmutter et al. take a methodical look at all that is ailing our brains in this modern world, and systematically lay out a plan for improving each aspect.
The advice is far from just dietary, though the chapter on diet takes a clear stance:
❝The food you eat and the beverages you drink change your emotions, your thoughts, and the way you perceive the world❞
The style is explanatory, and the book can be read comfortably as a “sit down and read it cover to cover” book; it’s an enjoyable, informative, and useful read.
Bottom line: if you’d like to give your brain a gentle overhaul, this is the one-stop-shop book to give you the tools to do just that.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Age Later – by Dr. Nir Barzilai
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Barzilai discusses why we age, why supercentenarians age more slowly, and even, why it is so often the case that supercentenarians outside of Blue Zones have poor lifestyles (their longevity is because of protective genes that mitigate the harmful effects of those poor lifestyles—the ultimate in “survivorship bias”).
He also talks not just genetics, but also epigenetics, and thus gene expression. Bearing in mind, there’s a scale of modifiability there: with current tech, we can’t easily change a bad gene… But we often can just switch it off (or at least downregulate its expression). This is where studies in supercentenarians are helpful even for those who don’t have such fortunate genes—the supercentenarian studies show us which genes we want on or off, what gene expressions to aim for, etc. Further clinical studies can then show us what lifestyle interventions (exercise, diet, nutraceuticals, etc) can do that for us.
With regard to those lifestyle interventions, he does cover many, and that’s where a lot of the practical value of the book comes from. But it’s not just “do this, do that”; understanding the reasons behind why things work the way they do is important, so as to be more likely to do it right, and also to enjoy greater adherence (we tend to do things we understand more readily than things we have just been told to do).
There are areas definitely within the author’s blind spots—for example, when talking about menopausal HRT, he discusses at great length the results of the discredited WHI study, and considers it the only study of relevance. So, this is a reminder to not believe everything said by someone who sounds confident (Dr. Barzilai’s professional background is mostly in treating diabetes).
In terms of style, it is very much narrative; somewhat pop-science, but more “this doctor wants to tell stories”. So many stories. Now, the stories all have informational value, so this isn’t padding, but it is the style, so we mention it as such. As for citations, there aren’t any, so if you want to look up the science he mentions, you’re going to need a bit of digital sleuthery to find the papers from the clues in the stories.
Bottom line: if you’re interested in the science of aging and how that has been progressing for the past decades and where we’re at, this book will give you so many jumping-off points, and is an engaging read.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Stop Using The Wrong Hairbrush For Your Hair Type
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When you brush your hair, you’re either making it healthier or damaging it, depending on what you’re using and how. To avoid pulling your hair out, and to enjoy healthy hair of whatever kind you have and whatever length suits you, it pays to know a little about different brushes, and the different techniques involved.
Head-to-head
Brush shapes and sizes are designed to achieve different effects in hair, not just for decoration. For example:
- Rat tail combs are excellent for parting and sectioning hair with clean lines. The rat tail part is actually more important than the comb part.
- Regular combs are multipurpose but best for use with flat irons, ensuring straighter hair for a longer time.
- Wide-tooth combs should not be used for detangling as they can cause breakage; instead, use a proper detangling brush. Speaking of detangling…
- Detangling brushes are essential for daily use. Whichever you use, start brushing from the bottom to prevent tangles from stacking and worsening. As for kinds of detangling brush:
- The “Tangle Teaser” is a good beginner option, but it may not detangle well for thicker hair.
- Wet Brush (this is a brand name, and is not about any inherent wetness) is the recommended detangling brush for most people. It can be used on wet or dry hair.
- Mason Pearson brush is a luxury detangling brush (see it here on Amazon) that works slightly more quickly and efficiently, but is expensive and not necessary for most people.
- Teasing brushes are for adding volume by backcombing—but require skill to prevent visible tangles. Best avoided for most people.
- Ceramic round brushes are the best for blow-drying, because they hold tension and help hair dry smoother and shinier.
- Blow-dryer brushes are great for easy blow-drying but should not be used on dry hair, to avoid damage.
- Denman brushes are for people with natural curls, enhancing curls without straightening them like a Wet brush would.
For more on all of these brushes, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: