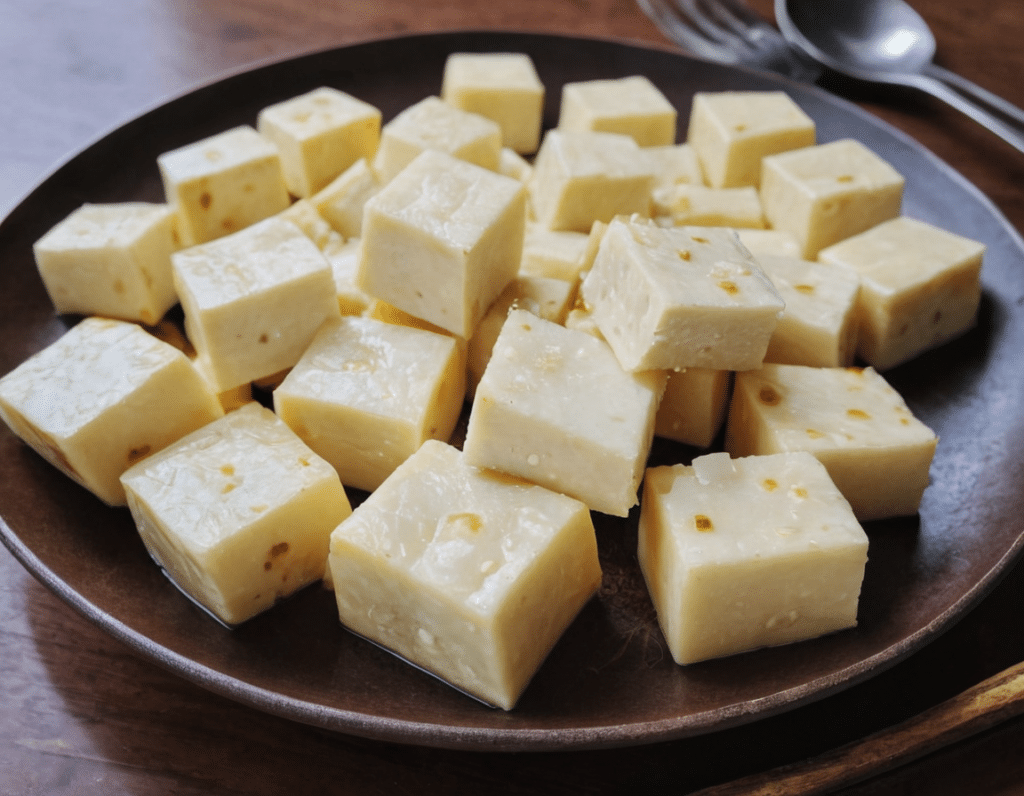
High-Protein Paneer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Paneer (a kind of Desi cheese used in many recipes from that region) is traditionally very high in fat, mostly saturated. Which is delicious, but not exactly the most healthy.
Today we’ll be making a plant-based paneer that does exactly the same jobs (has a similar texture and gentle flavor, takes on the flavors of dishes in the same way, etc) but with a fraction of the fat (of which only a trace amount is saturated, in this plant-based version), and even more protein. We’ll use this paneer in some recipes in the future, but it can be enjoyed by itself already, so let’s get going…
You will need
- ½ cup gram flour (unwhitened chickpea flour)
- Optional: 1 tsp low-sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Whisk the flour (and salt, if using) with 2 cups water in a big bowl, whisking until the texture is smooth.
2) Transfer to a large saucepan on a low-to-medium heat; you want it hot, but not quite a simmer. Keep whisking until the mixture becomes thick like polenta. This should take 10–15 minutes, so consider having someone else to take shifts if the idea of whisking continually for that long isn’t reasonable to you.
3) Transfer to a non-stick baking tin that will allow you to pour it about ½” deep. If the tin’s too large, you can always use a spatula to push it up against two or three sides, so that it’s the right depth
3) Refrigerate for at least 10 minutes, but longer is better if you have the time.
4) When ready to serve/use, cut it into ½” cubes. These can be served/used now, or kept for about a week in the fridge.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Quercetin Quinoa Probiotic Salad
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This quercetin-rich salad is a bit like a tabbouleh in feel, with half of the ingredients switched out to maximize phenolic and gut-healthy benefits.
You will need
- ½ cup quinoa
- ½ cup kale, finely chopped
- ½ cup flat leaf parsley, finely chopped
- ½ cup green olives, thinly sliced
- ½ cup sun-dried tomatoes, roughly chopped
- 1 pomegranate, peel and pith removed
- 1 preserved lemon, finely chopped
- 1 oz feta cheese or plant-based equivalent, crumbled
- 1 tsp black pepper, coarse ground
- 1 tbsp capers
- 1 tbsp chia seeds
- 1 tbsp extra virgin olive oil
Note: you shouldn’t need salt or similar here, because of the diverse gut-healthy fermented products bringing their own salt with them
Method
(we suggest you read everything at least once before doing anything)
1) Rinse the quinoa, add the tbsp of chia seeds, cook as normal for quinoa (i.e. add hot water, bring to boil, simmer for 15 minutes or so until pearly and tender), carefully (don’t lose the chia seeds; use a sieve) drain and rinse with cold water to cool. Shake off excess water and/or pat dry on kitchen paper if necessary.
2) Mix everything gently but thoroughly.
3) Serve:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Tasty Tabbouleh with Tahini ← in case you want an actual tabbouleh
- Making Friends With Your Gut (You Can Thank Us Later)
- Fight Inflammation & Protect Your Brain, With Quercetin
Take care!
Share This Post
-
How they did it: STAT reporters expose how ailing seniors suffer when Medicare Advantage plans use algorithms to deny care
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In a call with a long-time source, what stood out most to STAT reporters Bob Herman and Casey Ross was just how viscerally frustrated and angry the source was about an algorithm used by insurance companies to decide how long patients should stay in a nursing home or rehab facility before being sent home.
The STAT stories had a far-reaching impact:
- The U.S. Senate Committee on Homeland Security and Government Affairs took a rare step of launching a formal investigation into the use of algorithms by the country’s three largest Medicare Advantage insurers.
- Thirty-two House members urged the Centers for Medicare and Medicaid Services to increase the oversight of algorithms that health insurers use to make coverage decisions.
- In a rare step, CMS launched its own investigation into UnitedHealth. It also stiffened its regulations on the use of proprietary algorithms and introduced plans to audit denials across Medicare Advantage plans in 2024.
- Based on STAT’s reporting, Medicare Advantage beneficiaries filed two class-action lawsuits against UnitedHealth and its NaviHealth subsidiary, the maker of the algorithm, and against Humana, another major health insurance company that was also using the algorithm.
- Amid scrutiny, UnitedHealth renamed NaviHealth.
The companies never allowed an on-the-record interview with their executives, but they acknowledged that STAT’s reporting was true, according to the news organization.
Ross and Herman spoke with The Journalist’s Resource about their project and shared the following eight tips.
1. Search public comments on proposed federal rules to find sources.
Herman and Ross knew that the Centers for Medicare and Medicaid Services had put out a request for public comments, asking stakeholders within the Medicare Advantage industry how the system could improve.
There are two main ways to get Medicare coverage: original Medicare, which is a fee-for-service health plan, and Medicare Advantage, which is a type of Medicare health plan offered by private insurance companies that contract with Medicare. Medicare Advantage plans have increasingly become popular in recent years.
Under the Social Security Act, the public has the opportunity to submit comments on Medicare’s proposed national coverage determinations. CMS uses public comments to inform its proposed and final decisions. It responds in detail to all public comments when issuing a final decision.
The reporters began combing through hundreds of public comments attached to a proposed Medicare Advantage rule that was undergoing federal review. NaviHealth, the UnitedHealth subsidiary and the maker of the algorithm, came up in many of the comments, which include the submitters’ information.
“These are screaming all-caps comments to federal regulators about YOU NEED TO SOMETHING ABOUT THIS BECAUSE IT’S DISGUSTING,” Ross says.
“The federal government is proposing rules and regulations all the time,” adds Herman, STAT’s business of health care reporter. “If someone’s going to take the time and effort to comment on them, they must have at least some knowledge of what’s going on. It’s just a great tool for any journalist to use to figure out more and who to contact.”
The reporters also found several attorneys who had complained in the comments. They began reaching out to them, eventually gaining access to confidential documents and intermediaries who put them in touch with patients to show the human impact of the algorithm.
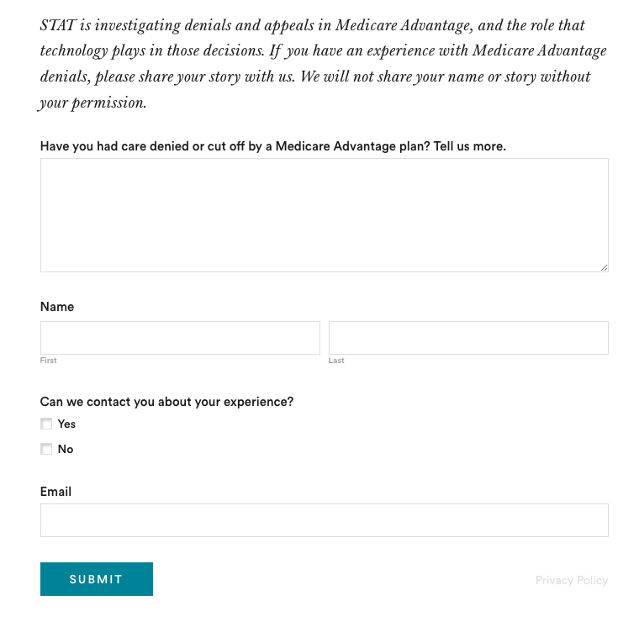
2. Harness the power of the reader submission box.
At the suggestion of an editor, the reporters added a reader submission box at the bottom of their first story, asking them to share their own experiences with Medicare Advantage denials.
The floodgates opened. Hundreds of submissions arrived.
By the end of their first story, Herman and Ross had confidential records and some patients, but they had no internal sources in the companies they were investigating, including Navihealth. The submission box led them to their first internal source.
(Screenshot of STAT’s submission box.) The journalists also combed through LinkedIn and reached out to former and current employees, but the response rate was much lower than what they received via the submission box.
The submission box “is just right there,” Herman says. “People who would want to reach out to us can do it right then and there after they read the story and it’s fresh in their minds.”
3. Mine podcasts relevant to your story.
The reporters weren’t sure if they could get interviews with some of the key figures in the story, including Tom Scully, the former head of the Centers for Medicare and Medicaid Services who drew up the initial plans for NaviHealth years before UnitedHealth acquired it.
But Herman and another colleague had written previously about Scully’s private equity firm and they had found a podcast where he talked about his work. So Herman went back to the podcast — where he discovered Scully had also discussed NaviHealth.
The reporters also used the podcast to get Scully on the phone for an interview.
“So we knew we had a good jumping off point there to be like, ‘OK, you’ve talked about NaviHealth on a podcast, let’s talk about this,’” Herman says. “I think that helped make him more willing to speak with us.”
4. When covering AI initiatives, proceed with caution.
“A source of mine once said to me, ‘AI is not magic,’” Ross says. “People need to just ask questions about it because AI has this aura about it that it’s objective, that it’s accurate, that it’s unquestionable, that it never fails. And that is not true.”
AI is not a neutral, objective machine, Ross says. “It’s based on data that’s fed into it and people need to ask questions about that data.”
He suggests several questions to ask about the data behind AI tools:
- Where does the data come from?
- Who does it represent?
- How is this tool being applied?
- Do the people to whom the tool is being applied match the data on which it was trained? “If racial groups or genders or age of economic situations are not adequately represented in the training set, then there can be an awful lot of bias in the output of the tool and how it’s applied,” Ross says.
- How is the tool applied within the institution? Are people being forced to forsake their judgment and their own ability to do their jobs to follow the algorithm?
5. Localize the story.
More than half of all Medicare beneficiaries have Medicare Advantage and there’s a high likelihood that there are multiple Medicare Advantage plans in every county across the nation.
“So it’s worth looking to see how Medicare Advantage plans are growing in your area,” Herman says.
Finding out about AI use will most likely rely on shoe-leather reporting of speaking with providers, nursing homes and rehab facilities, attorneys and patients in your community, he says. Another source is home health agencies, which may be caring for patients who were kicked out of nursing homes and rehab facilities too soon because of a decision by an algorithm.
The anecdote that opens their first story involves a small regional health insurer in Wisconsin, which was using NaviHealth and a contractor to manage post-acute care services, Ross says.
“It’s happening to people in small communities who have no idea that this insurer they’ve signed up with is using this tool made by this other company that operates nationally,” Ross says.
There are also plenty of other companies like NaviHealth that are being used by Medicare Advantage plans, Herman says. “So it’s understanding which Medicare Advantage plans are being sold in your area and then which post-acute management companies they’re using,” he adds.
Some regional insurers have online documents that show which contractors they use to evaluate post-acute care services.
6. Get familiar with Medicare’s appeals databases
Medicare beneficiaries can contest Medicare Advantage denials through a five-stage process, which can last months to years. The appeals can be filed via the Office of Medicare Hearings and Appeals.
“Between 2020 and 2022, the number of appeals filed to contest Medicare Advantage denials shot up 58%, with nearly 150,000 requests to review a denial filed in 2022, according to a federal database,” Ross and Herman write in their first story. “Federal records show most denials for skilled nursing care are eventually overturned, either by the plan itself or an independent body that adjudicates Medicare appeals.”
There are several sources to find appeals data. Be mindful that the cases themselves are not public to protect patient privacy, but you can find the number of appeals filed and the rationale for decisions.
CMS has two quality improvement organizations, or QIOs, Livanta and Kepro, which are required to file free, publicly-available annual reports, about the cases they handle, Ross says.
Another company, Maximus, a Quality Improvement Contractor, also files reports on prior authorization cases it adjudicates for Medicare. The free annual reports include data on raw numbers of cases and basic information about the percentage denials either overturned or upheld on appeal, Ross explains.
CMS also maintains its own database on appeals for Medicare Part C (Medicare Advantage plans) and Part D, which covers prescription drugs, although the data is not complete, Ross explains.
7. Give your editor regular updates.
“Sprinkle the breadcrumbs in front of your editors,” Ross says.
“If you wrap your editors in the process, you’re more likely to be able to get to the end of [the story] before they say, ‘That’s it! Give me your copy,’” Ross says.
8. Get that first story out.
“You don’t have to know everything before you write that first story,” Ross says. “Because with that first story, if it has credibility and it resonates with people, sources will come forward and sources will continue to come forward.”
Read the stories
Denied by AI: How Medicare Advantage plans use algorithms to cut off care for seniors in need
UnitedHealth pushed employees to follow an algorithm to cut off Medicare patients’ rehab care
UnitedHealth used secret rules to restrict rehab care for seriously ill Medicare Advantage patients
This article first appeared on The Journalist’s Resource and is republished here under a Creative Commons license.
Share This Post
-
Exercises for Sciatica Pain Relief
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Jessica Valant is a physiotherapist and Pilates teacher, and today she’s going to demonstrate some exercise that relieve (and also correct the cause of) sciatica pain.
Back to good health
You will need a large strap for one of these exercises; a Pilates strap is great, but you can also use a towel. The exercises are:
Pelvic Rocking Exercise:
- Lie on your back, feet flat, knees bent.
- Gently rock your pelvis forwards and backwards (50% effort, no glute squeezing).
Leg Stretch with Strap:
- Straighten your left leg and loop the strap around the ball of your right foot.
- Gently straighten and bend your right leg while holding the strap.
- Perform a “nerve glide” by flexing and pointing your foot (not a stretch, just gentle movement).
- Repeat on the left leg.
Piriformis Stretch:
- Bend your right knee and place your left ankle over it (figure-four position).
- For a deeper stretch, hold your right thigh and pull your legs inwards.
Lower Back Release:
- Let your legs fall gently to one side after stretching each leg, opening the lower back.
Back Extension:
- Lie on your belly, placing your elbows down, palms flat.
- Optional: push up slightly into a back bend if it feels comfortable.
Seated Stretching:
- Finish by sitting cross-legged or on a chair.
- Inhale while raising your arms up, exhale while lowering them down, then reach sideways with your arms to stretch.
- Perform gentle neck stretches by tilting your ear to your shoulder on each side.
She recommends doing these exercises daily for at least a few weeks, though you should start to see improvement in your symptoms immediately. Nothing here should cause a problem or make things worse, but if it does, stop immediately and consult a local physiotherapist for more personalized advice.
For more on all of this, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
6 Ways To Look After Your Back
Take care!
Share This Post
Related Posts
-
Caffeine: Cognitive Enhancer Or Brain-Wrecker?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Two Sides Of Caffeine
We asked you for your health-related opinions on caffeine itself, not necessarily the coffee, tea, energy drinks, etc that might contain it.
We have, by the way previously written about the health effects of coffee and tea specifically:
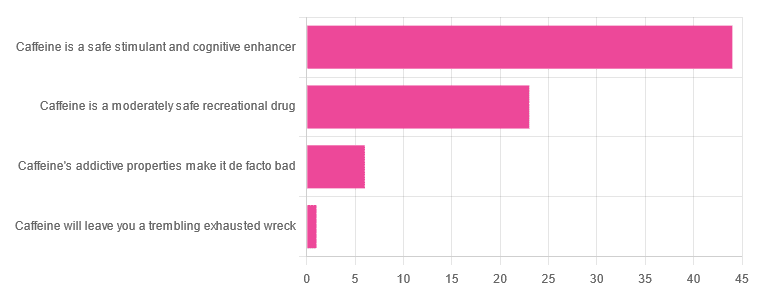
As for our question about caffeine itself, though, we got the above-depicted, below-described, set of results:
- About 59% said “caffeine is a safe stimulant and cognitive enhancer”
- About 31% said “caffeine is a moderately safe recreational drug”
- About 8% said “caffeine’s addictive properties make it de facto bad”
- One (1) person said “caffeine will leave you a trembling exhausted wreck”
But what does the science say?
Caffeine is addictive: True or False?
True, though one will find occasional academics quibbling the definition. Most of the studies into the mechanisms of caffeine addiction have been conducted on rats, but human studies exist too and caffeine is generally considered addictive for humans, for example:
See also:
Notwithstanding its addictive status, caffeine is otherwise safe: True or False?
True-ish, for most people. Some people with heart conditions or a hypersensitivity to caffeine may find it is not safe for them at all, and for the rest of us, the dose makes the poison. For example:
❝Can too much caffeine kill you? Although quite rare, caffeine can be fatal in cases of overdose; such circumstances are generally not applicable to healthy individuals who typically consume caffeine via beverages such as tea or coffee.❞
this paper, by the way, also includes a good example of academics quibbling the definition of addiction!
Caffeine is a cognitive enhancer: True or False?
True, but only in the case of occasional use. If you are using it all the time, your physiology will normalize it and you will require caffeine in order to function at your normal level. To attain higher than that, once addicted to caffeine, would now require something else.
Read more: Caffeine: benefits and drawbacks for technical performance
Caffeine will leave you a trembling exhausted wreck: True or False?
True or False depending on usage:
- The famously moderate 3–5 cups per day will not, for most people, cause any such problems.
- Using/abusing it to make up for lost sleep (or some other source of fatigue, such as physical exhaustion from exertion), however, is much more likely to run into problems.
In the latter case, caffeine really is the “payday loan” of energy! It’ll give you an adrenal boost now (in return, you must suffer the adrenal dumping later, along with lost energy expended in the adrenaline surge), and also, the tiredness that you thought was gone, was just caffeine’s adenosine-blocking activities temporarily preventing you from being able to perceive the tiredness. So you’ll have to pay that back later, with interest, because of the extra time/exertion too.
Want to make caffeine a little more gentle on your system?
Taking l-theanine alongside caffeine can ameliorate some of caffeine’s less wonderful effects—and as a bonus, l-theanine has some nifty benefits of its own, too:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
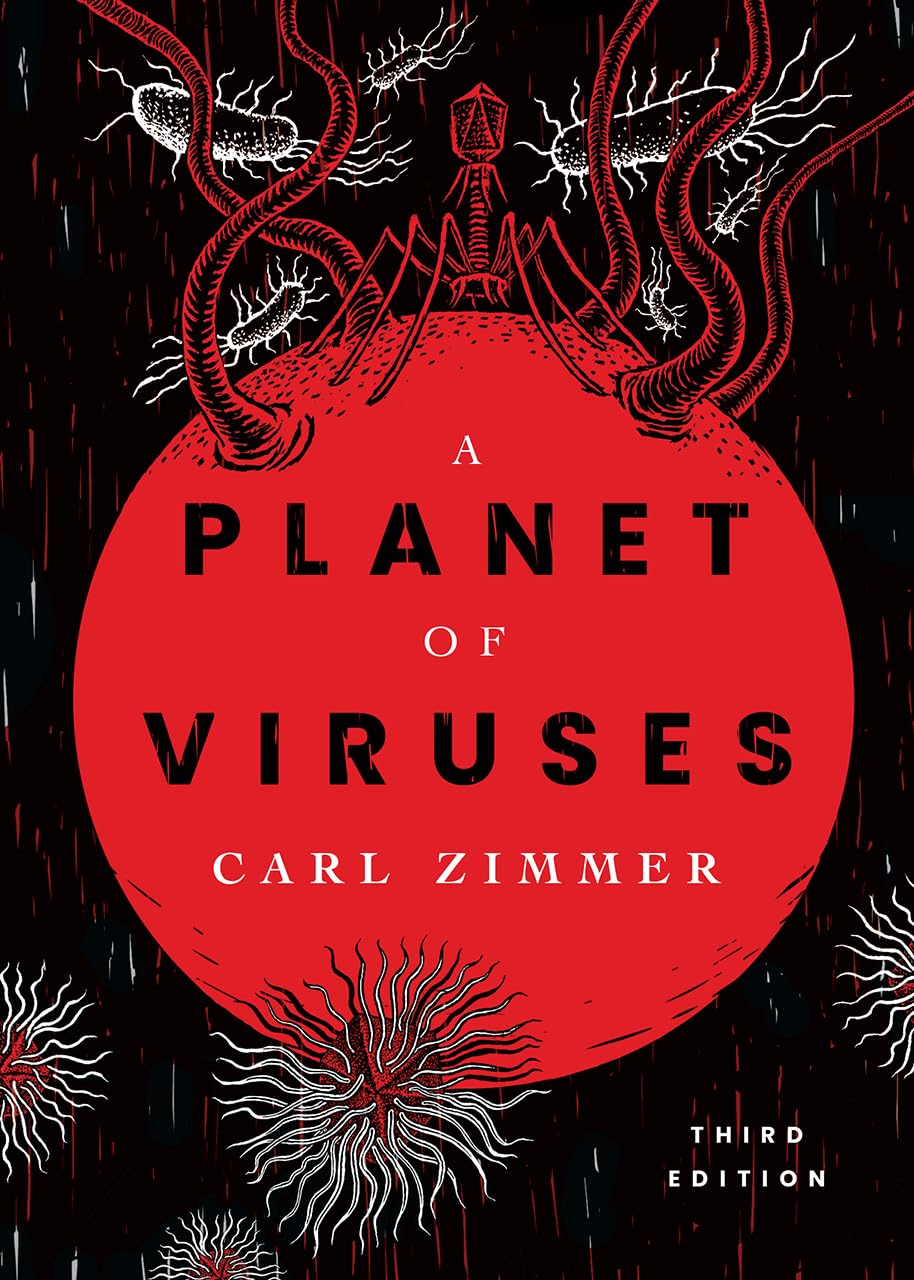
A Planet of Viruses – by Carl Zimmer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed numerous books on the immune system before, and this one’s mostly not about that.
Instead, this one focuses on the viruses themselves, and the part they play in our world, for good and for ill. Popular awareness tends to focus on the ill, of course.
But, there’s a lot that viruses do for us too, including:
- Weak/harmless viruses that keep our immune systems on their toes and ready
- Bacteriophage viruses that kill and consume pathogens that, left unchecked, would do the same to us
- Endogenous retroviruses that have become symbiotic with the human organism, without which our species would quickly go extinct
He also talks about biological warfare, and how we cannot bury our heads in the sand by avoiding research on those grounds, because someone will always do it anyway, so (as the motto of the immune system itself might say), best to be prepared.
The author is a science journalist, by the way, and has no PhD, but does have a flock of Fellowships and assorted scientific awards and honors, so he appears to be doing good work so far as the scientific community is concerned.
Bottom line: if you’d like to know more about viruses than “they’re very small and can cause harm”, then this book will open a whole new world.
Click here to check out A Planet of Viruses, and upgrade your knowledge!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
7 Signs of Undiagnosed Autism in Adults
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to adults and autism, there are two kinds of person in the popular view: those who resemble the Rain Man, and those who are making it up. But, it’s not so, as Paul Micallef explains:
The signs
We’ll not keep them a mystery; they are:
- Social interaction difficulties: such a person may struggle with understanding social cues, leading to awkwardness, isolation, or appearing eccentric.
- Need for structure and routine: either highly structured or disorganized, both of which stem from executive function challenges. The former, of course, is a coping mechanism, while the latter is the absence of same.
- Sensory sensitivities: can include sensitivities or insensitivities to light, sound, temperature, smells, tastes, and so forth.
- Spiky skillset: extreme strengths in certain areas, coupled with significant difficulties in others, leading to uneven abilities. May be able to dismantle and rebuild a PC, while not knowing how to arrange an Über.
- Emotional regulation issues: experiences of meltdowns, shutdowns, or withdrawal as coping mechanisms when overwhelmed. Not that this is “or”, not necessarily “and”. The latter goes especially unnoticed as an emotional regulation issue, because for everyone else, it’s something that’s not there to see.
- Unusual associations: making mental connections or associations that seem random or uncommon compared to others. The mind went to 17 places quickly and while everyone else got from idea A to idea B, this person is already at idea Q.
- Being “just different”: a general sense of being the odd one out, standing out in subtle or distinct ways. This is rather a catch-all, but if there’s someone who fits this, there’s a good chance, the other things apply too.
For more on all of these, whether pertaining to yourself or a loved one (or both!), enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- 16 Overlooked Autistic Traits In Women
- What is AuDHD? 5 important things to know when someone has both autism and ADHD
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: